Iron Pots for the Treatment of Iron Deficiency Anemia: Is there Sufficient Favorable Evidence?
Francisco Plácido Nogueira Arcanjo*, Cecília Costa Arcanjo and Paulo Roberto Santos
PhD, Universidade Federal do Ceará, Brazil
Submission: December 21, 2018; Published: March 13, 2019
*Corresponding author: Francisco Plácido Nogueira Arcanjo, Universidade Federal do Ceará, Campus Sobral, Av. Comandante Maurocélio Rocha Ponte, 100, Derby, 62.042-280, Sobral-CE, Brazil
How to cite this article: Francisco P N A, Cecília C A, Paulo R S. Iron Pots for the Treatment of Iron Deficiency Anemia: Is there Sufficient Favorable Evidence?. Nutri Food Sci Int J. 2019. 8(3): 555738. DOI:10.19080/NFSIJ.2019.08.555738.
Abstract
In the last years, there has been increasing interest in the development of affordable, easy-to-implement interventions to control the prevalence of iron deficiency anemia, due to the magnitude of this nutritional deficiency and knowledge of its effects on quality of life, morbidity and mortality. Previous studies have demonstrated that cooking food in cast iron pots could be efficacious in reducing the incidence of iron deficiency and iron deficiency anemia. This review highlights the results from the main published clinical trials on the effect of preparing food in cast-iron pots on hemoglobin concentrations and anemia prevalence rates, and their acceptability for cooking.
Keywords: Anemia; Iron Deficiency; Iron Pots; Nutrition; Review
Introduction
Iron deficiency anemia (IDA) results from lack of sufficient iron within the body leading to a decrease in mean hemoglobin (Hb) concentration, volume and size. IDA is typically caused by inadequate intake of iron, chronic blood loss, or a combination of both [1]. In the world, anemia affects almost 2 billion people and the majority of these live-in developing countries. Infants, children and women of reproductive age are especially at risk due to their increased nutrition needs [2,3]. In terms of public health, the negative repercussions of IDA are particularly serious as it is associated to inhibited growth, low birth weight, poor psychomotor and cognitive development, compromised immunity and increased infant morbidity and mortality [4-6].
Over the years, researchers have sought strategies to prevent and control IDA; however high IDA prevalence rates still persist in populations around the world, justifying the search for new strategies. One such strategy is the use of iron pots for cooking food. Up to date, different researchers have sought to assess the effect of cooking food in iron pots and its influence on hemoglobin concentrations in the blood with varying results, and a recently published paper has once again called into discussion this known but less popular method of iron supplementation [7]. The aim of this study is to conduct a review on the effect of preparing food in cast-iron pots on Hb concentrations and anemia prevalence rates, and the acceptability of these for cooking.
The Effect of Iron Pots on Hb concentrations and Anemia prevalence rates
As far as this review could determine, there is a relatively small number of published clinical trials on this theme. The main findings of which are summarized in this review and presented in Table 1 in order to simplify comparisons. In one randomized controlled clinical trial, Borigato et al. [8] assessed the efficacy of cooking food in iron pots for the prevention of anemia in premature infants aged 4 to 12 months (postnatal age). After intervention, the infants fed with food cooked in iron pots had significantly better hematologic values compared to the aluminum pots group, and lower IDA prevalence rates (36.4 vs. 73.9%). Adish et al. [9] conducted a community-based randomized trial to assess the effect of cooking in iron cooking pots compared to aluminum pots in Ethiopian children aged 2-5 years. At the end of the 12-month intervention, hemoglobin concentrations of participants in the iron-pot group was 1.7g/ dL higher than at baseline (p=0.008), which represented an adjusted difference of 1.3g/dL (p<0.001) between the groups. Furthermore, in the iron-pot group, anemia prevalence rates (hemoglobin <11g/dL) decreased from 57% to 13%, while the rate in the aluminum-pot group fell much less, from 55% to 39%.
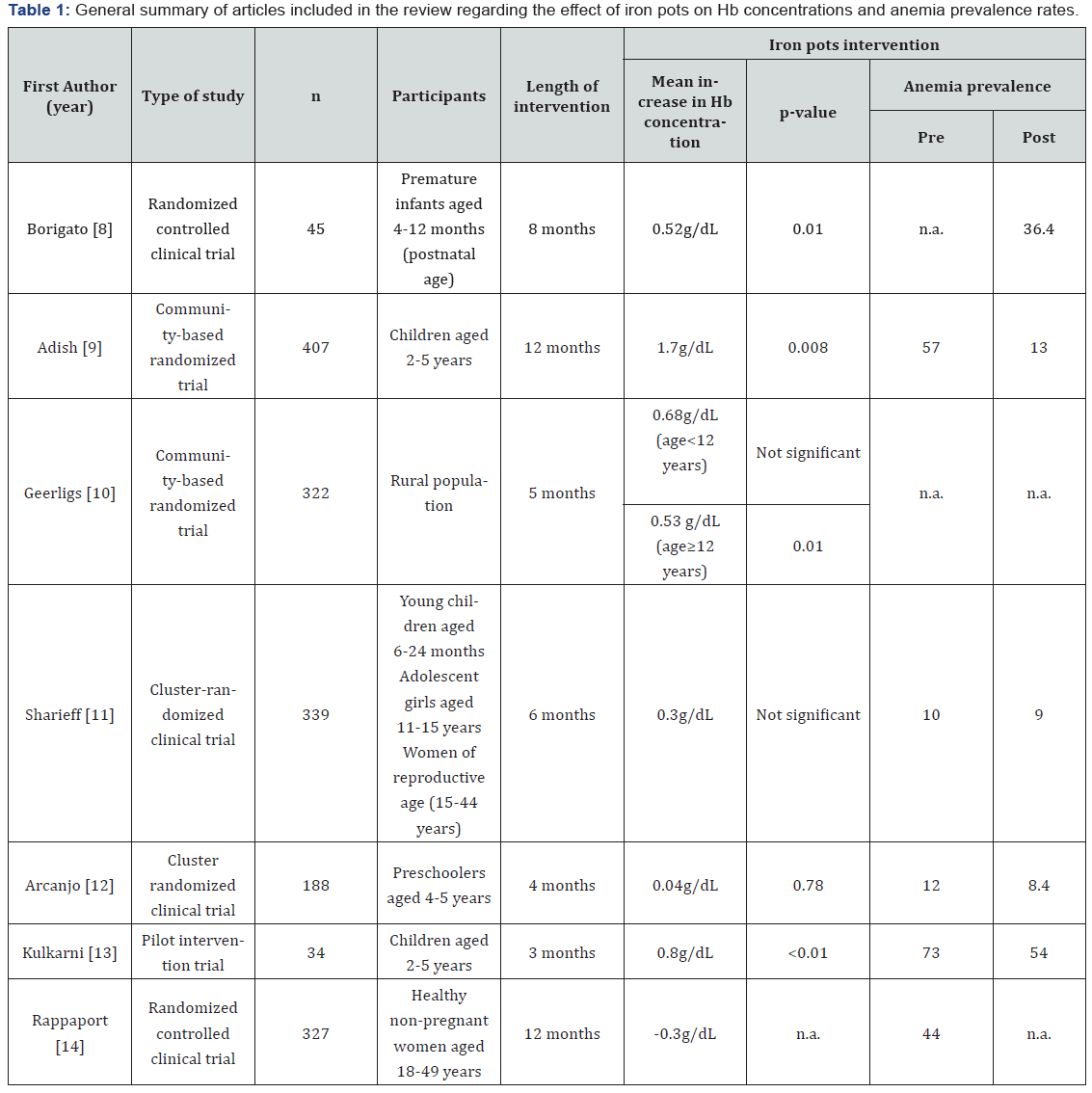
All numbers are absolute, unless otherwise stated.
p-value baseline - end-line
n.a. not available
Geerlings et al. [10] performed a community-based randomized trial to compare the effects of cooking food in iron pots with aluminum pots in an area with high malaria prevalence. Results from the study showed that adults (age ≥ 12 years) in the iron pots group presented a significant increase in Hb levels after 6 weeks, this difference remained significant after 20 weeks (iron + 5.3g/l vs. aluminum -2.2g/l, mean difference 7.5g/l, p=0.01); children (age < 12 years) showed an improvement in iron deficiency with no significant increase in Hb levels, possibly due to high malaria and parasite prevalence.
A cluster-randomized clinical trial was conducted in Benin with young children (aged 6-24 months), adolescent girls (aged 11-15 years) and women of reproductive age (15- 44 years). Individuals were randomly assigned to one of three intervention groups: cast iron cooking pot, blue steel cooking pot or control. Participants in the control group received either SprinklesTM or iron tablets. However, the results from this study were inconclusive regarding the efficacy of cooking food in iron pots to reduce IDA [11]. Another cluster randomized clinical trial, performed by Arcanjo et al. [12] with preschoolers aged 4 to 5 years, examined the effect of preparing food in iron pots on Hb concentrations. In the iron pots group, there was a non-significant increase in mean Hb concentration (0.04g/dL); however, there was a greater reduction in anemia prevalence (from 12.2 to 8.5%) than in the aluminum pots group. Furthermore, when only anemic preschoolers were analyzed there was a significant mean increase in mean Hb concentration, 1.69g/ dL (<0.0001).
A pilot study to develop iron rich snacks using iron pots compared to Teflon coated non-stick pots was conducted by Kulkarni et al. [13]. In this randomized trial, the efficacy of the snack was examined according to the Hb status of preschool children during a 3-month intervention. After intervention there was a significant increase (7.9 %) in mean hemoglobin, (from 10.1±1.6 to 10.9±1.7), serum iron and transferrin saturation. Moreover, anemia prevalence reduced from 73% at baseline to 54% at end-line. Another innovative trial by Rappaport et al. [14] assessed the use of a reusable fish-shaped iron ingot designed for home cooking and shaped like a fish. This randomized controlled trial in rural Cambodian anemic women (aged 18-49 y) was to explore the effect of cooking who with the iron ingot compared with a daily iron supplement or control after 1 year; however, no significant difference was observed in mean hemoglobin concentrations between the iron-ingot group, the iron-supplement group or the control group at the end of the intervention.
Acceptability of Iron Pots for cooking
Since iron pots may provide an innovative method to address IDA, other studies have been carried out to assess the acceptability of these for cooking. In one randomized trial study, by Prinsen Geerligs et al. [15], to evaluate acceptability, compliance and attitude towards the use of iron pots versus aluminum pots for cooking in two rural Malawian villages, the authors concluded that iron pots did not constitute an appropriate a strategy to reduce IDA in rural Malawian households due to their low acceptability when aluminum pots were available. The researchers added that to increase the acceptability of the iron pots a number of actions could be considered such as the absence of aluminum pots in order to reduce selection preference, and their introduction with clear instructions on best practice for pot use.
Another intervention trial was conducted by Tripp et al. [16] to assess the acceptability of iron pots for cooking in three refugee camps in western Tanzania. It was identified that iron pots were unpopular since they were heavier, more prone to rusting and more difficult to wash than stainless steel pots. The researchers alerted that the low usage of iron-alloy pots may lead to selling in poor populations, especially those with access to other pots.
Conclusion
IDA is a global public health problem, which is associated with an increased risk of morbidity and mortality, especially in pregnant women and children under five years of age. Consequently, there is an urgent need for innovative, lowcost interventions to treat and prevent anemia in these at-risk populations. From this review, the authors witnessed that cooking food in iron pots was beneficial to Hb concentrations in young children up to the age of 5 years. In communities with high prevalence rates of anemia, where other iron supplementation or fortification programs may be impractical, cooking in iron pots may provide a simple, useful and costeffective strategy to tackle IDA. However, educational programs would be necessary to elicit the importance and relevance of cooking in iron pots. Nevertheless, large scale interventions in different populations are necessary to confirm the effectiveness of this intervention on hemoglobin concentrations in at-risk populations.
References
- Johnson-Wimbley TD, Graham DY (2011) Diagnosis and management of iron deficiency anemia in the 21st century. Therap Adv Gastroenterol 4(3): 177-184.
- Viteri FEA (1998) New concept in the control of iron deficiency: community-based preventive supplementation of at-risk groups by the weekly intake of iron supplements. Biomed Environ Sci 11(1): 46-60.
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, et al. (2013) Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 382(9890): 427-451.
- Beard JL (2001) Iron biology in immune function, muscle metabolism and neuronal functioning. J Nutr 131(2S-2): 568S-580S.
- Domellöf M, Thorsdottir I, Thorstensen K (2013) Health effects of different dietary iron intakes: a systematic literature review for the 5th Nordic Nutrition Recommendations. Food Nutr Res 57.
- World Health Organization (2001) Iron deficiency anaemia: assessment, prevention, and control. A guide for programme managers. WHO, Geneva, Switzerland, pp. 114.
- Bansal D, Jain R (2018) Cooking in Iron Pots for Iron Deficiency Anemia: The Traditional Way Forward? Indian J Pediatr 85(8): 605- 606.
- Borigato EV, Martinez FE (1998) Iron nutritional status is improved in Brazilian preterm infants fed food cooked in iron pots. J Nutr 128(5): 855-859.
- Adish AA, Esrey SA, Gyorkos TW, Jean-Baptiste J, Rojhani A (199) Effect of consumption of food cooked in iron pots on iron status and growth of young children: a randomised trial. Lancet 353(9154): 712-716.
- Geerligs PP, Brabin B, Mkumbwa A, Broadhead R, Cuevas LE (2003) The effect on haemoglobin of the use of iron cooking pots in rural Malawian households in an area with high malaria prevalence: a randomized trial. Trop Med Int Health 8(4): 310-315.
- Sharieff W, Dofonsou J, Zlotkin S (2008) Is cooking food in iron pots an appropriate solution for the control of anaemia in developing countries? A randomised clinical trial in Benin. Public Health Nutr 11(9): 971-977.
- Arcanjo FPN, Macêdo DRR, Santos PR, Arcanjo CPC (2018) Iron Pots for the Prevention and Treatment of Anemia in Preschoolers. Indian J Pediatr 85(8): 625-631.
- Kulkarni SA, Ekbote VH, Sonawane A, Jeyakumar A, Chiplonkar SA, et al. (2013) Beneficial effect of iron pot cooking on iron status. Indian J Pediatr 80(12): 985-989.
- Rappaport AI, Whitfield KC, Chapman GE, Yada RY, Kheang KM, et al. (2017) Randomized controlled trial assessing the efficacy of a reusable fish-shaped iron ingot to increase hemoglobin concentration in anemic, rural Cambodian women. Am J Clin Nutr 106(2): 667-674.
- Prinsen Geerligs P, Brabin B, Mkumbwa A, Broadhead R, Cuevas LE (2002) Acceptability of the use of iron cooking pots to reduce anaemia in developing countries. Public Health Nutr 5(5): 619-624.
- Tripp K, Mackeith N, Woodruff BA, Talley L, Mselle L, et al. (2010) Acceptability and use of iron and iron-alloy cooking pots: implications for anaemia control programmes. Public Health Nutr 13(1): 123-130.






























