Randomized Controlled Clinical Trial on the Provision of the EMDR-PRECI to Family Caregivers of Patients with Autism Spectrum Disorder
Mónica Encinas1, Amalia Osorio1, Ignacio Jarero2* and Martha Givaudan2
1Department of Research, Ágape, Psycho-Oncology and Research Center, Puebla, Mexico
2Department of Research, Mexican Association for Mental Health Support in Crisis, Mexico City, Mexico
Submission: February 28, 2019; Published: March 19, 2019
*Corresponding author: Ignacio Jarero, Department of Research, Mexican Association for Mental Health Support in Crisis, Mexico City, Mexico
How to cite this article:Mónica Encinas, Amalia Osorio, Ignacio Jarero, Martha Givaudan. Randomized Controlled Clinical Trial on the Provision of the EMDRPRECI to Family Caregivers of Patients with Autism Spectrum Disorder. Psychol Behav Sci Int J. 2019; 11(1): 555802. DOI: 10.19080/PBSIJ.2019.11.555802
Abstract
This randomized controlled clinical trial aimed to evaluate the effectiveness of the eye movement desensitization and reprocessing Protocol for Recent Critical Incidents and Ongoing Traumatic Stress (EMDR-PRECI) in reducing posttraumatic stress disorder (PTSD), anxiety and depression symptoms in family caregivers of patients with autism spectrum disorder (ASD). Participants were randomly assigned to six 60-minute individual treatment sessions (N=14) or to care as usual control condition (N=12).
They completed pre, post, and follow up measurements PCL-5 and HADS, while participants continued taking care of their relatives with ASD, during the follow-up. Data analysis by repeated measures ANOVA revealed a significant effect for time, for group and interaction for PSTD and Anxiety: (F (2, 46) = 16.99 p <.001, ηP2 = .425), (F (1, 23 = 6.61, p<.01, ηP2 = .223), (F (2, 46) = 30.42, p <.001, ηP2 = .569); (F (2, 46) = 8.92, p <.001, = ηP2= .280), (F (2, 23) = 7.36, p <.05, ηP2 = .242), (F (2, 46) = 11.33, p <.001, ηP2= .330) respectively, and significant effect for time (F (2, 46) = 4.35, p <.05, ηP2 = .159) and interaction (F (2, 46) = 4.64, p <.05, ηP2 = .168) with no significant effect for group for depression. The study results suggest that the EMDR-PRECI could be an efficient and effective treatment to address family caregiver’s PTSD, anxiety and depression symptoms. Future research with randomized controlled clinical studies is recommended to replicate these results with a larger sample size of family caregivers of patients with ASD.
Keywords: Eye Movement Desensitization and Reprocessing; PRECI; Care Givers; Autism Spectrum Disorder (ASD); Posttraumatic Stress Disorder (PTSD); Anxiety; Depression.
Introduction
The Diagnostic and Statistical Manual of Mental Disorders fifth edition [1] classifies Autism Spectrum Disorder (ASD) as a neurodevelopmental disorder. The description of ASD includes difficulties in communication and social interactions, as well as restricted and repetitive behaviors and interests as its main features. People with ASD may present hypersensitivity, sleep disturbances, behavioral difficulties, and eating disorders, among other symptoms that may affect the day-to-day family dynamics and can cause a significant direct emotional impact on every family member. The World Health Organization (WHO) [2] estimates that 1 out of every 160 children in the world are diagnosed with ASD, while the Center for Disease Control and Prevention [3] says that 1 out of every 59 children with ASD have been identified.
Family caregivers of children with ASD face challenges in their day-to-day parenting activities which often cause higher stress levels compared to other groups of parents [4]. According to Stewart et al. [5] disruptive behaviors of some ASD-diagnosed children impact the parenting experience causing high distress levels along with other symptoms associated with depression, anxiety, somatization and hostility. Other researchers [6-8] found similar results including the presence of high stress levels and anxiety episodes and emphasized that parents of ASD-diagnosed children require specific interventions for the management of these symptoms.
The WHO [2] has pointed out the need to design plans and programs to provide support to family members of individuals that have been diagnosed with ASD. The WHO Guidelines on Mental Health Care After Traumatic Events [9], considers a traumatic event that directly affects an individual to be, in turn, regarded as a source of trauma for close relatives. As a result, primary caregivers of ASD-diagnosed persons could present posttraumatic stress disorder (PTSD) symptoms themselves and require the proper attention.
EMDR Therapy
Eye movement desensitization and reprocessing (EMDR) therapy [10,11] and trauma-focused Cognitive Behavioral Therapy (TF-CBT) are the only psychotherapies recommended for children, adolescents, and adults with PTSD in the WHO Guidelines for the Management of Conditions Specifically Related to Stress [12]. EMDR therapy is a structured eight-phase comprehensive approach that addresses the past, present, and future aspects of distressing memories of adverse life experiences. Processing occurs as patients focus on elements of the distressing memory while engaging simultaneously in bilateral stimulation
EMDR Therapy Administered to Caregivers
Passoni et al. [13] investigated the effectiveness of the EMDR integrative Group Treatment Protocol (EMDR-IGTP) on the “caregiver syndrome.” Forty-four primary caregivers entered the study. They were randomly assigned to either the “immediate” branch, who received the treatment soon after recruitment, or to the “delayed” branch, who received it two months after recruitment. The treatment consisted of eight group sessions (one per week). Emotional distress was measured before the treatment, immediately after the end of it, and two months later (follow-up), by means of several clinical scales. These preliminary results show for the first time that EMDR-IGTP reduces stress-related symptoms, anxiety, and depression in caregivers of patients with dementia. Castelli [14] examined the use of EMDR therapy in a rehabilitation center to deal with traumatic experiences associated with serious incapacitating disease. Also explored were the importance of EMDR therapy in helping to facilitate secure attachment relationships between patients and their caregivers. EMDR therapy appears to offer specific advantages in treating this especially difficult population, affording patients who live with a chronic condition of extreme physical vulnerability a sense of greater control over their own bodies and therefore over their own lives.
EMDR-PRECI
The EMDR Protocol for Recent Critical Incidents and Ongoing Traumatic Stress (EMDR-PRECI) [15] was developed in the field to treat recent (even hours after a trauma) or prolonged adverse experiences where related stressful events continue for an extended time and where there is no post-trauma safety period for traumatic memory consolidation. Jarero & Artigas [16] hypothesized that often, as a result of this ongoing lack of safety, the consolidation of the traumatic memory network is prevented. Therefore, the continuum of external adverse experiences creates a cumulative trauma exposure memory network [17] of linked pathogenic memories [18] with similar emotional, somatic (body sensations), sensorial (the five senses), and cognitive information (thoughts and beliefs), that extends into the present moment, and often producing maladaptive/catastrophic concerns about the future or flash-forwards [19]. Shapiro [11] recommends the EMDR-PRECI “for an extended post-disaster period to address situations in which there is ongoing trauma and therefore no subsequent period of safety” (p. 397). For more information about this protocol see Jarero, et al. [15].
EMDR-PRECI Previous Studies
i. After a 7.2-magnitude Earthquake: In this randomized controlled trial (RCT) using a delayed treatment-controlled design, 18 adults were treated within 30 days following a 7.2 earthquake in North Baja California, Mexico in 2010 by means of a single (80- to 130-minute) session of EMDR-PRECI [15]. Despite frequently occurring aftershocks, both groups (immediate-treatment group and delayed-treatment control group) showed substantial (30 points) reductions of trauma symptoms on the Impact of Events Scale [20], effects that were maintained at a 12-week follow-up. No participant developed PTSD during this period.
ii. After a Human Massacre: In this delayed treatment control design, a single EMDR-PRECI [21,22] individual session (90-120 minutes) was provided within 8 weeks postevent to 32 first responder forensic personnel who were collecting body parts following a massacre of hundreds of people. Results showed significant improvement for both immediate treatment (N=18) and waitlist/delayed treatment (N= 14) groups on the Impact of Events Scale [20] and Short PTSD Rating Interview (SPRINT) [23,24]. Follow-up scores at 3- and 5-months posttreatment showed that the original treatment results were maintained, with a further significant reduction of self-reported symptoms of posttraumatic stress and PTSD between posttreatment and follow-up. This study suggests that EMDR-PRECI was an effective early intervention, reducing traumatic stress for a group of traumatized adults continuing to work under extreme stressors in a human massacre situation. It appears that the treatment may have helped to prevent the development of chronic PTSD and to increase psychological and emotional resilience.
iii. After a Technological Disaster: In this RCT [25] using a delayed treatment-controlled design, the EMDR-PRECI was administered within 34 days of an explosion in an explosives manufacturing factory in Mexico that killed 7 employees. Twenty-five survivors who had posttraumatic stress symptoms related to the critical incident received two 60-minute sessions on consecutive days. Initial scores for both groups were in the severe range for trauma symptoms, as measured by the SPRINT [23,24] and decreased to low levels after treatment (from 22 to 2). Treatment effects were maintained 106 days after the explosion, and no participant developed PTSD during this period.
iv. With First Responders in Active Duty: In this RCT [26] 60 first responders were randomly assigned to two 60-minute individual treatment sessions (N=30) or to a notreatment control condition (N=30). They completed pre, post, and follow up measurements using the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) [27,28] and the Hospital Anxiety and Depression Scale (HADS) [29,30]. Data analysis by repeated measures ANOVA showed clear effects of the EMDR-PRECI in reducing PTSD work-related symptoms in the treatment group with symptom reduction maintained at 90-day follow-up with a large effect size (d=3.99), while participants continued to experience direct exposure to potentially traumatic work-related events during the follow-up period. The study results suggest that the EMDR-PRECI could be an efficient and effective way to address first responders’ work-related PTSD, anxiety and depression symptoms.
Objective
The objective of this study was to evaluate the effectiveness of the EMDR-PRECI in reducing PTSD, depression, and anxiety symptoms in family caregivers of patients with autism spectrum disorder (ASD).
Method
Study Design
To measure the effect of EMDR-PRECI on the dependent variable’s PTSD, Anxiety, and Depression, this study used a randomized control study design, comparing treatment and care as usual (information about ASD and training parents in the management of their children’s behaviors with no intervention of the study therapist) control groups. Symptoms of PTSD were measured in three-time periods: Time 1 pretreatment, Time 2 post-treatment, and Time 3 follow-up. Symptoms of anxiety and depression were measured at time 1 pretreatment and time 3 follow-up.
Ethics and Gold Standards
The research protocol was reviewed and approved by the EMDR Mexico International Research Ethics Review Board in compliance with the International Committee of Medical Journal Editors recommendations, the Guidelines for Good Clinical Practice of the European Medicines Agency (version 1 December 2016) and the Helsinki Declaration as revised in 2013. The research quality of this study partially fulfilled the criteria of the Revised Gold Standard scale [31] items. These included: (a) target symptoms were clearly defined, but without diagnosis, (b) measures were reliable and valid, (c) blind independent evaluators collected posttreatment measures at Times 2 and 3; (d) assessor reliability was checked by M.G., (e) treatment was manualized, (f) blind random assignment was conducted, (g) treatment fidelity was evaluated by supervisors, (h) no conditions were confounded, (i) multimodal measures were not used, and (j) length of treatment was appropriate for civilian participants with single trauma (five or more sessions).
Participants
This study was conducted in 2018 in the city of Puebla, Mexico at the “Ágape Desarrollo Humano Integral” Center installations. Potential participants were recruited through social networks such as Facebook and Whatsapp. The information was sent through WhatsApp groups of centers dedicated to the treatment of ASD, as well as other parent’s support networks. People interested were asked to call by phone to receive the details of the research project. A total of 46 potential participants called and received the information. Of those, 26 were able to attend the personal interview. The other 18 could not find the time or arrange for a person to take care of their relative with ASD and were therefore not able to attend the interview. All 26 persons that attended the intake interview fulfilled the inclusion criteria.
a. Inclusion criteria were: (a) to be the primary family caregiver of a person diagnosed with ASD, (b) to be an adult, (c) to not be receiving psychotherapy, (d) to not be receiving drug therapy, (e) be have the time availability to attend the interviews and treatment in the city of Puebla.
b. Exclusion criteria were: (a) ongoing self-harm/suicidal or homicidal ideation, (b) diagnosis of psychotic or bipolar disorder, (c) diagnosis of dissociative disorder, (d) organic mental disorder, (e) current, active chemical dependency problem, (f) significant cognitive impairment (e.g., severe intellectual disability, dementia).
Twenty-six participants (1 male and 25 females) all mothers and one stepfather of persons with ASD diagnosis (26 males and 2 females) met the inclusion criteria. The age of participants ranged from 29 to 61 years old (M=39.8 years). The age of the persons with ASD ranged from 2 to 33 years (M=10.3 years). Participation was voluntary with a signed informed consent form.
Randomization and Blinding Procedure
Participants were randomly selected to a treatment group or care-as-usual control group using a computer-generated randomnumber list. Two independent assessors blind to treatment conditions conducted the randomization process to avoid allocation influence. Participants were contacted by phone by an administrative assistant that was not part of the study to inform them if they belonged to the treatment group or the control group. Patients in the care-as-usual control group were informed that, for ethical reasons, they would receive the treatment after the study was concluded. The randomization group allocation was masked to the research assistants and to the independent assessors in charge of the assessments at post and follow-up times. There were 14 participants in the treatment group and 12 participants in the control group.
Instruments
We used the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) [27,28] Spanish version provided directly by the National Center for PTSD (NCPTSD) and adapted, with the NCPTSD approval, for the past week instead of the past month symptoms to conduct research with a high mobility population. It contains 20 items, including three new PTSD symptoms (compared with the PTSD Checklist for DSM-IV): blame, negative emotions, and reckless or self-destructive behavior. Respondents indicate how much they have been bothered by each PTSD symptom over the past week (rather than the past month), using a 5-point scale ranging from 0=not at all, 1=a little bit, 2=moderately, 3=quite a bit and 4=extremely. A total-symptoms score of zero to 80 can be obtained by summing the items. The sum of the scores yields a continuous measure of PTSD symptom severity for symptom clusters and for the whole disorder. Psychometrics for the PCL-5, validated against a CAPS-5 PTSD diagnosis, suggest that a score of 31–33 is optimal for determining probable PTSD [28]. The PCL-5 is intended for a variety of clinical and research assessment tasks, including quantifying PTSD symptom severity, measuring the underlying construct of PTSD, establishing a provisional PTSD diagnosis, and estimating presumed prevalence of PTSD. It is important to mention that at the first assessment time, before answering the PCL-5, all participants were asked to focus specifically on the worst family caregiver-related event that currently bothered them the most; then at each subsequent assessment time, they were asked to focus on the same event.
The Hospital Anxiety and Depression Scale (HADS) [29] has been extensively used to evaluate these psychiatric comorbidities in various clinical settings at all levels of healthcare services and with the general population [30]. It is a 14 item self-report scale to measure the anxiety (7 items) and depression (7 items) of patients with both somatic and mental problems using a 4-point Likert scale ranging from 0 to 3. The response descriptors of all items are Yes, definitely (score 3); Yes, sometimes (score 2); No, not much (score 1); No, not at all (score 0). A higher score represents higher levels of anxiety and depression: a domain score of 11 or greater indicates anxiety or depression; 8–10 indicates borderline case; 7 or lower indicates no signs of anxiety or depression.
Procedure
Assessments Times, Data Collection and Confidentiality of Data
Treatment and control group participants completed the instruments on an individual basis in the different measurement moments. During time 1, five research assistants, all licensed EMDR clinicians trained by the fourth author (MG) in instrument administration, general interview techniques, and ethical research behavior, collected clinical histories, signed informed consent forms, provided psycho-education and answered participants questions related to trauma, PTSD, anxiety, depression and EMDR therapy to decrease any possible prejudice against the treatment. Application of instruments for both groups was done after this procedure by the same research assistants who were not blind to the study but blind to the treatment allocation.
During Time 2 (post-treatment assessment) and Time 3 (follow-up assessment 90 days after treatment) assessment was conducted for all participants by blind independent assessors with a master’s degree in clinical psychology who were not part of the study. All data was collected, stored, and handled in full compliance with the EMDR Mexico International Research Ethics Review Board requirements to ensure confidentiality. Each study participant gave their consent for access to their personal data,which was strictly required for study quality control. All persons involved in this research project are subject to professional confidentiality.
Withdrawal from the Study
All research participants had the right to withdraw from the study without justification at any time and with assurances of no prejudicial result. If participants decided to withdraw from the study, they were no longer followed up in the research protocol. There were no withdrawals from this study.
Treatment
In this study, intensive EMDR therapy [32-34] was provided due to the necessity of participants’ work as caregivers. This intensive format allowed the participants to complete the full course of treatment in a short time period. Participants completed a total of six 1-hour sessions provided during three consecutive days twice a day.
Therapists and Treatment Fidelity
EMDR-PRECI was provided by ten licensed EMDR clinicians formally trained in the protocol administration, none of them authors of this study. Treatment fidelity and adherence to the protocol was fulfilled by EMDR therapists’ strict observance to all steps of the scripted protocol while they were evaluated by three supervisors who observed 50% of sessions, randomly assigned.
EMDR-PRECI Treatment Description
Each of the treatment group participants received a total of six 1-hour individual treatment sessions, twice daily during three consecutive days in a setting inside the Ágape Center. EMDRPRECI treatment focused only on the distressing memories related to their work as family caregivers of patients with ASD and did not address any other memories. To encompass the whole ongoing traumatic stress spectrum, clinicians asked each of the treatment group participants to remember the worst event that they selected during the PCL-5 assessment. Once the clients had reprocessed the worst event, clinicians asked them to run a mental movie of the whole experience as family care givers of patients with ASD from right before the beginning until today, or even into the future, and then to identify any other disturbing parts/ memories. All participants reprocessed more than one memory. The average of memories reprocessed was four. No adverse effects were reported during treatment or at 90-day follow-up.
Examples of Worst Experiences Reprocessed During Treatment
The worst experiences reported by family caregivers are grouped in: a) the time they received the diagnosis of their children, b) day-to-day disruptive behaviors such as tantrums in public, c) beliefs and judgments of people about child behavior, d) concern about the future, e) the uncertainty of knowing if their children will be independent and safe, and in one case, suicide attempt.
Specific Examples
1) “When he tried to commit suicide by putting a fork in the light contact”; 2) “When people do not believe he has ASD and relate it (the behavior) to lack of limits”; 3) “When he was aggressive with his brother and was about to break his arm”; 4) “The moment I knew the diagnosis, I couldn’t bear the news”; 5) “Constant fear that he cannot do anything with his life or that he might commit suicide”; 6) “One day he defecated and spread it on the walls, floor, and toys, and I hit him in front of his brother”; 7) “That someone could be physically or emotionally abusive to my son”; 8) “The late diagnosis and the anger for not having requested the complete assessments before”; 9) “Fear that my son cannot be self-sufficient”; 10) “When he lost control and threw a chair at school”; 11) “When people at school asked me to take my son somewhere else”; 12) “My death, him being alone and becoming a beggar”; 13) “The therapist telling me that I had to take my son to therapy every day because he had only one year to stimulate his development”; 14) “He put his life at risk almost every day because he did not measure danger.”
Statistical Analysis
Analysis of variance (ANOVA) for repeated measurements was used with three-time points for PTSD, anxiety, and depression. Analyses included two groups (treatment group = 14 subjects, and no-treatment control group =11 subjects) as independent variables and PTSD, anxiety, and depression as dependent variables. Effect size estimates are reported through eta square. Cohen’s d was calculated to report the effect size of the significant results of the t-test when comparing means.
Results
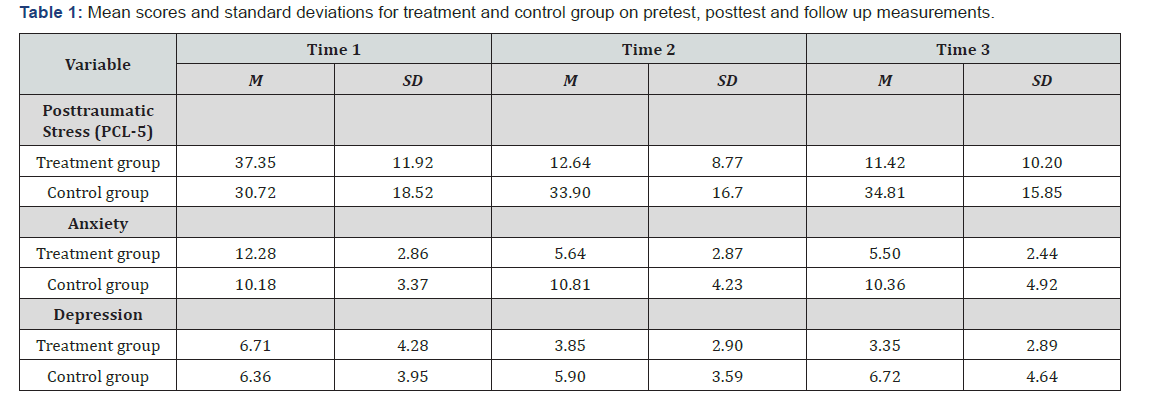
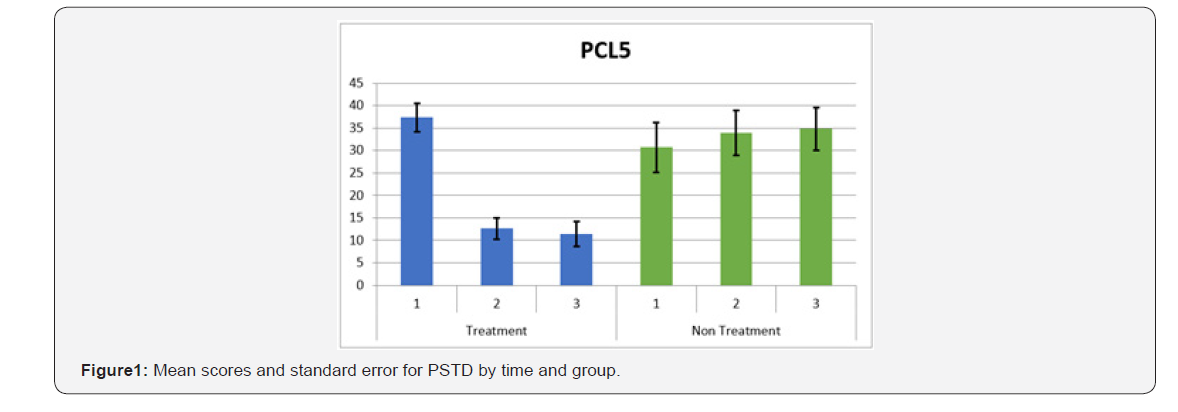
PTSD (PCL-5). Data analysis by repeated measures ANOVA revealed a significant effect for time (F (2, 46) = 16.99 p <.001, ηP2 = .425), a significant effect for group (F (1, 23 = 6.61, p<.01, ηP2 = .223) and a significant interaction between time and group, (F (2, 46) = 30.42, p <.001, ηP2 = .569). In the treatment group, mean scores showed a significant decrease between time 1 and time 2, t (13) = 5.50, p<.001, d=1.67. In the no-treatment control group no significant differences were found between means in all comparisons. Comparison between groups did not show significant differences for time 1. For time 2 and 3 significant differences among the groups were founded, t (23) = - 4.11, p <.01, d = -1.65 and t (23) = - 4.47, p <.01, d = -1.80 respectively Table 1 & Figure 1.
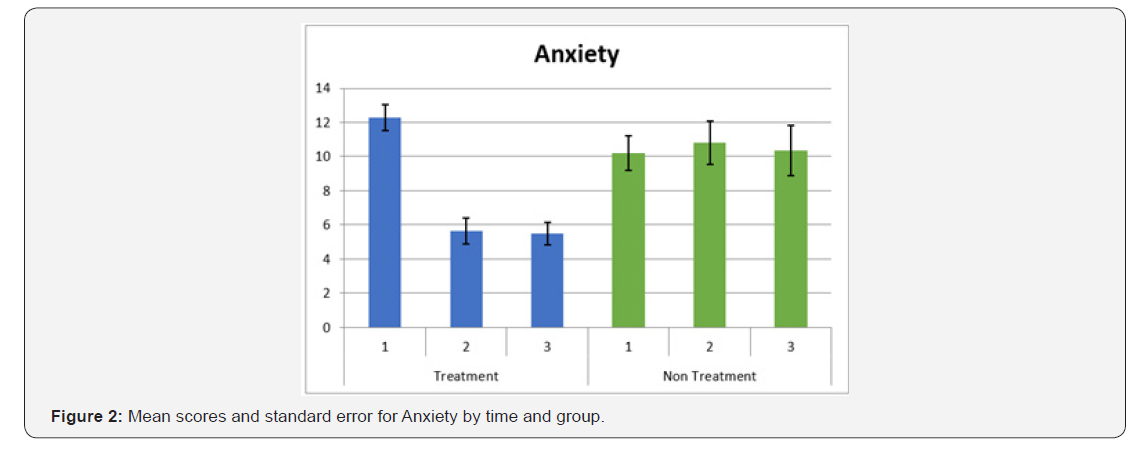
Anxiety. Repeated measures analysis of variance (ANOVA) showed a significant effect for time (F (2, 46) = 8.92, p <.001, = ηP2= .280), significant interaction effect between time and group (F (2, 46) = 11.33, p <.001, ηP2= .330) and significant effect for group (F (2, 23) = 7.36, p <.05, ηP2 = .242) for anxiety. Significant differences between time 1 and time 2 were found for the treatment group, t (13) = 5.77, p<.001, d=1.63. No significant differences were observed in the no-treatment control group between different time applications. Comparison between groups showed significant differences comparing post and follow up measurements t (23) = -3.63, p<.001, d= -3.73 and t (23) = 3.23, p< .05, d= -1.30, respectively Table 1 & Figure 2.
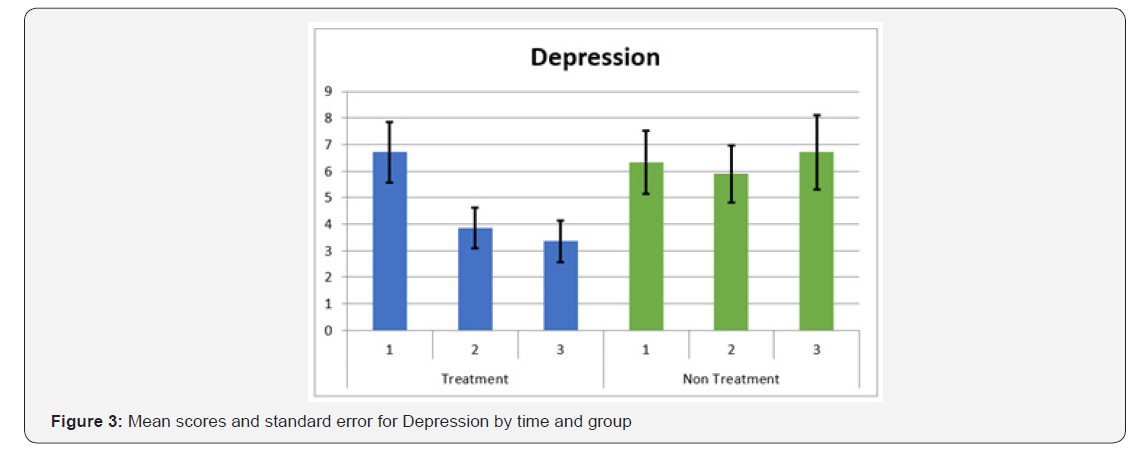
Depression. Results showed significant effect for time (F (2, 46) = 4.35, p <.05, ηP2 = .159) and significant interaction effects between time and group. (F (2, 46) = 4.64, p <.05, ηP2 = .168). No significant effect for group was founded. For the treatment group significant differences were found between time 1 and time 2, t (13) = 2.60, p<.05, d= .55). In the control group, no significant differences were found between means in all comparisons. Comparison between groups showed significant differences for time 3, t (23) = - 2.22, p <.05, d =.89 Table 1 & Figure 3.
Discussion
Significant effects for time and significant interaction effects were found for PTSD symptoms, anxiety and depression after the treatment. Significant effects for group were found for PTSD and anxiety but not for depression. The effect sizes, calculated with Cohen’s d, are large for PSTD and anxiety comparing prepost measurements for the treatment group and the effect size for depression is medium. These results show the effect of the treatment on all the dependent variables and showed clearly the decrease of scores from pretest to posttest which was maintained in the follow up. In the cases with significant differences between groups, all the effect sizes are large. For the control group there was a significant difference between pre and post measurement for PSTD, due to an increase in the symptoms with a small size effect.
According to Roberts et al. [35] there is a strong connection between PTSD and ASD. Results showed that the stress related to parenting a child with ASD could increase the risk for mothers to develop PTSD. Casey et al. [36] conducted a pilot study with parents who had just received the ASD diagnosis for their child and found that 20 percent of their sample reported experiencing PTSD symptoms. Ozturk et al. [37] conducted a study with 99 parents of children with ASD. Their results revealed the gender differences in parental attitudes about mental health. Mothers reported that they engaged in more social behaviors with their children than fathers. In addition, mothers reported higher level of depression than fathers. Bitsika & Sharpley [38] conducted a study with 107 parents of children with ASD. Results showed that over 90% of parents reported that they were sometimes unable to deal effectively with their child’s behavior. Nearly half of the participants were assessed to be severely anxious and nearly two thirds were clinically depressed.
Conclusion
Rearing a child with Autism Spectrum Disorder (ASD) is a unique challenge for family caregivers. It can be exhausting, overwhelming and stressful. Despite the literature which demonstrates that caregivers are at risk for mental, emotional and physical health problems, this population has remained essentially invisible, lacking the effective and supportive psychotherapeutic treatment that could potentially improve their mental, emotional, physical health and well-being. We believe that the intensive administration of the EMDR-PRECI could be an efficient and effective part of an integral approach to reduce care-giving related symptoms of PTSD, anxiety and depression, improving the quality of life for both family caregivers and children with ASD.
Limitations
The sample size of the study is a limitation. Therefore, future research with randomized controlled clinical studies is recommended to replicate these results with a larger sample size of family caregivers of patients with ASD.
Acknowledgement
This study was not founded on any grants. We want to express gratitude to the following individuals for their contributions: Lynne Levinson, Ana Gabriela Arriaga, Yael Becker, Milagros Cueto, Carolina Domínguez, Lourdes Fernández, Paola García, Alicia Gómez, Adriana González, Verónica Guillén, Gabriela Jiménez, Miriam Jiménez, María José Millán, María Alicia Peregrina, María Cristina Pérez, María Leticia Picazo, Patricia Ramírez, Pablo Treviño.
Conflict of Interest
All the authors do not have any possible conflicts of interest
References
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, (5th edn.), American Psychiatric Publishing: Arlington, VA, USA.
- Center for Disease Control and Prevention (2014) Prevalence of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report. Surveillance Summaries 63: 1-21.
- Post-Traumatic Stress Disorder (PTSD) (2018) National Institutes of Mental Health, United States.
- van Steensel FJA, van Bögels SM, Perrin S (2011) Anxiety disorders in children and adolescents with autistic spectrum disorders: A metaanalysis. Clin Child Fam Psychol Rev 14(3): 302–317.
- Mehtar M, Mukaddes NM (2011) Posttraumatic Stress Disorder in individuals with diagnosis of Autistic Spectrum Disorders. Res Autism Spectr Disord 5: 539-546.
- De Bruin EI, Ferdinand RF, Meester S, de Nij PFA, Verheij F (2007) High rates of psychiatric comorbidity in PDD-NOS. J Autism Dev Disord 37(5): 877-886.
- Storch EA, Sulkowski ML, Nadeau J, Lewin AB, Arnold EB, et al. (2013) The phenomenology and clinical correlates of suicidal thoughts and behaviors in youth with autism spectrum disorders. J Autism Develop Disord 43(10): 2450-2459.
- Dell’Osso L, Dalle Luche R, Carmassi C (2015) A new perspective in post-traumatic stress disorder: Which role for unrecognized autism spectrum. International Journal of Emergency Mental Health and Human Resilience 17(2): 436-438.
- Nietlisbach G, Maercker A (2009) Social cognition and interpersonal impairments in trauma survivors with PTSD. Journal of Aggression Maltreatment & Trauma 18(4): 382-402.
- Kerns CM, Newschaffer CJ, Berkowitz SJ (2015) Traumatic childhood events and autism spectrum disorder. J Autism Dev Disord 45(11): 3475-3486.
- Stavropoulos K, Bolourian Y, Blacher J (2018) Differential Diagnosis of Autism Spectrum Disorder and Post Traumatic Stress Disorder: Two Clinical Cases. J Clin Med 7(4).
- Trelles Thorne Mdel P, Khinda N, Coffey BJ (2015) Posttraumatic stress disorder in a child with autism spectrum disorder: Challenges in management. J Child Adolesc Psychopharmacol 25(6): 514-517.
- Morries LD, Cassano P, Henderson TA (2015) Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy. Neuropsychiatr Dis Treat 11: 2159-2175.
- Hamblin MR (2016) Shining light on the head: Photo biomodulation for brain disorders. BBA Clin 6: 113-124.






























