What Causes Patient Aggressive Behaviours in Healthcare Settings?
Tawanda Machingura1* and Chris Lloyd2
1Assistant Professor of Occupational Therapy, Bond University, Gold Coast, Australia
2Senior Research Fellow, Griffith University, Gold Coast, Australia
Submission: February 7, 2019; Published: February 25, 2019
*Corresponding author: Tawanda Machingura, Assistant Professor of Occupational Therapy, Faculty of Health Sciences and Medicine, Bond University, Gold Coast, Australia
How to cite this article:Machingura,T., Lloyd,C.. What Causes Patient Aggressive Behaviours in Healthcare Settings?. Psychol Behav Sci Int J. 2019; 10(5): 555796. DOI: 10.19080/PBSIJ.2019.10.555796.
View point
Health staff such as nurses and doctors are often victims of aggressive behaviour displayed by patients in hospital and health care settings particularly dementia units, emergency departments and mental health units. In Australia, there is currently an increased media attention on the topic however employers are still unsure of the causes or how to manage their ever-increasing scourge. The commonly pointed out scape goat has been the use of alcohol and drugs. Although this is a likely culprit it is not the only cause of such behaviours. This paper therefore seeks to examine the causes of patient aggressive behaviours and provide a more critical view to the problem and therefore enable solution focused thinking that actually will work. Research indicates that staff exposure to patient violence leads to poor outcomes for the patients, staff and employers [1]. Staff are more likely to have a lower job satisfaction, emotional exhaustion, cynicism, physical injury and poor psychological wellbeing and employers incur higher costs due to injury claims. Therefore, preventing aggressive behaviours has benefits for staff, patients and employers.
Understanding what causes aggressive behaviours is important for effectively reducing aggressive behaviour incidents in hospital settings. We know from previous studies that aggressive behaviours range from verbal abuse and physical violence to damage to property [2], International Council of Nurses (2009). Current literature generally categorizes risk factors into patient factors, environmental factors, treatment factors and societal factors [1]. We agree with this view but emphasize that these factors are not static but rather interactional. Our view is that in line with systems theory, one factor is hardly the only cause of aggressive behaviour. We argue that aggressive behaviour is the result of an interaction between negative patient, staff, environment and contextual factors as shown in Figure 1 below.
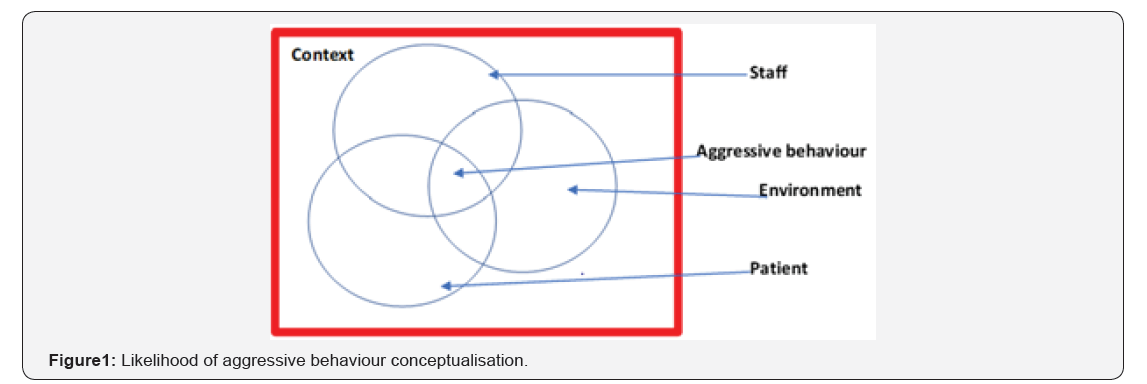
These factors are heterarchical in that no one factor is more important than another and all elements are unranked. Any one of the factors can become the key cause of the aggressive behaviour depending on the circumstances. This conceptualisation assumes that the more there is a negative interaction between the staff, patient and environment factors within a given context the more likely is aggressive behaviour to occur. The implication for management is therefore to take a more holistic systems approach to reduce this interaction focusing on patients, staff, environment and context rather than just one thing such as intoxication. Such a model allows policy makers to come up with robust and effective organisational policies to assess and manage the risk of aggression towards staff or property. The specific factors of the patient, staff, environment and context are outlined in Figure 2 below.
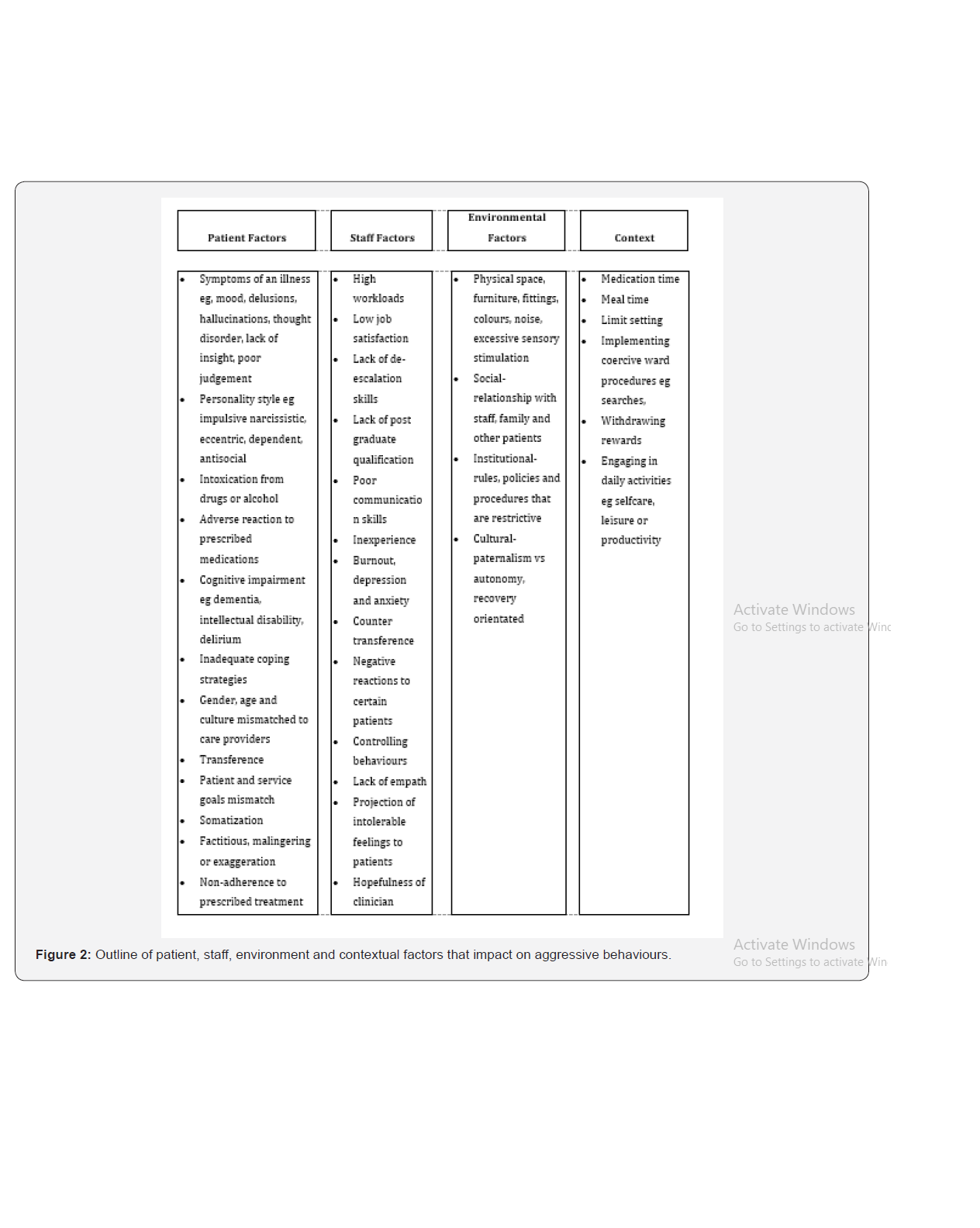
We argue that trying to manage each factor individually is unhelpful and the use of systems theory thinking is much more likely to yield positive results. We suggest a more holistic view to aggressive behaviour causes in healthcare settings as a way of enabling services to make sound policies on aggressive behaviours in health care going forward and avoid knee jerk reactions that might even make the situation worse for staff, patients and employers.
References
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, (5th edn.), American Psychiatric Publishing: Arlington, VA, USA.
- Center for Disease Control and Prevention (2014) Prevalence of autism spectrum disorder among children aged 8 years-autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report. Surveillance Summaries 63: 1-21.
- Post-Traumatic Stress Disorder (PTSD) (2018) National Institutes of Mental Health, United States.
- van Steensel FJA, van Bögels SM, Perrin S (2011) Anxiety disorders in children and adolescents with autistic spectrum disorders: A metaanalysis. Clin Child Fam Psychol Rev 14(3): 302–317.
- Mehtar M, Mukaddes NM (2011) Posttraumatic Stress Disorder in individuals with diagnosis of Autistic Spectrum Disorders. Res Autism Spectr Disord 5: 539-546.
- De Bruin EI, Ferdinand RF, Meester S, de Nij PFA, Verheij F (2007) High rates of psychiatric comorbidity in PDD-NOS. J Autism Dev Disord 37(5): 877-886.
- Storch EA, Sulkowski ML, Nadeau J, Lewin AB, Arnold EB, et al. (2013) The phenomenology and clinical correlates of suicidal thoughts and behaviors in youth with autism spectrum disorders. J Autism Develop Disord 43(10): 2450-2459.
- Dell’Osso L, Dalle Luche R, Carmassi C (2015) A new perspective in post-traumatic stress disorder: Which role for unrecognized autism spectrum. International Journal of Emergency Mental Health and Human Resilience 17(2): 436-438.
- Nietlisbach G, Maercker A (2009) Social cognition and interpersonal impairments in trauma survivors with PTSD. Journal of Aggression Maltreatment & Trauma 18(4): 382-402.
- Kerns CM, Newschaffer CJ, Berkowitz SJ (2015) Traumatic childhood events and autism spectrum disorder. J Autism Dev Disord 45(11): 3475-3486.
- Stavropoulos K, Bolourian Y, Blacher J (2018) Differential Diagnosis of Autism Spectrum Disorder and Post Traumatic Stress Disorder: Two Clinical Cases. J Clin Med 7(4).
- Trelles Thorne Mdel P, Khinda N, Coffey BJ (2015) Posttraumatic stress disorder in a child with autism spectrum disorder: Challenges in management. J Child Adolesc Psychopharmacol 25(6): 514-517.
- Morries LD, Cassano P, Henderson TA (2015) Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy. Neuropsychiatr Dis Treat 11: 2159-2175.
- Hamblin MR (2016) Shining light on the head: Photo biomodulation for brain disorders. BBA Clin 6: 113-124.






























