Prevalence of High-Risk Human papillomavirus Genotypes and Predictors factors for Cervical Cancer in Unimmunized Brazilian Women without Cytological Abnormalities
Dra. Rachel Siqueira de Queiroz Simões1*, Emmanuele Pariz Silva2 and Dra. Ortrud Monika Barth1
1 Laboratory of Morphology and Viral Morphogenesis, Instituto Oswaldo Cruz, Fundação Oswaldo Cruz, Brazil
2 Vale do Itajaí, Itajaí University, Santa Catarina, Brazil
Submission: February 26, 2018; Published: March 29, 2018
*Corresponding author: Rachel Siqueira de Queiroz Simões, Laboratory of Morphology and Viral Morphogenesis, Instituto Oswaldo Cruz, Fundação Oswaldo Cruz, Avenida Brasil 4365, 21040-900, Rio de Janeiro, Brazil.
How to cite this article: Dra. Rachel Siqueira de Queiroz Simões, Emmanuele Pariz Silva, Dra. Ortrud Monika Barth. Prevalence of High-Risk Human papillomavirus Genotypes and Predictors factors for Cervical Cancer in Unimmunized Brazilian Women without Cytological Abnormalities. Adv Biotech & Micro. 2018; 8(5): 555749. DOI: 10.19080/AIBM.2018.08.555749
Abstract
HPV is the most common sexually transmitted disease based on its oncogenic activity as high-risk (hr) types, low-risk types (lr) and types of undetermined-risk depending upon the associated diseases. The aim of this study was to evaluate the HPV infection prevalence and to identify the risk factors as demographic, behavioral and biological variables related to cervical cancer in unimmunized and sexually active women patients attended at public health institutions. A cross-sectional study conducted from 2014 to 2016 was performed at Rio de Janeiro city. All women were randomly selected and submitted to clinical and sociodemographic investigation. About 100 cervical cell scrapings were collected with a cervical cytobrush during the gynecological examination. After nucleic acid amplification directed to a conserved region of the HPV L1 gene, high-risk type specific primers (HPV16/18/31/45) were performed for genotyping. Statistical analysis was applied to analyze the risk factors associated with HPV infection in 18 sociodemographics variables obtained from informative questionnaires. This study demonstrated by the Chi-square test that of the 100 participants, 20% (95% CI: 12-28) were DNA HPV positive. HPV 18 and 45 were the most frequently detected HPV types. Most women were currently not married (56%) and married or cohabitating (44%) (p<0.05). Psychosocial and psychosexual issues demonstrated that six percent of the women exhibit history of sexually transmitted diseases, except HIV, with 85% of women having sex with until to five partners (p<0.03) and 15% used oral contraceptives, while 71% did not use any type of condom (p<0.03). A previous history of STD was not significantly related. Cytological status was without alterations in the population investigated. This paper contributed to a better understanding about the natural history of HPV from of the pre-immunization prevalence study of the active sexually and clinical free lesions women in Brazil.
Keywords: Cervical cancer; Epidemiology; Human papillomavirus; Predictor factors; Prevalence
Introduction
Human papillomavirus (HPVs) are double stranded, non-enveloped DNA virus of the Papilloma viridae family. The mucosal HPV types have been described in the Alpha papillomavirus genus that infects the anogenital epithelium. HPV is the most common sexually transmitted disease based on their oncogenic activity as high-risk (hr) type, low-risk type (lr) and type of undetermined-risk depending upon the associated diseases [1-3].
Cervical cancer is the most common cancer in the developing countries. Several studies described the prevalence and age distribution of different HPV types with systematic review about the HPV vaccination programme [4] including risk populations [5] among adolescents [6] and young women with normal cytology [7]. In Scotland, the type specific prevalence of HPV was performed using three specimen types for urine (32.2%), self- taken swab (39.5%) and liquid based cytology samples (49.4%) [8]. In England, a comparative prevalence study and odds ratio of HPV infection in the three different age groups (16-18y.o; 19-21 y.o; 22-24 y.o) were performed in the pre-immunization and post-immunization period [9].
The United States epidemiological study, using self-administered questionnaire about HPV vaccine and other characteristics, was conducted among mothers with her daughter and son between the ages of 9 and 17 years [10]. Brazilian study of HPV in oral mucosa detected 23.2% prevalence in patients free of clinical-pathological alterations [11]. DNA HPV was detected in the oral mucosa of asymptomatic men who have had over 16 sexual partners since initiation activity [12].
In Greece, HPV-16 and 51 were the most prevalence detected high risk HPV (hrHPV) types of 27.4%. Multiple HPV infections were detected in younger women (14-19 y.o) [13]. A population- based study in Costa Rica, showed a positive association between vaginal pH and multiple HPV types infections and intraepithelial neoplasia [14]. Another study about cost-effectiveness analyses of HPV vaccination against cervical cancer and prevention of genital warts was performed in the Netherlands using epidemiological and economic parameters [15]. The economic impact of quadrivalent HPV vaccination was analyzed in Brazil also using a transmission dynamic model [16] as in Estonia [17] and Scotland [8].
More than 200 HPV genotypes and several HPV types associated with particular diseases as oral lesions (Heck´s disease, oropharyngeal carcinoma, laryngeal papillomas), anogenital warts (Bowenoid papulosis, Buschike-Lowenstein tumor), Epidermodysplasia verruciformis (plane warts, Pityriasis-like plaques, squamous cell carcinomas of sun-exposed skin) have been described [18]. Previous studies investigated the most efficient and cost effective cervical cancer screening program. The Brazilian Immunization Program recommended the vaccine to be administered at 9 to11 years of age before most adolescents became sexually active. HPV vaccination is the best preventive strategy against cervical cancer, cervical intraepithelial neoplasia and genital warts. Licensed HPV vaccines are bivalent (Cervarix®) against HPV16/18 (Glaxo Smith Kline Biologicals S.A.), quadrivalent (Gardasil®) target HPV16/18/6/11 (Sanofi Pasteur/ Merck Sharp & Dohme- MSD) or nonavalent vaccines (Gardasil-9®) target HPV16/18/31/33/45/52/58/6/11 and have been applied in many countries [19].
Several potential benefits of vaccination have been associated in HPV related diseases as cancer anus-genital, head and neck cancer, colorectal tumors, cancer penile and recurring respiratory papillomatosis. The aim of this study was to evaluate the HPV infection prevalence and to identify the risk factors as demographic, behavioral and biological variables related with the cervical cancer in unimmunizedand sexually active women patients attended at public health institution.
Materials and Methods
Epidemiological study
A cross-sectional study conducted from 2014 to 2016 was performed at the Manguinhos Complex community in Rio de Janeiro city. This study was approved by Sérgio Arouca Public Health National School Committee (number686.868). The participants, who spontaneously accessed the ambulatory of gynecology attending in a Public Family Health Program, were randomly selected and interviewed. All women were submitted to clinical and socio-demographic investigation.
Questionnaire
The responders without a previous history of immunosuppressive disease, not pregnant and sexually active regardless of age were included in the cohort. The women who had been vaccinated against HPV and have had intraepithelial lesions or neoplasia were not considered eligible for enrolment in this study. HPV educational leaflet was developed to facilitate the participation of invited women. About 18 demographic and socio-economics characteristics were used in the questionnaire. The profile was measured based on biological variables age, ethnic group, familiar income, education, marital status, number of partners, alcohol use, tobacco smoking, abortion, sexual transmitted diseases (STD), oral anti-contraceptive and condom use of the female population.
Molecular screening
About 100 cervical cell scrapings were collected with a cervical cytobrush from the ecto- and endo-cervix of the uterus during the gynecological examination. The clinical samples were immersed in 10mM Tris buffer, and stored at -20 °C. DNA extraction was performed using Qiagen DNA extraction Kit. In order to evaluate the viral DNA quality, swab samples were performed by β-globin PCR primers (PC04/GH20). The presence of DNA-HPV was detected by PCR amplification (450bp) using consensus primers (MY09/MY11) [20] and Nested PCR (GP5+/GP6+) [3]. After nucleic acid amplification directed to a conserved region of the HPV L1 gene, high-risk type specific primers (HPV16/18/31/45) were performed for genotyping. In addition, polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) assay patterns of L1 PCR products were used for genotyping including four restriction endonucleases (PstI, HaeIII, DdeI and RsaI).
Statistical analysis
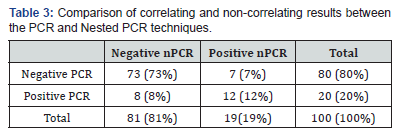
Statistical analysis using the Chi-square test was applied in order to analyze the risk factors associated with HPV infection in 18 socio-demographic variables obtained from informative questionnaires. The data were stored in an Excel spreadsheet and the association between nominal variables and the positive outcome for HPV was performed by Fisher’s exact test or χ2. To determine the correlation between the methods of diagnosis of HPV (PCR and Nested PCR) the Kappa test was tested. Thus, the low correlation attributed for Kappa values were between 0.00 and 0.20, fair correlation had values between 0.21 and 0.40, moderate correlation was between 0.41 and 0.60, good correlation had values between 0.61 and 0.80, and excellent correlation had values between 0.81 and 1.00.
Results
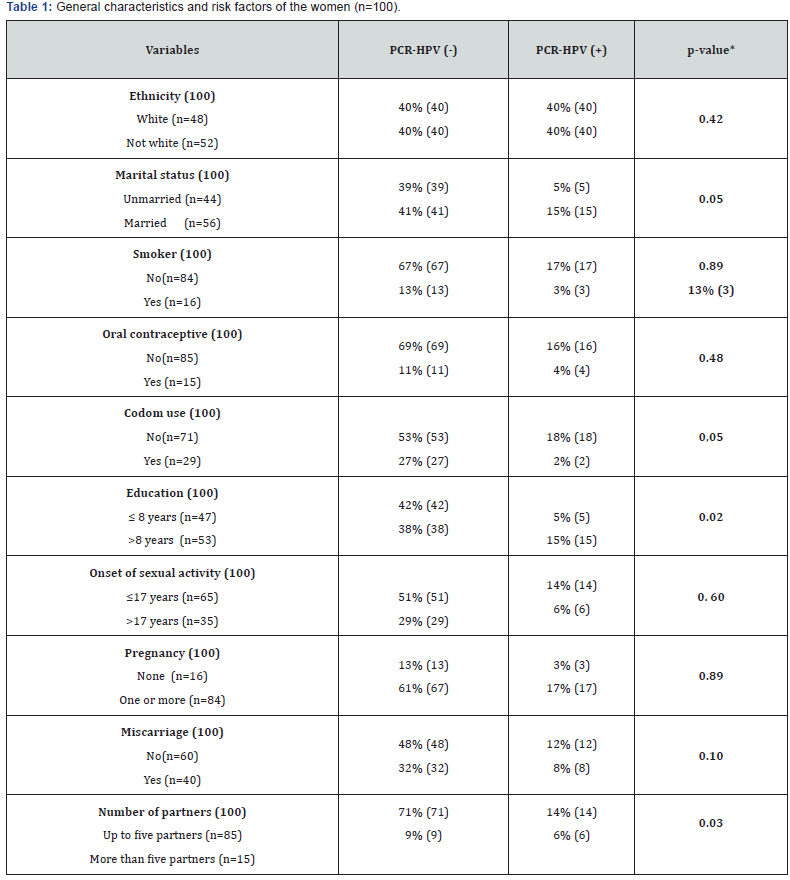
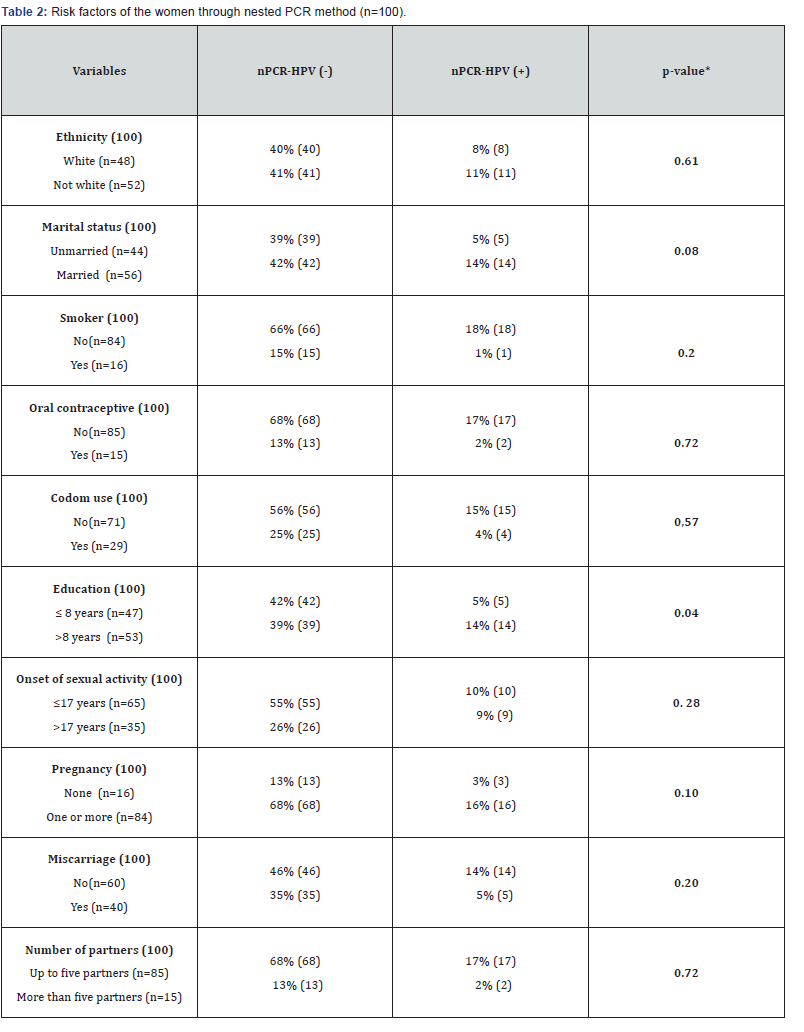
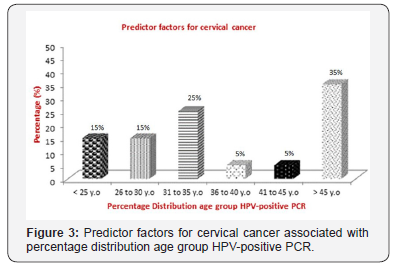
In order to verify HPV infection, this cross-sectional design study demonstrated by using the Chi-square test that of the 100 participants, 20% (95% CI: 12-28) were DNA HPV positive. HPV 18 and 45 were the most frequently detected HPV types. Of these, 8% were amplified by HPV18/45 indicating co-infection (5% HPV18 and 3% HPV18/45); and 12% were undetermined types. HPV16 and 31 types were not detected to none of the samples tested. A group of100 women was divided into six aged groups (≤25 y.o [15%, 95% CI]; 26 to 30 y.o [15%, 95% CI]; 31 to 35 y.o [25%, 95% CI]; 36 to 40 y.o [5%, 95% CI]; 41 to 45 y.o [5%, 95% CI]; ≥45 y.o [35%, 95% CI]). Distribution among racial/ethnic groups was representative when 47% of women were white and 53% were black and on the race/ethnicities. About 16% reported being smokers and 3% drug users. Of all the participating, 27% used alcoholic, 40% reported having had at least one abortion, 15% used oral contraceptives, while 71% did not use any type of condom (p<0.03).Most women were currently not married (56%) and married or cohabitating (44%) (p<0.05).Psychosocial and psychosexual issues demonstrated that six percent of the women exhibit history of sexually transmitted diseases, except HIV, with 85% of women having sex with until to five partners (p<0.03) by chi-squared tests and 14% started sexual activity under the age 17 (Table 1 & 2) (Figure 1 & 2).
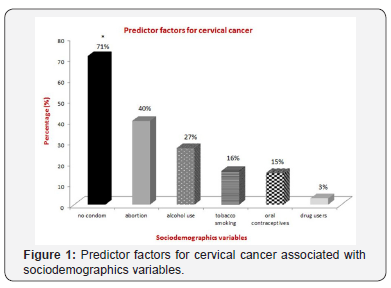

About the employment status of all the participating women, 90% reported having had at least one until four basic salaries. Only 5% women have had higher education. The most women (87%) have had secondary and fundamental education. Comparing the genotypes, 37.5% were predominately over 45 years old, 62.5% of respondents were HPV18 positive and married and/or of cohabitation matrimonial status, 62.5% don´t smoke; all of them don´t use drugs and alcohol, four patients (50%) have monthly income between one to four minimum wages, 37.5% started sexual activity before the age of 17 years and 50% had less than five sexual partners (Figure 3).
Twenty five percent of the patients have had multiple infections (HPV18/45) and were unmarried. The 3% who have had the both types of HPV infection had more than five sexual partners. A highly significant factor associated with HPV infection was who did not use the condom and had an income between one to four minimum wages, both with 87.5%. A previous history of STD was not significantly related. Cytological status was without alterations in the population investigated.
According to the results, we evaluated the correlation and/ or non-correlation between the samples analyzed. Between the PCR and nested PCR techniques, there are 12% (12 samples) correlation between the samples identified as positive and 73% (73 samples) correlation between the negative. Non-correlation was found in 7% (7 samples) samples of negative PCR, whereas the nested PCR showed to be positive, and 8% (8 samples) showed positive PCR and negative nPCR. This demonstrates that there is a moderate correlation between the techniques according to the Kappa association test (k:0.52). PCR-RFLP techniques demonstrated some limitations (Table 3).
Discussion
Our study analyzed only pre-immunization women at six different age groups compared with Mesheret al. (2014). The high-risk HPV prevalence of our study was 20% detected only in swab samples collected with a cervical cytobrush when compared with specimen types of Scotland women from urine, self-taken swab and liquid based cytology samples [18].
Italian women with normal cytology were DNA positive also of HPV by PCR amplification [7] when compared with our results in unimmunized Brazilian women without cytological damage. Similar to Rahman et al. [10] in a United States study, our study analyzed some different variables about demographic and social behaviors also. Our cross-sectional study detected 20% prevalence in cervical swab samples similar to the HPV prevalence of Tristão et al. [11] but not associated with the oral mucosa.
We analyzed several variables stratified by six age groups, but the vaginal pH was not included in our study. Semistructured interviews were made by school nurses about HPV vaccine implementation [21]. There were no significant associations between vaginal pH and detection of HPV at the post-menopausal age ranges (55-64 years old) in a Costa Rica study. Over 65 y.o, strong association between a vaginal pH >5.0 and carcinogenic HPV positivity was reported by Clarke et al. [14]. Co-infections were also detected in younger women in our study, but the HPV16 was not detected as in the Greece population by Argyri et al. [13].
Percentages of cervical cancer screening, mortality and hysterectomyzed population were excluded as disease model parameters in our study differently when compared with Kawai et al. [16] analyzing the health and economic impact of HPV vaccination in Brazil. Cost-effectiveness of the bivalent and quadrivalent HPV vaccine associated with the vaccine price per dose, duration of protection by years, relative risk reduction of unvaccinated women and discount rate health effects was described by Westra et al. [15].
Conclusion
Our study estimated the prevalence of HPV in unvaccinated active women in the Manguinhos Habitation Complex, Rio de Janeiro, Brazil. This epidemiological study showed a strongly association among the presence of DNA HPV genital types with risk factors to cervical cancer in unimmunized women and of free clinical lesions. Socio-demographic characteristics as behavior changes and covariables associations related to sexual health were significantly relevant in women without cytological abnormalities. The data from this study recorded the prevalence of high-risk HPV genotypes.
This paper contributed to a better understanding about the natural history of HPV from a pre-immunization prevalence study of active sexually and free lesions clinical women in Brazil. These results showed the importance of the cofactors for progression and persistence of HPV infection and may be useful to future epidemiological surveillance reports, educational intervention and evaluation of new clinical and subclinical cases of cervical intraepithelial neoplasia and genital warts. A large challenge to public health is the cancer prevention in populations from developing countries with high risk exposure associated with the history of other STDs in different geographic regions. So, public health programs should to encourage the vaccination emphasizing the effectiveness of the vaccine as part of general HPV vaccine recommendations.
Acknowledgement
This research was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES)/“Brasil Sem Miséria”Program and theConselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). The authors thank Dra. Maria Glória Bonecini and her team for technical contributions.
References
- Centers for disease control and prevention (2004) Genital HPV infection fact sheet. CDC: National Prevention Information Network.
- Simões RSQ, Barth OM (2015) Papillomavirus: Viral vectors in the gene therapy and new therapeutic targets. International Journal of Biomedical Research 6(10): 763-768.
- Simões RSQ, Barth OM (2017) Immunological and structural analysis of HPV-positive cervical carcinoma cell lines and bovine papillomavirus virus-like particles (BPV-VLP). International Journal of Advanced Research 5(4): 1003-1009.
- Hendry M, Lewis R, Clements A, Damery S (2013) “HPV? Never heard of it!”: A systematic review of girls´ and parents´ information needs, views and preferences about Human papillomavirus vaccination. Vaccine 31(45): 5152-5167.
- Guerry SL, De Rosa CJ, Markowitz LE, Walker S, Liddon N, et al. (2011) Human papillomavirus vaccine initiation among adolescent girls in high-risk communities. Vaccine 29(12): 2235-2241.
- Figueredo ARR, Turchi MD, Santos LE, Guimarães EMB, Garcia MMD, et al. (2013) Prevalence, genotype profile and risk factors for multiple Human papillomavirus cervical infection in unimmunized female adolescents in Goiânia, Brazil: a community-based study. BMC Public Health 13:1041.
- Panatto D, Amicizia D, Tanzi E, Bianchi S, Frati ER, et al. (2013) Prevalence of Human papillomavirus in young Italian women with normal cytology: how should we adapt the national vaccination policy? BMC Infect Dis 13:575.
- Kavanagh K, Sinka K, Cuschieri K, Love J, Potts A, et al. (2013) Estimation of HPV prevalence in young women in Scotland; monitoring of future vaccine impact. BMC Infect Dis 13:519.
- Mesher D, Soldan K, Howell-Jones R, Panwar K, Manyenga P, et al. (2014) Reduction in HPV 16/18 prevalence in sexually active young women following the introduction of HPV immunization in England. Vaccine 32(1): 26-32.
- Rahman M, Elam LB, Balat MI, Berenson AB (2013) Well-woman visit of mothers and Human papillomavirus vaccine intent and uptake among their 9-17 year old children. Vaccine 31(47): 5544-5548.
- Tristão W, Ribeiro RMP, Oliveira CA, Betiol JC, Bettini JSR (2012) Epidemiological study of HPV in oral mucosa through PCR. Braz J Otorhinolaryngol 78(4): 66-70.
- Machado AP, Almeida FG, Bonin CM, Prata TTM, Ávilla LS, et al. (2014) Presence of highly oncogenic Human papillomavirus in the oral mucosa of asymptomatic men. Braz J Infect Dis 18(3): 266-270.
- Argyri E, Papaspyridakos S, Tsimplaki E, Michala L, Myriokefalitaki E, et al. (2013) A cross sectional study of HPV type prevalence according to age and cytology. BMC Infect Dis 13:53.
- Clarke MA, Rodriguez AC, Gage JC, Herrero R, Hildesheim A, et al. (2012) A large, population-based study of age-related associations between vaginal pH and Human papillomavirus infection. BMC Infect Dis 12:33.
- Westra TA, Stirbu-Wagner I, Dorsman S, Tutuhatunewa ED, Vrij EL, et al. (2013) Inclusion of the benefits of enhanced cross-protection against cervical cancer and prevention of genital warts in the costeffectiveness analysis of Human papillomavirus vaccination in the Netherlands. BMC Infect Dis 13:75.
- Kawai K, Araujo GTB, Fonseca M, Pillsbury M, Singhal PK (2012) Estimated health and economic impact of quadrivalent HPV (types 6/11/16/18) vaccination in Brazil using a transmission dynamic model. Bio Med Central Infectious Diseases 12:250.
- Uusskula A, Muursepp A, Kawai K, Raag M, Jurisson M, et al. (2013) The epidemiological and economic impact of a quadrivalent human papillomavirus (HPV) vaccine in Estonia. BMC Infect Dis 13:304.
- Cubie HA (2013) Diseases associated with Human papillomavirus infection. Virology 445(1-2): 21-34.
- Huber B, Schellenbacher C, Shafti-Keramat S, Jindra C, Christensen N, et al. (2017) Chimeric L2-Based Virus-Like Particle (VLP) Vaccines Targeting Cutaneous Human papillomaviruses (HPV). Plos One, 12(1):e0169533.
- Forslund O, Antonsson A, Nordin P, Hansson BG (1999) A broad range of Human papillomavirus types detected with a general PCR method suitable for analysis of cutaneous tumors and normal skin. Journal of General Virology 80(Pt 9): 2437-2443.
- Brabin L, Stretch R, Roberts SA, Elton P, Baxter D, et al. (2011) The school nurse, the school and HPV vaccination: A qualitative study of factors affecting HPV vaccine uptake. Vaccine 29(17): 3192-3196.