Metabolic Outcomes of Bariatric Surgery in Obesity Management: Indian Perspective
Vikas Ahluwalia*
Max Super Speciality Hospital, India
Submission: March 12, 2018; Published: August 24, 2018
*Corresponding author: Vikas Ahluwalia, Max Super Speciality Hospital, India.
How to cite this article: Vikas A. Metabolic Outcomes of Bariatric Surgery in Obesity Management: Indian Perspective. Curre Res Diabetes & Obes J. 2018; 8(4): 555744. DOI: 10.19080/CRDOJ.2018.08.555744.
Introduction
Obesity is defined as a medical disease in which excess body fat has accumulated to the extent that it may have a negative impact on health. Obesity has been a global burden in the society, destroying nations medically and economically. It is considered when the body mass index (BMI), is over 30kg/m2, with the range 25-30kg/m2 defined as overweight. India is one of the countries with the highest prevalence of obesity. The term obesity is a major part of metabolic syndrome, where parameters like abdominal girth, fasting sugars, blood pressure, serum triglycerides and high-density lipoproteins are playing the key markers. The most important causes leading to obesity are excessive food intake, sedentary life style and genetic causes. Others may be some endocrine disorders and medications Obesity is a major risk factor linked to diabetes, hypertension, dyslipidemia, cardiovascular disease, stroke, osteoarthritis, depression, cancer and early death.
There is a requirement for optimal integration with multidisciplinary approach i.e lifestyle modification + pharmacotherapy + bariatric surgery for current management of obesity. Changes in diet and exercising are the main treatments for obesity. Reducing the consumption of energy-dense foods and increasing the intake of dietary fiber should be incorporated in diet plans. Some medicines may be used, along with a suitable diet that reduce appetite or decrease fat absorption. If multiple attempts in diet control and exercise fail then surgery for obesity is considered either by a balloon dilatation, gastrectomy or bypass to reduce the area of absorption in the stomach and intestines. Bariatric surgery has gained popularity worldwide as a treatment for obesity. It is associated with long-term weight loss and improvement in obesity related conditions.
The term – Diabesity (diabetes + obesity) is a constellation that includes obesity, insulin resistance, metabolic syndrome and type 2 diabetes. Bariatric surgery has shown marked improvement in management of diabesity. Overweight and obesity have a significant economic impact on health systems and the medical costs resulting in a big burden to the country and worldwide.
Objectives of Study
Primary objective
-To assess resolution of Diabetes Mellitus after surgery.
-To assess the resolution Dyslipidemia after surgery
-To assess resolution of Hypertension after surgery.
Secondary objective
-To assess change in BMI.
-To assess change in Waist circumference.
Study Design & Methods
We conducted a retrospective study on 69 patients (males-27 and females-42) who underwent bariatric surgery (RYGB) in the Minimal Access Metabolic Surgery Institute, Max Hospital, Delhi, India. Enrollment was done after taking consent from the patients who were operated since 2012 and completed the 3 year follow up protocol till 2017 (Figure 1).
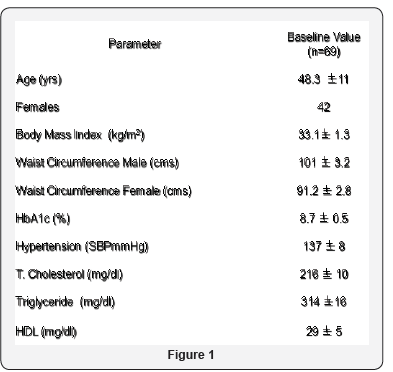
Baseline characteristics
The mean age was 48.3 years (range 40-62 years). The duration of the study was 2012 -2017.the selection criteria of these patients were BMI 30-35Kg/metre sq, HbA1c >8.0mg/dl and willingness to comply with the follow up protocol.
Data and statistical analysis
Continuous data are presented as means±standard deviation and changes in metabolic parameters were evaluated using SPSS software, version 12 and p- value <0.05 were considered significant.
Results
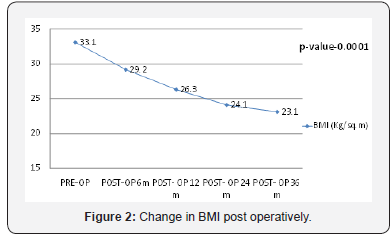
(Figure 2) shows a statistically significant decrease in the Body Mass Index of patients who underwent the surgery.
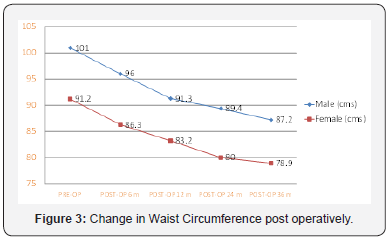
(Figure 3) shows the decrease in the waist circumference of the males and females. Some of them falling the below the cut off value for metabolic syndrome.

(Figure 4) shows the significant decrease in HbA1C values in patients undergoing the surgery, with 88.4 % patients undergoing remission.
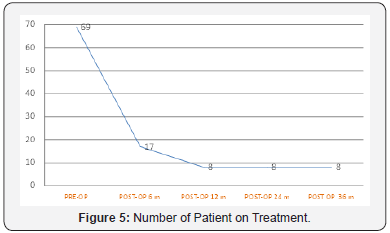
(Figure 5) shows that among the patients who underwent surgery, only 11 % were on the treatment, at the end of 3 years post operatively.
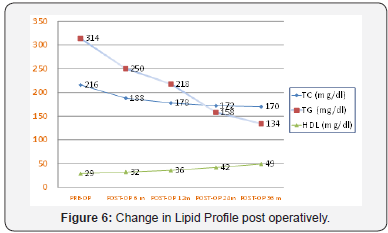
(Figure 6) shows the improvement in Lipid profile unto an extent that 74.6 % patients landed into remission after the surgery.

(Figure 7) shows the changes in blood pressure, systolic and diastolic) post operatively. 58 % had a normal blood pressure post-surgery.
Metabolic Outcomes
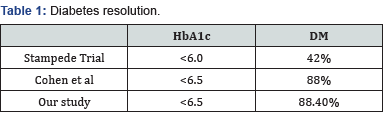
(Table 1) Our study is in accordance with the study conducted by Cohen et al where they had 88 % resolution in the prevalence of Diabetes, as compared to ours (88.4%).
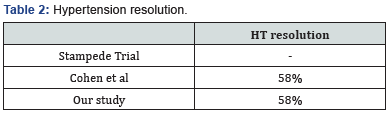
(Table 2) Our study results are like the one conducted by Cohen et al in terms of resolution of hypertension post-surgery (58% vs 58 %).
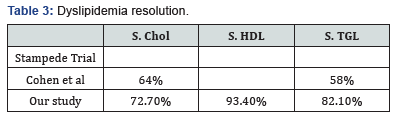
(Table 3) As compared to Cohen et al, our study shows a greater reduction in levels Serum Cholesterol (64 % vs 72.7 %) & Serum Triglycerides (58% vs 82.1 %).
Conclusion
The study concluded that bariatric surgery can be considered as a treatment option for poorly controlled diabetics with BMI 30 to 35kg/m2. The negative outcomes of obesity are greater than the risk of surgery as the treatment option.
References
- Abetz L, Sutton M, Brady L, (2002) The diabetic foot ulcer scale: a quality of life instrument for use in clinical trials. Pract Diab Int 19: 167-175.
- Brownrigg JR, Davey J, Holt PJ (2012) The association of ulceration of the foot with cardiovascular and all-cause mortality in patients with diabe- tes: a meta-analysis. Diabetologia 55(11): 2906-2912.
- Brem H, Balledux J, Bloom T, Kerstein MD, Hollier L (2000) Healing of diabetic foot ulcers and pressure ulcers with human skin equivalent: a new paradigm in wound healing. Arch Surg 135(6): 627-634.
- Bennett SP, Griffiths GD, Schor AM, Leese GP, Schor SL (2003) Growth factors in the treatment of diabetic foot ulcers. Br J Surg 90(2): 133- 146.
- Diabetes UK (2011) Putting feet first: national minimum skills framework. Joint initiative from the Diabetes UK, Foot in Diabetes UK, NHS Diabetes, the Association of British Clinical Diabetologists, the Primary Care Diabetes Society, the Society of Chiropodists and Podiatrists. Diabetes, London, UK.
- Guzman-Gardearzabal E, Leyva-Bohorquez G, Salas-Colín S, Paz- Janeiro JL, Alvarado-Ruiz R, et al. (2000) Treatment of chronic ulcers in the lower extremities with topical becaplermin gel .01%: a multicenter open-label study. Adv Ther 17(4): 184-189
- Singh N, Armstrong DA, Lipsky BA (2005) Preventing foot ulcers in patients with diabetes. JAMA 293(2): 217-228.
- Bakker K, Apelqvist J, Schaper NC (2012) on behalf of the International Work-ing Group on the Diabetic Foot Editorial Board. Practical guidelines on the management and prevention of the diabetic foot 2011. Diabetes Metab Res Rev 28(Suppl 1): 225-231.
- Ramsay SD, Newton K, Blough D (1999) Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care 22(3): 382-387.
- Rathur HM, Boulton AJM (2007) The diabetic foot. Clin Dermatol 25: 109-120.
- Young MJ, McCardle JE, Randall LE (2008) Improved survival of diabetic foot ulcer patients 1995-2008: possible impact of aggressive cardiovascular risk management. Diabetes Care 31(11): 2143-2147.
- Hinchcliffe RJ, Andros G, Apelqvist J (2012) A systematic review of the effectiveness of revascularisation of the ulcerated foot in patients with diabetes and peripheral arterial disease. Diabetes Metab Res Rev 28(Suppl 1): 179-217.
- Muller IS, Bartelink ML, Wim JC (2002) Foot ulceration and lower limb amputation in type 2 diabetic patients in Dutch Primary Health Care. Diabetes Care 25(3): 570-574.
- Dutta P, Bhansali A, Mittal BR, Singh B, Masoodi SR (2006) Instant 99mTc-ciprofloxacin scintigraphy for the diagnosis of osteomyelitis in the diabetic foot. Foot Ankle Int 27(9): 716-722.
- National Institute for Health and Clinical Excellence (2011) Diabetic foot problems: inpatient management of diabetic foot problems. Clinical guide- line 119. NICE, London, UK.
- Veves A, Falanga V, Armstrong DG, Sabolinski ML (2001) Graftskin, a human skin equivalent, is effective in the management of noninfected neuropathic diabetic foot ulcers: a prospective randomized multicenter clinical trial. Diabetes Care 24(2): 290-295.






























