Abstract
Alcohol is a psychoactive compound produced when sugar (carbohydrate) in grains; fruits and vegetables are fermented anaerobically by yeast or bacteria converting the glucose to alcohol and carbondioxide. Alcohol is a source of energy for humans supplying 7 kcal per gramme; but the calories are empty i.e.; devoid of other essential nutrients. It is readily absorbed into the blood from different segments of the gastrointestinal tract by simple diffusion. Alcohol is metabolized mainly in the liver by three enzyme systems which include Alcohol Dehydrogenase (ADH); Microsomal Ethanol Oxidizing System (MEOS) and catalase. Alcohol causes significant damage to the liver and brain cells leading to their death. It erodes the gastrointestinal tract and reduces enzyme and bile output thereby making digestion and absorption of nutrients difficult. Alcohol diminishes thiamin absorption and increases its excretion. Vitamin K deficiency in alcoholism may arise when there is an interruption of fat absorption due to pancreatic insufficiency; biliary obstruction; or intestinal mucosal abnormalities secondary to folate deficiency. The recommended intake of alcohol is two units per day for men and one drink per day for women. Excess alcohol intake above the recommended intake not only has serious physiological effects on the body but also leads to emotional disturbances and social violence.
KeywordsAlcohol; Metabolism; Nutrients; Organs; Damage; Intake
Introductıon
Alcohol is a class of organic compounds containing Hydroxyl (OH) groups [1]. It is an organic compound composed of carbon; oxygen; and hydrogen with the chemical formular C2H5OH. It is a psychoactive compound produced when sugar (carbohydrate) in grains; fruits and vegetables is fermented anaerobically by yeast or bacteria converting the glucose to alcohol and carbon dioxide. It is a source of energy for humans supplying 7kcal per gramme; but the calories are “empty” (i.e.; devoid of beneficial nutrients) [2]. According to Gropper et al. [3]; ethanol may account for up to 10% of total energy intakes of moderate consumers and up to 50% for alcoholics. Bennet et al. [4] stated that variations in drinking patterns include the type of beverages consumed preferentially; occasions on which consumption typical occurs; drinking levels that are considered normal and population subgroups for whom drinking is considered acceptable. The 2016 Global burden of disease [5] study estimated that Nigeria was one of the countries with the highest prevalence of current alcohol use among adults 15 years and older in Sub-Saharan Africa (SSA); 40 to 59.9% at a population level; for both males and females.
Metabolism of alcohol
From the moment an alcoholic beverage enters the body; it is treated as if it has special privileges [1]. It is transported unaltered in the blood stream and then oxidatively degraded in tissues; primarily the liver; first to acetaldehyde and then to acetate [3]. Alcohol is readily absorbed into the blood from different segments of the gastrointestinal tract by simple diffusion. About 20% of ingested alcohol is absorbed directly across the walls of an empty stomach and can reach the brain within a minute [1]. Food slows the gastric emptying time and stimulates secretions such as gastric acid; which dilutes the alcohol and slow its absorption. Metabolism of alcohol is dependent on numerous factors such as gender; race; size; physical conditions; what is eaten; the alcohol content of the beverage and even how much sleep one has had [2]. A woman cannot metabolism much alcohol in the cells that line her stomach because of low activity of the enzyme; Alcohol Dehydrogenase (ADH) [6]. Whitney and Rolfes [1] reported that women produce less of the enzymes ADH than men consequently; more alcohol reaches the intestine for absorption into the blood stream. Women seem to merit a lower limit for safe drinking because of their smaller size; greater proportion of body fat and slower metabolism of alcohol in the stomach [7].
In addition; research shows that different peoples carry different variations of the ADH and ALDH (Acetaldehyde Dehydrogenase) enzymes [8]. Some of these enzyme variants work efficiently than others; this means that some people can breakdown alcohol to acetaldehyde or acetaldehyde to acetate more quickly than others. The types of ADH and ALDH an individual carry has been shown to influence how much he or she drinks which in turn influences his or risk of developing alcoholism [9]. ADH enzymes present in the liver varies with individual depending on the genes they have inherited and on how recently they have eaten. Fasting as little as a day forces the body to degrade its proteins including the alcohol-processing enzymes and this can also slow the rate of alcohol metabolism by half [1].
Gropper et al. [3] explained that at least three enzyme systems
are capable of ethanol oxidation. They include;
• Alcohol Dehydrogenase (ADH).
• The Microsomal Ethanol Oxidizing System (MEOS) also
known as the cytochrome P.450 system.
• Catalase (in the presence of Hydrogen Perioxode (H2O2)).
Alcohol Dehydrogenase (ADH)
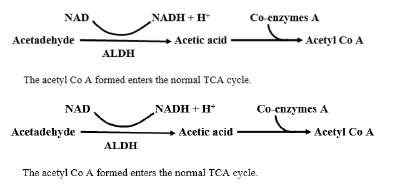
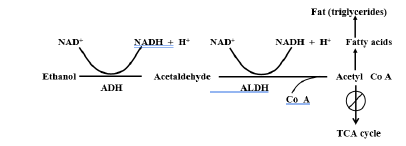
The Alcohol Dehydrogenase (ADH) is a soluble enzyme functioning in the cytoplasm of cells. It is an ordinary nicotinamide adenine Dinudeotide (NAD+) requiring dehydrogenase [3]. Alcohol at low to moderate quality is converted to acetaldehyde by the action of ADH (which requires zinc for its activity) and the coenzyme NAD [2]. The NAD (oxidized coenzyme form of niacin) picks up two hydrogens from the alcohol to form NADH + H (reduced form) and produces the intermediate product; acetaldehyde.
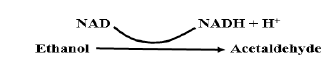
Acetaldehyde is a highly unstable compound that quickly forms free radial structures which are highly toxic if not quenched by antioxidants. Edenberg [10] stated that acetaldehyde is a highly toxic substance and a known carcinogen. The acetaldehyde formed is then converted to acetyl – Co A again yielding NADH + H+ with the aid of acetaldehyde dehydrogenase and co-enzyme A. The B vitamin; niacin; (in its role as the coenzyme NAD) helpfully picks up these hydrogen ions (becoming NADH) [1]. Thus; whenever the body breaks down alcohol NAD diminishes and NADH accumulates.
Microsomal Ethanol Oxidizing System (MEOS)
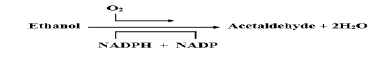
The ADH pathway cannot keep up with the demands to metabolize moderate to excessive levels of alcohol into acetaldehyde [2]. As a result; another enzyme system; MEOS; exists to metabolize the excess alcohol. Despite its name; the microsomal ethanol oxidizing system can oxidize a wide variety of compound in addition to ethanol; including fatty acids; aromatic hydrocarbon; steroids and barbiturate drugs [3]. Ethanol oxidation by the MEOS is linked to the simultaneous oxidation of NADPH (nicotinamide adenine dinucleotide phosphate (reduced form)) by molecular oxygen. One oxygen atom from the oxygen molecule is used to oxidize NADPH to NADP and the second atom oxidizes ethanol substrate to acetaldehyde. Both oxygen atoms are reduced to water; therefore, two water molecules are formed in this reaction [3].
According to Gropper et al. [3]; an important feature of the MEOS is that some of its enzymes; including the cytochrome P-450 units are inducible by ethanol particularly at higher concentrations and can induce the synthesis of these substances. The result is that the hepatocytes can metabolize ethanol much more effectively; thereby establishing a state of metabolic tolerance. Compared with a normal (non-drinking or light drinking) subject; an individual in a state of metabolic tolerance to ethanol can ingest larger quantities of the substance before showing the effects of intoxication.
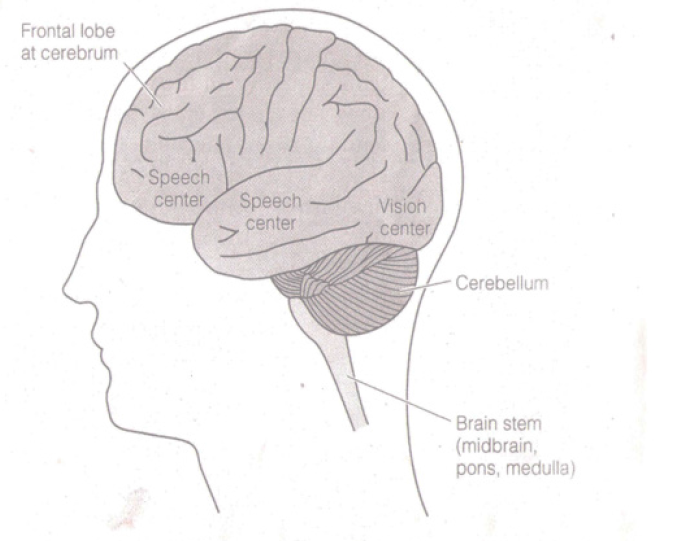
Effect of alcohol on the brain. Source: Whitney and Rolfes (1).
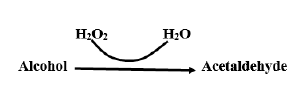
Catalase (in the presence of hydrogen peroxide (H2O2)):
The catalase system found in the liver is a minor pathway for metabolizing alcohol [3]. It is in the peroxisomes of the cell [6]. The catalase H2O2 system is the least active probably accounting for less than 2% of in vivo ethanol oxidation [3]. The catalase is heme iron dependent and is found mostly in cell peroxisomes (cytoplasmic organelles where lots of H2O2 are produced during oxidation of compounds example very long chain (20 carbon) fatty acids among other molecules). The catalase system metabolizes ethanol when sufficient H2O2 is available without requiring NAD as a co factor. It also yields acetaldehyde.
Metabolic Alternations in Alcoholism
Acetaldehyde Toxicity.
Both the ADH and MEOS routes of ethanol oxidation produce acetaldehyde which is believed to exert direct adverse effects on metabolic systems [3]. Gropper et al. [3] also explained that acetaldehyde has been shown to impede the formation of microtubules in liver cells and to cause the development of perivenular fibrosis. Either of which is believed to initiate the events leading to cirrhosis. Although acetaldehyde is short lived; usually existing in the body for a brief time before it is broken down into acetate; it has the potential to cause significant damage [8]. This is particularly evident in the liver; where the bulk of alcohol metabolism takes place [11]. In addition to its toxic effects; some researchers believed that acetaldehyde may be responsible for some of the behavioral and physiological effects previously attributed to alcohol [12]. For example; when acetaldehyde is administered to lab animals; it leads to in-coordination; memory impairment and sleepiness associated with alcohol [13].
It was once thought that alcoholic cirrhosis was caused by malnutrition; as the drinker satisfied his or her caloric needs with the empty calories of alcohol at the expense of a nutritionally adequate diet. In view of the effect of high levels of acetaldehyde on hepatocyte structure and function; however; it is now known that chronic overindulgence can cause cirrhosis in the absence of nutritional deficiency and even when alcohol is co ingested with an enriched diet.
High NADH: NAD+ Ratio
The oxidation of ethanol increases the concentration of NADH at the expense of NAD+ thereby elevating the NADH: NAD+ ratio [3]. This is because ADH and ALDH use NAD as co-substrate. During alcohol metabolism the multitude of other metabolic processes for which NAD is required including glycoclysis; the TCA (Tricarboxylic Acid) cycle and the electron transport chain falter [1]. Whitney and Rolfes [1] went further and explained that acetyl Co A molecules are blocked from getting into the TCA cycle by the high level of NADH. Instead of used for energy; the acetyl Co A molecules become building blocks for fatty acids.
The accumulation of hydrogen ions during alcohol metabolism
shifts the body’s acid base balance towards acid. Excess NADH
also promotes the production of lactic acid from pyruvate. The
conversion of pyruvate to lactic acid uses the hydrogen from
NADH and restores some NAD; but a lactic acid build up has
serious consequences of its own – it adds still further to the body’s
acid burden and interferes with the excretion of another acid; uric
acid; causing inflammation of the joints [1].
Pyruvate + NADH +H → Lactate + NAD
In the absence of NAD; lipids accumulate in most tissues in which ethanol are metabolized; resulting in fatty liver; fatty myocardium; fatty renal tubules and so on [3]. As NADH accumulates; it slows dehydrogenase reactions of the Kreb’s cycle such as the isocitrate dehydrogenase and α-ketoglutarate dehydrogenase reactions; thereby slowing the overall activity of the cycle. The high NADH: NAD ratio therefore directs metabolism away from Kreb’s cycle oxidation and toward fatty acid synthesis. The increased NADH also promotes fatty acid synthesis and opposes lipid oxidation with as net result; fat accumulation [14].
The Glutamate Dehydrogenase (GluDH) reaction also is affected by a rise in NADH concentration resulting in impaired gluconeogenesis. GluDH converts glutamate to α-ketoglutarate and ammonia in the presence of NAD [3]. This reaction is reversible. A shift in the reaction towards glutamate due to elevated NADH depletes the availability of α-ketoglutarate which is the major acceptor of amino groups in the transamination of amino acids.
Induced Metabolic Tolerance
As earlier mentioned; ethanol can induce enzymes of MEOS causing an increased rate of metabolism of substrates oxidation by this system. This induction contributes to the metabolic tolerance to ethanol that develops in the alcoholics (in addition to the central nervous tolerance) with other cytochrome P450 possibly also involved [15]. Once the MEOS is active; alcohol tolerance increases because the rate of alcohol metabolism increase [2]. In addition to tolerance to ethanol; alcoholics tend to display tolerance to various other drugs [14]. It has been observed that when an individual drinks and uses another drug at the same time; the drug will be metabolized more slowly because the MEOS is busy disposing of alcohol [1]. Consequently; the drug cannot be handled until later and the dose may build up so that its effect is greatly amplified – sometimes to the point of being fatal. In contrast; once a heavy drinker stops drinking and alcohol is no longer completing with other drugs the enlarged MEOS metabolizes drugs much faster than before [1]. As result; determining the correct dosages of medications can be challenging.
Gropper et al. [3] explained that retinol like ethanol; spills over into the MEOS when ADH is saturated and NAD stores are low because of heavy ingestion of ethanol; hence leading to ethanol induction of retinol-metabolizing enzymes. Although induction accelerates the hepatic oxidation of retinol; the oxidation product is not retinal but other polar; inert product of oxidation. In effect; the alcohol subject becomes tolerant to vitamin A; necessitating a higher dietary intake of the vitamin to maintain normal hepatocyte concentrations.
Interaction with Nutrients
Thiamin (vitamin B1)
Alcohol diminishes thiamin absorption; alcohol increase thiamin excretion and alcoholics consume such a poor-quality diet that there may be few; if any; vitamins in the foods and beverages consumed [16]. Even well-fed alcoholics may be deficient in vitamins – thiamin; vitamin A; folate; vitamin D; pyridoxine and vitamin E in part because ethanol disrupts vitamin metabolism [17]. Thiamin is required; in the tissues; for the assembly and proper functioning of several enzymes that are important for the breakdown or metabolism of sugar molecules into other types of molecules [18]. Proper functioning of these thiamin-using enzymes is required for numerous critical biochemical reactions in the body; including the synthesis of certain brain chemicals (neurotransmitters); production of the molecules making up the cell’s genetic material (i.e. nucleic acids) and production of fatty acids; steroids and certain complex sugar molecules [19]. Thiamin deficiency in alcoholics cause Wernicke-Korsakoff Syndrome (WKS) and beri-beri heart disease; and probably contributes to polyneuropathy [14]. Wernicke-Korsakoff syndrome is characterized by ocular motor signs; ataxia; a staggering gait and deranged mental functions [2]. Wernicke-Korsakoff syndrome typically consists of two components; a short lived and severe condition called Wernicke’s encephalopathy and a long lasting and debilitating condition known as Korsakoff’s psychosis [20]. The symptoms of Wernicke’s encephalopathy include mental confusion; paralysis of the nerves that move the eyes (ie oculomotor disturbances); and an impaired ability to coordinate movements particularly of the lower extremities (ie alexia). According to Sechi and Serra [21]; Wernicke encephalopathy is characterized by the presence of a triad of symptoms: ocular disturbances (ophthalmoplegia); changes in mental state (confusion) and unsteady stance and gait (ataxia). For example; patients with Wernicke’s encephalopathy may be too confused to find their way out of a room.
Korsakoff’s psychosis is a chronic neuropsychiatric syndrome characterized by behavioral abnormalities and memory impairment [22]. Vetreno [23] reiterated that amnesic symptoms of WKS include both retrograde and anterograde amnesia. The retrograde amnesia is shown by the patients’ inability to recall or recognize information for recent public events. The anterograde memory loss is demonstrated through deficits in tasks that involve encoding and then recalling lists of words and faces; as well as semantic learning tasks.
Although these patients have problems remembering old information (retrograde amnesia) it is the disturbance in acquisition of new information (anterograde amnesia) that is most striking.
Pyridoxine (Vitamin B6)
Alcohol impairs the conversion of pyridoxine and pyridoxamine to pyridoxal phosphate which is the main form of the vitamin found in systemic blood [3]. Inadequate intake may partly explain low pyridoxal phosphate; but increased destruction and reduced formation may also contribute [14]. Also; the presence of acetaldehyde formed from ethanol metabolism may enhance hydrolysis of pyridoxal phosphate with subsequent formulation of the excretory products; pyridoxic acid or 4 – pyridoxic acid. Pyridoxal phosphate is more rapidly destroyed in erythrocytes in the presence of acetaldehyde; the product of ethanol oxidation; perhaps by displacement of pyridoxal phosphate from the protein and consequent exposure to phosphatase [24].
Acetaldehyde pulls the vitamin B6 coenzyme out of its orientation with its enzyme causing an increased destruction of the vitamin [2]. This leads to decreased red blood cell production and causes a form of anaemia in alcoholics. Vitamin B6 is involved in protein metabolism. It is also needed for conversion of tryptophan to niacin and hence its deficiency affects niacin level negatively. Without adequate vitamin B6; synthesis of key neurotransmitters diminishes; and abnormal compounds produced during tryptophan metabolism accumulate in the brain [1]. This can cause depression and confusion and in extreme cases – convulsions.
Folic Acid
Folate deficiency generally results from a low or inadequate intake of folate-rich foods or inadequate absorption which often is associated with alcoholism. The diseased liver of alcoholics cannot retain as much folate and the kidney increases excretion. Whitney and Rolfes [1] noted that alcohol interfers with the secretion of biologically active folate into the bile and its reabsorption by enterohepatic circulation and so most alcoholics become folate deficient. Reduced nutrient absorption due to damage of the mucosa by alcohol can cause folate deficiency [2]. Folate deficiency inevitably leads to fewer villi which decreases the absorption of almost all the nutrients. Alcohol accelerates the production of megaloblastic anaemia in patients with depleted folate stores [25] and it suppresses the hematologic response to folic acid in folic acid-depleted patients [26].
Vitamin D
Dietary vitamin D may not be absorbed because the alcohol damaged pancreas can’t produce enough fat-digesting enzymes to facilitate fat absorption; which in turn inhibits vitamin D absorption [2]. In patients with alcoholic liver disease; vitamin D deficiency probably derives from too little vitamin D substrate; which results from poor dietary intake; malabsorption caused by cholestasis or pancreatic insufficiency and insufficient sunlight [27]. The damaged liver in alcoholics loses the capacity to convert vitamin D to its biologically active form. Maurice et al. (27) also explained that insufficient intake of calcium and phosphorus or decreased calcium absorption in the presence of normal or increased 1; 25OH vitamin D3 (and parathormone) may accelerate bone loss in patients with alcoholism.
Factors associated with excessive alcohol intake affecting bone loss include insufficient intake of nutrients (especially calcium; protein and or vitamin D) coupled with poor absorption of nutrients as well as elevated parathyroid hormone concentrations. Alcoholics relatively suffer from osteoporosis and experience more bone breaks. Several factors appear to be involved; alcohol enhances fluid excretion; which leads to excessive calcium losses in the urine; upsets the hormonal balance required for healthy bones; slows bone formation; leading to a lower bone density; stimulates bone breakdown and increase the risk of falling [1]. Alcoholism may cause bone cell dysfunction; which diminishes bone formation and reduces bone mineralization; leading to osteoporosis [2]. Alcoholics have decreases in bone density and bone mass; increased susceptibility to fractures and increased osteonecrosis [27]. Patients with alcoholism have abnormalities of calcium; phosphorus; and vitamin D homeostasis. With intoxication; the chances of falling increase thereby leading to a fracture.
Vitamin K
According to Berdanier et al. [14]; vitamin K deficiency in alcoholism may arise when there is an interruption of fat absorption due to pancreatic insufficiency; biliary obstruction; or intestinal mucosal abnormalities secondary to folic acid deficiency. It has been shown that inadequate intake of dietary vitamin K is not a likely cause of clinical deficiency unless there is concomitant sterilization of the large gut; which is a reliable source of the vitamin. Alcohol induced hepatocyte injury interferes with the use of available vitamin K; with a consequent drop in blood levels of clothing factors whose synthesis depends on this vitamin (27). Abnormally high levels of inactive factor (prothrombin) are found in the plasma in the presence of cirrhosis or vitamin K deficiency (28) This renders alcoholics susceptible to bleeding.
Iron
Berdanier et al. [14] stated that there may be either deficiency or excess of iron in the body of alcoholics. Alcoholics may be iron deficient because of the several gastrointestinal tract lesions to which they are prone and that may bleed. Iron overload may result from the inflammation of the intestines that affect the intestinal barriers and allows more iron to pass through. Alcohol damages the intestine; further impairing its defense against absorbing excess iron [1]. The absorbed iron is progressively deposited within tissues especially the liver; heart and pancreas among others causing extensive organ damage and ultimately organ failure [3].
Associated Organ Damage
Liver
Liver is the major organ for alcohol metabolism. About 90% of the absorbed alcohol circulates through the body and is eventually transported to the liver for metabolism via the portal vein while only about 10% is excreted through urine or breath [29]. Nearly all ingested alcohol is oxidized by hepatic (and to some extent; gastric) ADH and hetaptic MEOS. The brain; pancreas and stomach also metabolize alcohol [8]. Regardless of the amount of alcohol consumed; the liver metabolizes ethanol at the rate of 0.015 – 0.017 per hour and that is why large doses of alcohol could be fatal [30]. Since there is an increase in fatty acids synthesis because of high NADH: NAD; these fatty acids accumulate in the liver. With alcohol; the more dietary triglycerides that are present in the diet; the more fat accumulates in the liver [27]. Whitney and Rolfes [1] explained that fat accumulation can be seen in the liver after a single night of heavy drinking. This blocks the flow of blood to the liver cells; and they begin to die (necrosis). When the liver cells die; they form fibrous scar tissues – fibrosis. When these fibrous scar tissues harden; it leads to cirrhosis and at this stage; the condition is irreversible.
Brain damage
If more alcohol arrives at the liver than the enzymes can handle; the extra alcohol travels to all parts of the body; circulating again and again until liver enzymes are finally available to process it [1]. Some alcohol metabolism also occurs in other tissues; including the pancreas and the brain causing damage to their cells and tissues [10]. Acute and chronic alcohol consumption can have both subtle as well as dramatic effects on the brain and its functioning.
Whitney and Rolfes [1]; explained effect of alcohol on the
brain as follows:
• When alcohol flows to the brain; it first sedates the
frontal lobe – the reasoning part. As the alcohol molecules diffuse
into the cells of these lobes; they interfere with reasoning and
judgment.
• Speech and vision centers are affected next. If the
drinker drinks faster than the rate at which the liver can oxidize
the alcohol; blood alcohol concentrations rise; the speech and
vision centers of the brain become sedated.
• Voluntary muscular control is then affected. At this
point; people under the influence stagger when they try to walk.
• Respiratory and heart action are the last to be affected.
Finally; the conscious brain is completely subdued; and the person
passes out.
According to Brick [31]; in high level of alcohol consumption; the specialized poison control-cells of the brain detect too much alcohol and send signal to the stomach to vomit. This is an attempt to eliminate any unabsorbed alcohol from reaching the blood stream to save life.
Cardiovascular damage
Alcohol is a major source of excess calories which get turned into fat; so the triglyceride levels in the blood increase. Alcohol reduces the amount of the enzyme that breaks down triglycerides. Alcohol’s contribution to body fat is most evident in the central obesity that commonly accompanies alcohol consumption; popularly and appropriately known as the “beer belly” [32]. Fat infiltration can cause the heart to nearly twice its normal size; which may lead to death from heart failure [2]. Excess alcohol consumption over the course of long periods is associated with an increase in oxidative stress; which may account for some adverse effects on the cardiovascular system [32]. Diane et al. [33] also explained that the conversion of alcohol to acetaldehyde by cytochrome P450 2E1 is coupled with the generation of free radicals; reactive oxygen species; and lipid peroxidation resulting in liver and possible cardiac damage.
There have been controversies over the cardio protective effect of alcohol. Some researchers have suggested that drinking red wine can help prevent heart disease. Results; however; are not conclusive with some suggesting that it is the overall lifestyle of the participants rather than the drinking of red wine that led to the improvements [34]. Reseveratrol is a prostate cancer-fighting compound found in red grapes from which red wine is being made; it also prevents platelets in blood from clothing. Zilkens [34] also stated that consuming large amount of red wine or just grapes – which have a much lower concentration of antioxidants than wine will increase the insulin levels and eventually have a positive impact on your lipid health. Although alcohol has both immunosuppressive and anti-inflammatory properties; any beneficial effects; for example; on heart and vascular endothelium may be offset by increased susceptibility to infections [33]. Because apparent protection has been noted in people taking only one drink per week or per month; factors other than alcoholic beverages are at play; such as lifestyle; that contribute to the coronary protective effect observed in modest drinkers [27].
Gastrointestinal Tract (GIT) damage
Alcohol is toxic to the cells lining the esophagus; making cancer more likely [2]. According to Keshavarzian; Fields; Vaeth and Holmes [35]; alcohol consumption is associated with motility changes in the GIT including diarrhoea. Alcohol consumption is a cause of acute gastritis and duodenitis [36]. These areas of the gut are exposed to the highest concentration of ethanol for the longest times [27]. Barboriak and Meade [37] explained that the effects of ethanol on gastric emptying of meals are concentration dependents; higher concentration cause more consistent delays of passage of solid contents.
Alcohol is known to cause pancreatitis thereby decreasing the pancreatic output. Reduced enzymes output by the pancreases and decreased bile production by the liver makes the digestion and absorption of nutrients difficult [2]. Thus; the breakdown of amino acids and fats chiefly governed by the action of pancreatic enzymes is slowed or insufficiently completed. Feinman and Lieber [6] reiterated that alcoholic patients are often nutritionally depleted by inadequate food intake due to abdominal pain accompanied by years of poor digestion. In addition; nutritional deficiencies themselves may lead to further absorption problems example folate deficiency alters the cells lining the small intestine; which in turn; impairs absorption of water and nutrients (including glucose; sodium; and additional folate) [38].
Kidney damage
The kidneys are responsible for the regulation of the volume and the composition of body fluid; including electrically charged particles (i.e.; ions); such as sodium; potassium; and chloride ions. Epstein; [39] stated that alcohol’s diuretic effect alters the body’s fluid level; and this produces disturbances in the body’s electrolyte concentrations. This diuretic nature of alcohol leads to increased urine production and potential dehydration. Heavy alcohol consumption causes vasoconstriction; and this could to hypertension; a major risk factor for kidney diseases.
Fetal damage
Conclusive evidence shows that large amounts of alcohol harm the fetus especially when associated with binge drinking (for a woman; consumption of four or more alcoholic drink at one sitting) [2]. Binge drinking is especially perilous during the first 12 weeks of pregnancy as this is when critical early developmental events take place in the womb. When a pregnant woman drinks more alcohol than she can metabolize; the excess reaches the fetus which has no means of detoxifying it. Alcohol crosses the placenta freely and deprives the developing fetal brain of both nutrients and oxygen [1].
Whitney and Rolfes [1] also explained that the result may be fetal alcohol syndrome; a cluster of symptoms that include: prenatal and postnatal growth retardation; impairment of the brain and nerves; with consequent mental retardation; poor coordination and hyperactivity; abnormalities of the face and skull and increased frequency of major birth defects: cleft palate; heart defects and defects in ears; eyes; genitals and urinary system.
The most obvious symptoms of fetal alcohol syndrome are the abnormal facial features but the most tragic ones are the mental disabilities. When a woman drinks during pregnancy; she causes damage in two ways: directly by intoxicating and indirectly by malnutrition. Priors to the complete formation of the placenta; alcohol diffuse directly into the tissue of the developing embryo causing incredible damage. When alcohol crosses the placenta; fetal blood alcohol also can prevent the fetus from receiving necessary nutrients through the placenta [40].
The mother may not even appear drunk; but the fetus may be poisoned. Alcohol remains in the fetal blood long after it has disappeared from the maternal blood. It is not malnutrition that is the main cause of fetal alcohol syndrome but it arguments the clinical signs seen in these children. Poor nutrition may cause the mother to metabolize alcohol more slowly; exposing the fetus to high levels of alcohol for longer periods of time [41]. Whitney and Rolfes [1] noted that male alcohol ingestion also affects fertility and fetal development. An association between paternal alcohol intake one month prior to conception and low infant birth weight is apparent in human beings (Paternal alcohol intake was defined as average of two or more drinks daily or at least five drinks on one occasion). This relationship was independent of either parent’s smoking and of the mother’s use of alcohol; caffeine; or other drugs. An occasional drink may be innocuous; but researchers are unable to say how much alcohol is safe to consume during pregnancy. For this reason; health care professionals urge women to stop drinking as soon as they realize they are pregnant or; better; as soon as they plan to become pregnant.
Recommended intake of Alcohol
It is difficult to establish an exact amount of alcohol that is appropriate for everyone since people have different tolerance to alcohol. However; an accepted definition of moderate is not more than two drinks a day for the average-sized man and not more than one drink a day for the average sized women [1]. According to the United State Department of Agriculture (USDA) and the United State Department of Health and Human Services [42]; moderate drinking is consuming not more than two standard drinks per day for men and not more than one per day for women. The National Institute on Alcohol Abuse and Alcoholism [8] further recommended that people aged 65 and above limit their consumption of alcohol to a drink per day. WHO [43] stated that the safe limit of alcohol is two to three units/day; a maximum of 21 units per week for males and one to two units/day; a maximum of 14 units per week for females. Whitney and Rolfes [1] defined a drink as any alcoholic beverage that delivers ½ ounces of pure ethanol: i.e. 5 ounces of wine; 10 ounces of wine cooler; 12 ounces of beer and 1½ ounces of distilled liquor (80 proof Whisky; Scotch; rum or vodka).
Alcohol Abuse and Alcoholism
Alcohol abuse is the continued consumption of alcohol despite the development of social; legal or health problems [44]. It involves consumption of excess amount of alcohol to the detriment of human health or personality. Alcohol is also abused when it is used by under aged youth or in certain conditions such as pregnancy; lactation; and some degree of sickness. Alcohol abuse sets in much more quickly in young people than in adults [45]. Children as young as 10 may begin experimenting with alcohol to feel grown up; to fit in and belong to a group; to relax and feel good; to take risks and rebel against authority and simply to satisfy curiosity [2].
Alcoholism also known as addiction or alcohol dependence syndrome is a disease involving a strong need to drink or inability stop drinking. Alcoholism is usually progressive and develops when the abuser increased tolerance and drinks greater amount to achieve the same desired effect. It includes the repetitive use of alcohol; often to alleviate anxiety or solve other emotional problems [2].
Social and economic problems associated with alcohol abuse/alcoholism
Problem drinking can result in decreased job performance; an increased number of sick days; interference with regular sleep at home; and increased sleeping on the job [46]. It is extensively dangerous to mix drinking with activities requiring sound judgment and responsibility [47]. Alcohol does not belong to driving; athletics and water sports activities. Compared with nondrinking or moderate drinkers; people who frequently binge drink (at least three times within two weeks) are more likely to engage in unprotected sex; have multiple sex partners; damage property and assault others [48]. Binge or heavy drinking is defined as at least four to five drinks in a row [1].
Alcoholism affects the entire family. Living with an alcoholic family member causes stress for everyone; and; for a child; this dysfunction reduces the chances of becoming intellectually; culturally; and socially independent [1]. Children of alcoholics often have long-lasting emotional problem which they carry over into adulthood. Other social effect of alcoholism includes economic losses due to time off work owing to alcohol related disorders; illnesses and injury; chaotic family life and disruption of social relationship; emotional problems; violence; and legal problems.
Conclusion
Alcohol is not considered as an essential nutrient because it provides the body with empty calories. It requires no digestion; and its metabolism takes precedence over metabolism of the other energy yielding nutrients. Its metabolism depends on several factors such as gender; race and body composition amongst others. Alcohol has been implicated in several illnesses such as liver cirrhosis; gastrointestinal disturbances; and brain damage. Although it has been found to possess some cardioprotective qualities; medical practitioners do not recommend it to patients/clients because its risks far outweigh the benefits if the recommended maximum intake is exceeded. Alcohol not only has serious physiological effects on the body; but it also leads to emotional disturbances and social violence.
Recommendations
According to Wardlaw and Kessel [2]; there is no
commendation for a nondrinker to start consuming alcohol for
any health benefits.
• Do not exceed the recommended maximum intake for
your age and sex.
• Do not drink on an empty stomach.
• Drink slowly allowing at least one hour in between
drinks.
• Do not drink prior to engagement on activities that
require sound judgment e.g.; driving.
• Do not drink when you are planning to get pregnant and
when you are already pregnant and during breastfeeding.
• When you are drinking and feel thirsty; drink water
instead of more alcohol.
• Talk to a friend when you are depressed or confused
instead of taking solace in alcohol.
• When a drinker has passed out during drinking; he
should be allowed to sleep but must be watched over. He should
be helped to lie on his side instead of his back; so that when he
vomits; he won’t choke.
• Alcoholics should stop alcohol gradually to avoid
withdrawal syndrome.
• Alcoholics should join reputable therapy program for
them e.g.; Alcohol Anonymous in USA.
References
- Whitney EN, Rolfes SH (2002) Understanding Nutrition. 9th edition. USA: Wardsworth group pp.230-239.
- Wardlawl GN, Kessel M (2002) Perspectives in Nutrition. 5th edition. USA: McGraw-Hill pp.296-315.
- Gropper SS, Smith JL and Groff JL (2005) Advanced Nutrition and Human Metabolism. 4th edition. USA: Wardsworth group 101-105.
- Bennett LA, Campillo C, Chandrashekar CR, Gureje O (1998) Alcoholic Beverage Consumption in India, Mexico and Nigeria; a cross-cultural comparison. Alcohol Health and Research World 22(4): 243-252.
- GBD (2018) Alcohol Collaborators Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 392:1015-1035.
- Feinman L, Lieber CS (1999) Ethanol and lipid metabolism. American Journal of clinical Nutrition 70: 791-792.
- Klatsky A (2009) Alcohol and cardiovascular diseases. Expert Review of Cardiovascular Therapy 7(5): 499-506.
- National Institute on Alcohol Abuse Alcoholism, National Institutes of Health (2007) Alcohol Metabolism: An update. Alcohol Alert 72:1.
- Hurley TD, Edenberg HJ, Li TK (2002) The pharmacogenomics of alcoholism. In: pharmacogenomics: the search for individualized therapies. Weinheim, Germany: Wiley-VCH pp.417-441.
- Edenberg HJ (2007) The genetics of alcohol metabolism; Role of alcohol dehydrogenase and aldehyde dehydrogenase variants. Alcohol Research and Health 30(1): 5-13.
- Zakhari S (2006) Overview: How is alcohol metabolized by the body? Alcohol Research and Health 29(4): 245-254.
- Deitrich R, Zimatkin S, Pronko S (2006) Oxidation of ethanol in the brain and its consequences. Alcohol Research and Health 29(4): 266-273.
- Quetemont E, Didome V (2006) Role of acetaldehyde in mediating the pharmacological and behavioral effects of alcohol. Alcohol Research and Health 29(4): 256-265.
- Berdanier CD, Feldman EB, Flatt WP, Joer ST (2002) Handbook of Nutrition and Food. Washington D.C: CRC Press 915-935.
- Salmela KS, Kessova IG, Tsyrlov IB, Lieber CS (1998) Respective roles of human cytochrome P-4502E1, 1A2, and 3A4 in the hepatic microsomal ethanol oxidizing system. Alcohol: Clinical and Experimental Research 22(9): 2125-32.
- Tanphaichitr V (1999) Thiamin. In: Shils ME, Olson HA, Shike M, eds. Modern Nutrition in Health and Disease. 8th ed Philadelphia: Lea and Febiger 359-365.
- Green PHR, Tall AR (1999) Drugs, alcohol and malabsorption. American Journal of medicine 67: 1066-197.
- Bakalkin G (2008) Alcoholism associated molecular adaptations in brain neurocognitive circuits.
- Singleton CK, Martin PR (2001) Molecular mechanisms of thiamine utilization. Current Molecular Medicine 1(2): 197-207.
- Ellissavet K (2006) Alcoholic dementia: myth or reality. Annals of General Psychiatry 5(1): 57.
- Sechi GP, Serra A (2007) Wernicke's encephalopathy: new clinical settings and recent advances in diagnosis and management. The Lancet Neurology 6(5): 442-55.
- Victor M, Adams RD, Collins G (1989) The Wernicke-Korsakoff Syndrome and Related Neurologic Disorders Due to Alcoholism and Malnutrition. 2nd ed. Philadelphia: Davis.
- Vetreno RP (2011) Thiamine deficiency-induced neurodegeneration and neurogenesis (PhD Thesis). Binghamton University.
- Lumeng L, Li TK (1974) Vitamin B6 metabolism in chronic alcohol abuse. Pyridoxal phosphate levels in plasma and the effects of acetaldehyde on pyridoxal phosphate synthesis and degradation in human erythrocytes. Journal of clinical Investigation 53(3): 693-704.
- Lindenbaum J (1980) Folate and vitamin B12 deficiencies in alcoholism. Seminars in Hematology 17: 119-129.
- Sullivan LW, Herbert V (1964) Suppression of Hematopoiesis by Ethanol. Journal of Clinical Investigation 43(11): 2048-2062.
- Maurice ES, Shike M, Ross AC, Caballero B, Cousins RJ (2006) Modern nutrition in health and disease. 10th edition. USA: Lippincott Williams and Wilkins pp.1235-1255.
- Blanchard RA, Furie BC, Jorgensen M, Kruger SF, Furie B (1981) Acquired vitamin K-dependent carboxylation deficiency in liver disease. New England Journal of Medicine 305(5): 242-8.
- Cederbaum AI (2012) Alcohol metabolism. Clinical Liver Disease 16: 667-685.
- Office of Alcohol and Drug Education (2023) What is intoxication?
- Brick J (2005) Alcohol poisoning. Research and educational consulting 215: 504-510.
- Sakurai Y, Umeda T, Shinchi K, Honjo S, Wakabayashi K, et al. (1997) Relation of total and beverage specific alcohol intake to body mass index and waist-to-hip ratio: A study of self-defense officials in Japan. European Journal of Epidemiology 13(8): 893-898.
- Diane LL, Ricardo AB, Momtaz W, Thomas DG (2005) Opportunities. Journal of the American College of Cardiology 45: 1916-1924.
- Zilkens R (2005) Hypertension: Journal of the American Heart Association 45: 1-6.
- Keshavarzian A, Fields JZ, Vaeth J, Holmes E (1995) The differing effect of acute chronic alcohol on gastric intestinal permeability. American Journal of Gastroenterology 98(1): 2205- 2211.
- Gottfried EB, Korsten MA, Lieber CS (1978) Alcohol induced gastric and duodenal lesions in man. American Journal of Gastroenterology 70(6): 587-592.
- Barboriak JJ, Meade RC (1997) Effect of Alcohol on Gastric Emptying in Man. American Journal of Clinical Nutrition 23(9): 1151-1153.
- Feinman L (1989) Alcoholism and pancreatitis: Does nutrition play a role? Alcohol Health and Research world 13(3): 232-237.
- Epstein M (1997) Alcohol’s impact on the kidney function. Alcohol Health Research World 21(1): 84-92.
- Dreosti IE (1993) Nutritional factors underlying the expression of the fetal alcohol syndrome. Annals of the New York Academy of Sciences 678: 193-204.
- Shanker K, Hidestrand M, Liu X, Xiao R, Skinner CM, et al. (2006) Physiologic and genomic analyses of nutrition-ethanol interactions during gestation: implications for foetal ethanol toxicity.
- United States Department of Agriculture, United States Department of Health, Human Services (1995) Home and Garden Bulletin No. 232, 4th ed. Washington, DC: U.S. Department of Agriculture.
- World Health Organization (2018) Global Status Report on Alcohol and Health.
- Reoseli M, Habros P, Hollorius L (2005) Consumption of alcoholic beverages in relation to community health. Journal of epidemiology and community health 55: 648-652.
- Liu S (1997) Prevalence of Alcohol-impaired driving: Results from a national self-reported survey of health behaviours, Journal of the American Medical Association 277: 122-125.
- National Institute on Alcohol Abuse and Alcoholism (1995) Alcohol. Alert No. 29: College students and drinking. Bethesda MD: National Institute on Alcohol Abuse and Alcoholism.
- National Institute on Alcohol Abuse and Alcoholism (1999) Are women more vulnerable to alcohol’s effects? Alcohol Alert 46: 1
- Ferguson DM, Lynskey MT (1996) Alcohol misuse and adolescent sexual behaviors and risk taking. Pediatrics 98: 91-96.






























