Perioperative Nutrition Optimization in Elective General Surgery: A Literature Review
Catherine Lindsay McKnight*
Department of Surgery, Trauma, and Critical Care, University of Tennessee-Knoxville, USA
Submission: May 5, 2017; Published: November 10, 2017
*Corresponding author: Catherine Lindsay McKnight, Department of Surgery, Trauma, and Critical Care, University of Tennessee-Knoxville, Tennessee, 1924 Alcoa Highway BoxU-11, Knoxville, USA, Tel: 864-305-6058; Fax: 865-3059231; Email: cmcknight@utmck.edu
How to cite this article: Catherine L M. Perioperative Nutrition Optimization in Elective General Surgery: A Literature Review. Nutri Food Sci Int J. 2017; 3(5): 555622. DOI:10.19080/NFSIJ.2017.03.555622.
Abstract
Prevention has been a recent focus not only in primary care but also in surgery as well, and appropriately there have been state and nationwide movements to reduce patients’ overall risks when receiving an elective surgery. The American College of Surgeons National Surgical Quality Improvement Program (NSQIP) is an outcomes-based program to measure and improve the quality of surgical care in the private sector. The NSQIP database focuses on post operative risks such as deep venous thrombosis, surgical site infection, adverse cardiac events, post-operative pneumonia, and several more. For prevention of these risks, factors such as temperature, glucose control, perioperative antibiotics, smoking cessation, electrolyte management, perioperative beta blockers and statins have been the concentration. Preoperative albumin is reported, but overall nutritional status is currently not reported as a factor associated with surgical risk.
Before the surgical community can identify it as a risk factor, nutrition must be defined. Defining nutrition has not been an easy task and is debated even amongst nutrition experts. Once nutrition is defined, surgeons need an accurate but efficient assessment tool to preoperatively identify the patients at risk. Once a patient is identified as high risk, a surgeon must know the therapies to implement to prevent postoperative complications.
Keywords: Nutrition; Perioperative; Surgery; Outcomes; Risk factors
Abbreviations: NSQIP: National Surgical Quality Improvement Program; ASPEN: American Society for Parenteral and Enteral Nutrition; BMI: Body Mass Index; NRSP: Nutritional Risk Score; AHA: American Heart Association; ASA: American Society of Anesthesiologists; TPN: Total Parenteral Nutrition
Introduction
Definition
According to most recent ASPEN guidelines, malnutrition is defined by involuntary loss of 10% or more of usual body weight within 6 months, involuntary loss of 5% or more of usual body weight in 1 month, involuntary loss or gain of 10 pounds within 6 months, body mass index less than 18.5 kg/m2 or greater than 25 kg/m2, chronic disease, increased metabolic requirements, altered diets or diet schedules, or inadequate nutrition intake, including not receiving nutrition for greater than 7 days [1]. Having a definition helps clinicians assess which surgical patients are at risk.
Perioperative nutrition is still neglected by the majority of surgeons. A Swiss-Austrian Survey performed in 2011 of 173 surgical departments showed that 80% of surgeons agreed nutrition decreases complications, 59% agreed nutrition decreases length of hospital stay, but only 20% of surgeon’s implemented routine screening [2]. The disconnect does not seem to be the lack of recognition of the importance of nutrition, but more the lack of initiative and resources to start a method of screening.
Assessment
Screening elective general surgery patients for nutrition as a risk factor does not need to be an expensive or time consuming process. Elective general surgery can be split into low risk and high risk operations, and the surgical population can be divided into healthy and unhealthy. Three questions a surgeon must ask him or herself before an elective operation is: What is this patient’s current nutritional status? How severe is the surgical insult? How will my surgery affect nutrition delivery and absorption? [3].
To answer the first question, a nutritional screening tool should be used. There are several screening tools available. Jie B et al. [4] in Nutrition 2012 performed a prospective multicenter cohort study on 1085 patients looking at preoperative nutritional assessment with the NRS-2002 (Table 1 & 2) showing 512 patients at risk of complications. 102 patients had an NRS>5. Preoperative nutritional therapy was shown to benefit patients with an NRS>5 vs an NRS<5: 50.6 versus 25.6% risk in complications and 17 versus 13 days hospital length of stay respectively. The majority of studies and clinicians use an NRS 2002 score of >3 to decide when to involve a nutritional specialist [4].
A more recent multivariate analysis was performed by Grass et al. to assess whether nutritional parameters correlate with the NRS-2002 to identify postoperative morbidity. The study concluded that the nutritional support based on NRS- 2002 screening potential could result in overfeeding and deleterious clinical consequences [5]. The recommendation developed that any patient with an NRS-2002 score of >3, needs to be assessed by a nutrition specialist to guide nutritional intervention. The NRS-2002 score should be used as one tool in the surgeon’s tool belt, and should be used in conjunction with proper nutritional assessment by a nutrition specialist (Table 1).
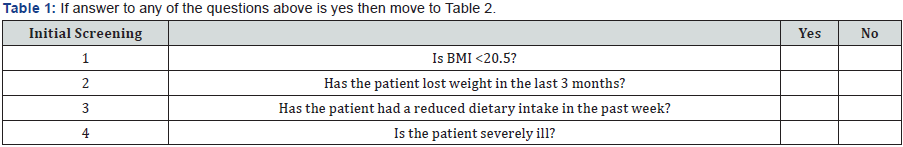
If answer to any of the questions above is yes then move to (Table 2)
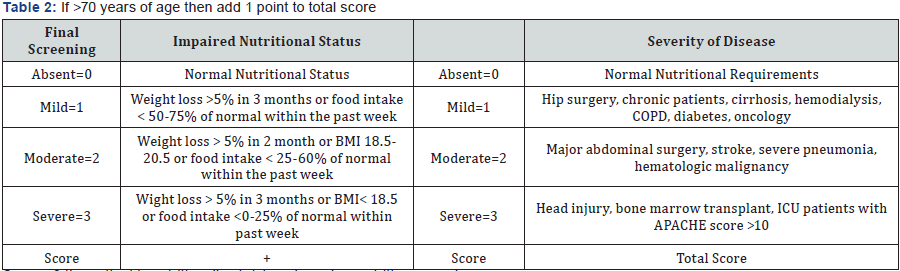
Score >3 the patient is nutritionally at risk and needs a nutrition care plan
Score <3 then patient is screened weekly prior to surgery [1,6-8].
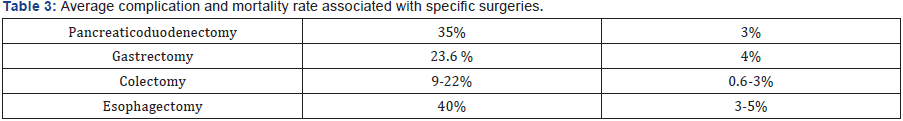
The severity of surgical insult depends on the patient’s risk factors and the type of operation. AHA and ASA are classification systems to assess a patient’s cardiac risk and overall fitness for surgery respectively. The complication and mortality rate differs depending on the specific operation (Table 3).
Should surgeons use Albumin as an assessment tool or a surrogate marker? In 1997 a VA Preoperative Risk Assessment Study was published in JACS concluding that preoperative albumin is the single best predictor of overall operative risk. Decreased albumin was associated with increased mortality, increased pneumonia, anastomotic leaks, abscess, respiratory failure, use of TPN, and ICU and hospital length of stay. This was again reconfirmed in 2003 by Kudsk et al in JPEN. Currently there is no good measure to follow. Prealbumin and CRP may be helpful but do not replace clinical judgment. Preoperative Albumin is currently recorded in the NSQIP database.
An expensive but newer screening tool involves imaging with MRI or CT scan objectively looking at the muscle and fat ratio. Objective measures of sarcopenia directly correlate with perioperative complications [9]. The suggestion is not to order imaging on every elective general surgery patient if there is no other indication for imaging, but the majority of patient’s about to undergo surgery have other indications for a CT scan, and this can be a helpful tool to predict postoperative complications. Preoperative low lean body mass is a predictor of perioperative weight loss which is known to increase a patient’s risk of complications [10].
Preoperative
Oral supplementation
After a patient is determined to be at higher risk for postoperative complications, they should see a nutritional specialist, but how is the nutritional care plan determined? There is a new meta-analysis that compares preoperative oral nutritional supplements versus immunonutrition. Oral nutritional supplements were not inferior to immunonutrition on several outcomes including wound infection, overall complications, and hospital length of stay [11]. Specific to colorectal surgery, preoperative oral carbohydrate loading has been shown to significantly decrease hospital length of stay and trend toward earlier return of gut function when compared to fasting or supplementary water [12]. Other meta-analysis shows the same results in addition to improvement of postoperative nausea and vomiting. Even though carbohydrate load groups display similar plasma glucose patterns to the non-carbohydrate load groups, this practice should be used with caution in diabetic patients [13].
Mechanical bowel preparations and antibiotics
The literature on colorectal surgery has been pendulous in terms of preoperative bowel preparations and enteral and parenteral antibiotics. Large variations are seen throughout the surgical community. Modulation of microbiota preoperatively to improve overall outcomes is a current hot topic. In animal models there is an increase in mortality with inoculation of Pseudomonas secondary to the expression of barrier disrupting adhesin PA-IL. Anastomotic disruption can be caused by change in bacterial flora and some of the causes of change include mechanical bowel preparations, antibiotic bowel preparations, parenteral antibiotic administration, ischemia, etc [14,15].
Probiotics
Probiotics can decrease the clostridium difficile infection rates and is known to decrease enterobacteriaceae levels. This has been shown in 6 small studies, but probiotics still carries a safety profile [16-18].
Perioperative
Enteral
Type of Nutrition: Nutrition deteriorates immediately in the postoperative period resulting in a decrease in weight, BMI, and arm circumference at 30 days postoperative. 50% of patients lose >5% Total B ody Weight. E arly enteral nutrition can decrease infectious complications and mortality. A metaanalysis looking at 26 randomized control trials of immune formula given after open gastrointestinal operations exhibited decreased infectious complications by 36%, an 18% overall decrease in complications, a decreased length of hospital stay in over 75% of the studies, but no decrease in overall mortality in 100% of the studies [19].
One of the newest studies compares patients who received perioperative immunonutrition versus patients who did not receive perioperative immunonutrition. Four outcome variables reached statistical significance including the overall percentage of complications, and percentage with any infectious complications, surgical site infection, including superficial and deep [20].
Timing of Nutrition: Early implementation of enteral nutrition is encouraged in the postoperative setting even without waiting on bowel function. In colorectal surgery, patients who were started on early enteral feeds had decreased anastomotic leak rates when compared to patients who awaited bowel function. Contraindications of early enteral feeds include bowel obstruction, high output fistulas, under resuscitated critically ill patients who are not perfusing their gastrointestinal tract, and short bowel syndrome. Ileus is not a contraindication to enteral feeds.
Parenteral
Historically some surgeons have “bulked up” patients in the perioperative period with supplemental TPN. The VA Coop study from 1991 showed that perioperative TPN did not improve outcomes and trended toward increased complications including excess calories, excess omega-6 fatty acids, and poor glucose control [21]. To address preoperative supplementation, the parenteral route is an option if there is no alternative route available. The bulk of studies support 5 days of supplementation [22,23].
Discussion and Conclusion
Nutritional optimization should be achieved periopertively for the elective surgical patient. Surgeons have multiple barriers to overcome to achieve this goal. Patient compliance may be a barrier, but improving preoperative education through literature and programs may improve overall patient compliance. Resources, time constraints, and finances may prevent the initial screening and nutrition planning with a patient. Understanding the definition of malnutrition first will aid surgeons in their assessment of patients.
Once high risk patients are identified, recommendations are for a nutrition specialist to be consulted to help develop a nutrition care plan. Some facilities may not have the luxury of a nutrition specialist for outpatients. If this is the situation, then the responsibility falls on the surgeon alone. Adoption of malnutrition as a risk factor by quality improvement projects would help decrease several postoperative complications and would also challenge surgeons to include nutrition risk assessments in their preoperative planning.
References
- White JV, Guenter P (2012) Consensus Statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Under-nutrition). JPEN J Parent Ent Nutr 36(3): 275-283.
- Grass F, Cerantola Y, Schafer M, Muller S, Demartines N, et al. (2011) Perioperative nutrition is still a surgical orphan: results of a Swiss- Austrian Survey. Eur J Clin Nutr 65(5): 642-647.
- Miller KR, Wischmeyer PE, Taylor B, McClave SA (2013) An Evidence- Based Approach to Perioperative Nutrition Support in the Elective Surgery Patient. J Parenter Enteral Nutr 37(5): 39-50.
- Jie B (2012) Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition 28(10): 1022-1027.
- Grass (2015) Preoperative nutritional screening by the specialist instead of the nutritional risk score might prevent excess nutrition: a multivariate analysis of nutritional risk factors. Nutrition Journal 14: 37.
- Papenfuss WA, Kukar WA, Oxenberg J (2014) Morbidity and mortality associated with gastrectomy for gastric cancer. Ann Surg Oncol 21(9): 3008-3014.
- Haigh PI, Bilimoria KY, DiFronzo LA (2011) Early postoperative outcomes after pancreatic oduodendecotmy in the elderly. Arch Surg 146(6): 715-723.
- Papenfuss WA, Kukar M, Attwood K (2014) Transhiatal versus transthoracic esophagectomy for esophageal cancer: a 2005-2011 NSQIP comparison of modern multicenter results. J Surg Oncol 110(3): 298-301.
- Sandini M (2016) A high visceral adipose tissue-to-skeletal muscle ratio as a determinant of major complications after pancreatoduodenectomy for cancer. Nutrition 32(11-12): 1231-1237.
- Grass F (2016) Nutritional Status Deteriorates Postoperatively Despite Preoperative Nutrtional Support. Ann Nutr Metab 68 (4): 291-297.
- Hegazi RA, Hustead DS, Evans DC (2014) Preoperative standard oral nutrition supplements vs immunonutrition: results of a systematic review and meta-analysis. JACS 219(5): 1078-1087.
- Jones C (2011) The role of carbohydrate drinks in preoperative nutrition for elective colorectal surgery. Annals The Royal College of Surgeons of England 93(7): 504-507.
- Jones C (2011) The role of carbohydrate drinks in preoperative nutrition for elective colorectal surgery. Annals The Royal College of Surgeons of England 93(7): 504-507.
- Fink D (2011) Pseudomonas aeruginosa potentiates the lethal effect of intestinal ischemia-reperfusion injury: the role of in vivo virulence activation. J Trauma 71(6): 1575-1582.
- Morowitz MJ (2011) The human microbiome and surgical disease. Ann Surg 253(6): 1094-10101.
- He D, Wang HY, Feng JY (2013) Use of pro/synbiotics as prophylaxis in patients undergoing colorectal resection for cancer: a meta-analysis of randomized controlled trials. Clin Res Hepatol Gastroenterol 37(4): 406-415.
- Sadahiro S, Suzuki T, Tanaka A (2014) Comparison between oral antibiotics and probiotics as bowel preparation for elective colon cancer surgery to prevent infection: prospective randomized trial. Surgery 155(3): 493-503.
- Steele SR, McCormick J, Genevieve M (2015) Practice Parameters for the management of Clostridium difficile infection. Dis Col Rectum 58(1): 10-24.
- Marimuthu K (2012) A meta-analysis of the effect of combination of immune modulating nutrients on outcome in patients undergoing major open gastrointestinal surgery. Ann Surg 255(6): 1060-1068.
- Moya P (2016) Perioperative Standard Oral Nutrition Supplements Versus Immunonutrition in Patients Undergoing Colorectal Resection in an Enhanced Recovery (ERAS) Protocol: A Multicenter Randomized Clinical Trial (SONVI Study). Medicine 95(21): 3704.
- The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group (1991) Perioperative Total Parenteral Nutrition in Surgical Patients. The New England Journal of Medicine 325(8): 525-532.
- Bharadwaj S (2016) should perioperative immunonutrtion for elective surgery be the standard of care? Gastroenterol Rep 4(2): 87-95.
- Wilson MZ, Dillon PW, Hollenbeak CS (2014) How do risk factors for mortality. Surg Endosc 28(12): 3392-3400.






























