Review on General Effective & Therapeutic Diabetic Wound Management
Blessing Nimasajai XS*
University of Bisha, Saudi Arabia
Submission: February 05, 2018; Published: August 24, 2018
*Corresponding author: Blessing Nimasajai XS, Lecturer in Nursing, Applied Medical Science College For Females, Alnamas, University Of Bisha, Saudi Arabia.
How to cite this article: Blessing Nimasajai XS. Review on General Effective & Therapeutic Diabetic Wound Management. Curre Res Diabetes & Obes J. 2018; 8(4): 555743. DOI: 10.19080/CRDOJ.2018.08.555743.
Abstract
Diabetes mellitus is a syndrome of disordered metabolism with abnormally high blood glucose levels (hyperglycemia) (Tierney 2002). According to the latest 2016 data from the World Health Organization (WHO) it is estimated that globally 422 million adults are living with diabetes mellitus .The different types of diabetes are type 1 diabetes (diminished production of insulin) “insulin-dependent diabetes mellitus” ( IDDM) or “juvenile diabetes” , type 2 diabetes (impaired response to insulin and β-cell dysfunction) “non-insulin-dependent diabetes mellitus” (NIDDM) or “adult-onset diabetes” and the other is gestational diabetes which occurs during pregnancy. All type shows signs and symptoms like hyperglycemia, excessive urine production, compensatory thirst, increased fluid intake, blurred vision, unexplained weight loss, lethargy, and changes in energy metabolism. Uncontrolled diabetes mellitus may cause many complications, one of the most serious complication is diabetic wound. This article is based on various research reviews and it was written because most of the people were suffering with diabetic wound and finally they are going for amputation, which is really a painful event and according to me all body parts is very much important for all human being and as early as from the creation of human being by God , the human body is created with all necessary parts & it is our duty & responsibility in caring & protecting the humans body parts as much as possible from amputation. Drop of insulin in blood leads to diabetes mellitus and its complication leads to diabetic ulcer and finally some diabetic ulcers lead to the loss of body parts. To prevent from amputation on behalf of diabetic ulcer, all health care professionals should give more concentration in therapeutic diabetic wound management.
Keywords: Diabetes mellitus; Insulin; Hyperglycemia; Diabetic ulcer; Amputation; Complication
Introduction
“Wounds don’t heal the way you want them to, they heal the way they need to. It takes time for wounds to fade into scars. It takes time for the process of healing to take place. Give yourself that time. Give yourself that grace. Be gentle with your wounds. Be gentle with your heart. You deserve to heal.” - Dele Olanubi
Diabetes mellitus is a group of metabolic disorder characterized by hyperglycemia resulting from deficiency in insulin secretion and its imbalance. The increased blood sugar level in diabetes mellitus is associated with long-term damage, dysfunction, and failure of various organs such the eyes, kidneys, nerves, heart, and blood vessels. As per 2016 data from the World Health Organization (WHO) shows the estimation of 422 million adults are living with diabetes mellitus worldwide. Diabetes prevalence has been rising more rapidly in middle- and low-income countries [1]. The major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation is diabetes mellitus. WHO projects that by 2030, diabetes will be the seventh leading cause of death worldwide. The different types of diabetes are type 1 diabetes (diminished production of insulin) “insulin-dependent diabetes mellitus” (IDDM) or “juvenile diabetes”, type 2 diabetes (impaired response to insulin and β-cell dysfunction) “ non-insulin-dependent diabetes mellitus” (NIDDM) or “adult-onset diabetes” and the other is gestational diabetes which occurs during pregnancy. All type shows signs and symptoms like increase blood sugar level, excessive urine production, increased thirst, increased fluid intake, blurred vision, unexplained weight loss, lethargy, and changes in energy metabolism. Diabetic ulcers are growing more rapidly due mainly to increased incidence of both Type I and maturity-onset diabetes in the developed (high-GDP) countries around the world [2]. The prevalence of diabetic ulcers is rising at 9% annually. At present, this pool of patients is growing faster than the new technologies are reducing the incidence of wounds by healing them uncontrolled diabetes mellitus may cause many complications, one of the most serious complication is diabetic wound. This article is based on various research reviews and it was written because most of the people were suffering with diabetic wound and finally they are going for amputation, which is really a painful event and according to me all body parts is very much important for all human being and as early as from the creation of human being by God, the human body is created with all necessary parts & it is our duty & responsibility in caring & protecting the humans body parts as much as possible from amputation [3]. Drop of insulin in blood leads to diabetes mellitus and its complication leads to diabetic ulcer and finally some diabetic ulcers lead to the loss of body parts. To prevent from amputation on behalf of diabetic ulcer, all health care professionals should give more concentration in therapeutic diabetic wound management. Diabetic wound is a major health problem and its management involves a multidisciplinary approach (Figure 1). This review aims to provide an information regarding the current management strategies of diabetic wound, from prevention to the options for treatment. The authors believe that it may be useful to primary healthcare providers who were involved in the prevention or management of diabetic wound.
Definition/Terminology
Diabetes mellitus is defined as a chronic disease caused by imbalance between insulin by the pancreas and its demand. It leads to increased concentrations of glucose in the blood, which in turn damage many of the body’s systems, the blood vessels and nerves [4].
Diabetic wound is a wound which occur because of various factors, such as mechanical changes in conformation of the bony architecture of the foot, peripheral neuropathy, and atherosclerotic peripheral arterial disease, all of which occur with higher frequency and intensity in the diabetic population.
Diabetic wound risk factors
Risk factors includes poorly fitted or poor-quality shoes, poor hygiene (not washing regularly or thoroughly), improper trimming of toenails, alcohol consumption, eye disease from diabetes, heart disease, kidney disease, obesity, tobacco use (inhibits blood circulation) etc.
Cause of diabetic wound:
1. Increase Blood Sugar Levels: Diabetes is a metabolic disease that causes elevated levels of glucose in the blood. Elevated blood glucose levels stiffen the body’s arteries and narrow its blood vessels, restricting the delivery of the blood and oxygen needed to support the body’s natural healing abilities.
2. Decrease or Poor Circulation: Individuals with diabetes are at an increased risk for peripheral arterial disease (PAD), a condition that restricts blood flow to the feet and legs. PAD is especially problematic for those with chronic wounds, particularly diabetic foot ulcers, because it can seriously inhibit the body’s ability to heal. If left untreated, PAD can lead to amputation of the affected limb.
3. Peripheral Neuropathy /Nerve Damage: A lack of circulation in the extremities can result in a reduced supply of oxygen and nutrients to the body tissue and nerves, which is necessary for healing. Over time, nerves in these areas may become damaged, decreasing the sensation of pain, temperature and touch, making patients vulnerable to injury.
4. Immune System Issues: One of the roles the body’s immune system is to clear away dead, damaged tissue and build new skin cells once a wound or injury has occurred. Diabetes can slow a person’s immune system, which affects the body’s ability to send white blood cells to fight bacteria in an infected diabetic foot ulcer.
5. Infection: Because diabetics tend to have weaker immune systems, their bodies are more susceptible to infection. Particularly in those with diabetes, it’s common for a wound to develop an infection like non-healing diabetic foot ulcers.
Types /classification of diabetic wound
There are two most common diabetic wounds. They are external origin diabetic wounds and internal origin diabetic wounds. Due to peripheral neuropathy, wounds of external origin, such as skin cuts, burns, bumps and bruises, may often go unnoticed by the diabetic patient [5]. If external wounds go unnoticed for some time, delayed treatment can put the patient at risk for further complications. Wounds of internal origin, such as skin ulcers, ingrown toenails or calluses, can lead to the breakdown of skin and surrounding tissue, increasing the risk of bacterial infections.
Signs & symptoms of diabetic wound
Common signs and symptoms of diabetic wound are chronic pain or completely painless, signs of inflammation (swelling, redness, heat, pain and loss of function), signs of infection (pus drainage, discharge, bad odor and dead tissue), numbness and dullness (signs of nerve damage), fever and/or chills (signs of progressively worsening infection that can be limb-threatening or even life-threatening).
Diagnostic evaluations for diabetic wound
Diagnostic evaluations for diabetic wound include history collection, physical examination, examination of the ulcer, testing for loss of sensation, testing for vascular status, laboratory investigations (blood tests), pulse-volume recording, ultrasonography, ankle-brachial index, radiography, computed tomography, magnetic resonance imaging, bone scans, and angiography [6].
Factors that delay diabetic wound healing
Local factors are continued pressure over the site, desiccation and dehydration, trauma, edema, infection or heavy colonization, necrosis, maceration caused by incontinence, lack of oxygen delivery to the tissues, etc., [7]. Systemic factors are old age, obesity, chronic diseases, malnutrition, vascular insufficiency, immunodeficiency, smoking, stress, etc., (Table 1 & 2).


Management of diabetic wound
A. The essential components of diabetic wound management are:
B. Treating underlying disease processes
C. Ensuring adequate blood supply
D. Local wound care, including infection control
E. Antibiotic for infected diabetic wounds
F. Tissue debridement
G. Inflammation and infection control
H. Moisture balance (optimal dressing selection)
I. Epithelial edge advancement.
J. Pressure offloading.
a. Avoid bandaging over toes as this may cause a tourniquet effect (instead, layer gauze over the toes and secure with a band- age from the metatarsal heads to a suitable point on foot)
b. Use appropriate techniques (e.g. avoiding creases and being too bulky) and take care when dressing weightbearing areas
c. Avoid strong adhesive tapes on fragile skin
d. Avoid tight bandaging at the fifth toe and the fifth metatarsal head (trim the bandage back)
e. Ensure wound dead space is eliminated (e.g. use a dressing that conforms to the contours of the wound bed)
f. Remember that footwear needs to accommodate any dressing.
g. Vacuum-assisted closure: Vacuum-assisted closure (VAC) is a new method in wound care which speeds wound healing by causing vacuum, improving tissue perfusion and suctioning the exudates.
h. Hydrotherapy: The process of providing an adequate amount of liquid to bodily tissues
i. Treatment of charcot foot: Charcot neuropathic osteoarthropathy (CN), commonly referred to as the Charcot foot, the diabetic Charcot foot syndrome is a serious and potentially limb-threatening lower-extremity complication of diabetes. The diabetic Charcot foot is an inflammatory syndrome characterized by varying degrees of bone and joint disorganization secondary to underlying neuropathy, trauma, and perturbations of bone metabolism. Management includes Offloading at the acute active stage of the Charcot foot is the most important management strategy and could arrest the progression to deformity, antiresorptive drugs, Surgical treatment of Charcot arthropathy of the foot and ankle is based primarily on expert opinion [8]. Surgery has generally been advised for resecting infected bone (osteomyelitis), removing bony prominences that could not be accommodated with therapeutic footwear or custom orthoses, or correcting deformities that could not be successfully accommodated with therapeutic footwear, custom ankle-foot orthoses, or a Charcot Restraint Orthotic Walker.
j. Surgical Care, surgical wound closure & bone resection: Diabetics have higher risks of wound healing complications following surgery. Surgical wounds can easily become chronic wounds, such as pressure ulcers, without the right care. There are several types of wound dressings available, including the following:
a) Alginates: Alginate dressings encourage debridement and absorb wound drainage.
b) Collagens: These work well for surgical wounds in diabetics by encouraging blood vessel and new tissue growth.
c) Foams: Foam dressings have a high absorption rate, provide thermal insulation, and create moist healing environments.
d) Silvers: Silver-based dressings draw in bacteria and neutralize them, making them an excellent choice for preventing wound infections.
Armstrong et.al proposed a classification model for surgical management of the diabetic foot based on fundamental variables present in the assessment of risk and indication like presence of neuropathy (loss of protective sensation), presence or absence of an open wound & presence or absence of any acute limbthreatening infection [9]. According to the classes of diabetic foot surgery, class III (curative) and class IV (emergency) procedures involve a current diabetic foot ulcer or open wound. Emergency procedures are those performed to limit the spread of acute, limb-threatening infections. This class of surgery may be performed in the presence of limb ischemia to prevent further spread of the infection. The potential for vascular intervention should be considered either concomitant with this procedure, or in the immediate postoperative hospitalization period. he goals of the curative procedure is to speed up the healing of the diabetic foot wound and prevent recurrence of this wound. Surgical decision making is heavily dependent on the type of wound and its location. It is our experience that most chronic ulcerations present in the diabetic foot are a direct result of increased plantar pressure in the presence of peripheral neuropathy. The surgical goal for these types of ulcers is to relieve the source of increase in pressure. Some of the most time-honored procedures involve some sort of bone resection. This type of procedure aids in eliminating pressure underlying the wound. In the forefoot, bone resection has been well documented as able to heal a wound faster, prevent ulcer reoccurrence, and lower the incidence of infection compared with conservative treatment [10-13]. This may include isolated metatarsal head resection [14-16], pan metatarsal head resection, transmetatarsal amputation (TMA), exostectomy, and partial calcanectomy.
a. Revisional surgery for is frequently needed to control diabetic foot infections and for bony architecture may be required to remove pressure points. Such intervention includes resection of metatarsal heads or ostectomy.
b. Vascular reconstruction: Vascular surgeons, radiologists and plastic surgeons should form an integral part of the diabetic foot team. Here the potential limitation of investigation or reliance on symptoms in the diabetic patient are discussed. The acute presentation of the patient with a diabetic foot may necessitate emergency drainage or abscess formation and debridement of infected necrotic tissue, if necessary, prior to formal investigation and reconstruction. Detailed investigation should include intra-arterial digital subtraction angiography, with or without color flow duplex. These investigations will help to delineate the most beneficial interventional management. This may include a combination of interventional radiological techniques, proximal and distal vascular reconstruction, and indeed the combination of femorocrural, popliteal-crural reconstruction with plastic surgical techniques. Distal reconstruction in combination with split skin grafts and/or free flap closure may also help to preserve the limb in diabetic patients with severe necrosis and infection which requires extensive debridement.
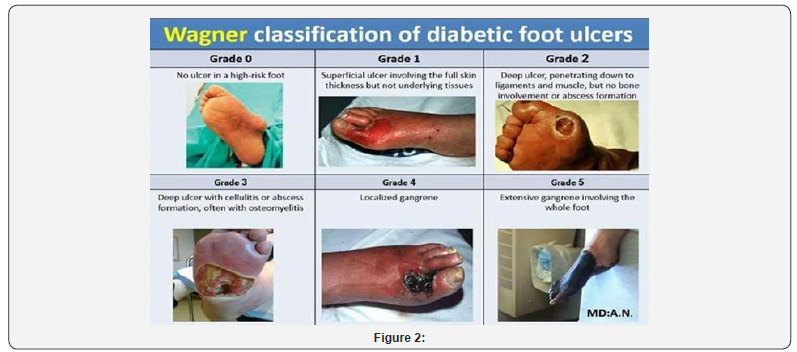
c. Skin grafts, Tissue-cultured skin substitutes, Xenograft: Advanced therapies for foot wounds are saving limbs, restoring mobility, and improving the lives of many people with diabetes who suffer from non-healing foot ulcers (Figure 2). Skin substitutes can consist of bioengineered or artificial skin, autografts (taken from the patient), allografts (taken from another person) or xenografts (taken from animals). According to Dieckmann et al. skin substitutes can be divided into two broad categories: biomaterial and cellular. Biomaterial skin substitutes do not contain cells (acellular) and are derived from natural or synthetic sources. Natural sources include human cadaveric skin processed to remove the cellular components and retain the structural proteins of the dermis and collagen matrix obtained from bovine and porcine sources. Synthetic sources include degradable polymers such as polylactide and polyglycolide. Whether natural or synthetic, the biomaterial provides an extracellular matrix that allows for infiltration of surrounding cells. Cellular skin substitutes are distinguished by their origin: xenogeneic (from nonhuman species), autologous (from the patient), and allogenic (from another human). Keratinocytes and fibroblasts obtained from these sources are cultured in vitro to produce the cellular material used to make the substitute. However, the classification of skin substitutes into either biomaterial or cellular is not completely accurate since the two are combined into several wound care products. Human tissue can be obtained from human donors, processed, and used exactly in the same role in the recipient-skin for skin, tendon for tendon, bone for bone. These uses are regulated as human tissue intended for transplantation, if the proposed clinical use and manufacturing methods are consistent with definitions of “Homologous Use” and “Minimal Manipulation”. Human tissue and cells may also be used as a source of cells for culturing to produce cellular-derived material for wound healing.
d. Hyperbaric Oxygen Treatment: Hyperbaric Oxygen Therapy is a treatment option for diabetic patients with a foot ulcer, where the patient inhales 100% oxygen in a pressurized chamber. This method helps the body increase the oxygen levels in the blood. It also exposes the affected tissues to more oxygen than would otherwise be present, thus allowing for enhanced healing. Hyperbaric oxygen therapy (HBOT) has been promoted as an effective treatment for diabetic foot wounds, it improves wound tissue hypoxia, enhancing perfusion, reducing edema, down regulating inflammatory cytokines, promoting fibroblast proliferation, collagen production, and angiogenesis make it a useful adjunct in clinical practice for “problem wounds,” such as diabetic foot ulcers. Hyperbaric oxygen therapy increases the saturation of oxygen in the blood, due to the enhancement of atmospheric pressure. Increased oxygen can promote white blood cell activity, encourage tissue development and induce capillary growth. This method can be beneficial for a variety of conditions but is proving exceptionally promising in the treatment of diabetic foot ulcers.
e. Dietary Managements: Nutrient deficiencies have influence of wound healing in a different way. Malnutrition and/ or nutrient deficiencies can impair collagen synthesis, prolong inflammation, decrease phagocytosis (causing dysfunction of B and T cells), and decrease the mechanical strength of the skin. High-protein, high-calorie, nutrient-enriched supplements may be recommended between meals if food intake doesn’t meet a patient’s needs for wound healing. Arginine and glutamine are two amino acids that have been studied extensively for their role in wound healing. In addition, beta-hydroxy-methyl buterate, which is a metabolite of the amino acid leucine, has been linked with improved wound healing and tissue regrowth. People with diabetes do not heal as efficiently as people with normal blood sugar levels. Certain foods can also help keep your blood sugar optimal.
f. blood sugar levels: Certain foods can also help keep your blood sugar optimal.
Protein helps to repair tissue
a. Fish
b. Shellfish
c. Eggs (egg whites have protein and no cholesterol)
d. Cheese (low fat is better for your heart)
e. Poultry
f. Lean meat
g. Nut butters (peanut butter, almond butter, cashew butter, etc.)
Carbohydrates give you energy
a. Starch (bread-whole grains are best-cereal, noodles, rice, barley, kasha)
b. Starchy vegetables (sweet or white potatoes, corn, peas, beans)
c. Non-starchy vegetables (broccoli, green beans, asparagus, salad greens)
d. Fruit
e. Milk (drinking milk, soymilk or yogurt)
Fat allows you to absorb your fat-soluble vitamins-A, D, E, K
a. Oil (olive and canola oil are best for your heart)
b. Nuts (are good for your heart and health)
c. Avocado (is good for your heart)
d. Margarine (pick one without trans-fat)
e. Butter (use more sparingly)
The following vitamins are excellent to heal wounds most efficiently
A. Vitamin C-foods with high levels:
a. Peppers (especially red)
b. Kiwi fruit, Tomatoes
c. Citrus fruits (oranges, grapefruits)
d. Broccoli
B. Vitamin A-foods with high levels:
a. Orange colored fruits/vegetables
b. Dark green leafy vegetables
C. Vitamin E-foods with high levels:
a. Whole grainsa. Whole grains
b. Wheat germ
c. Dark leafy green vegetables
d. Eggs**
e. Nuts and seeds
D. Vitamin B-foods with high levels:
a. Whole grains (wheat and oats)
b. Fish and seafood
c. Poultry and meat
d. Eggs**
E. Zinc-foods with high levels:
a. Oysters (very high)
b. Beans
** Egg yolks contain vitamins and cholesterol while egg whites contain protein
A. Restriction of Activity: Many evidence-based cases studies show that increase activity delays in wound healing process, so therefore it is important to minimize the activities to the affected extremities
B. Amputation may be indicated in circumstances during Ischemic rest pain that cannot be managed by analgesia or revascularization, a life-threatening foot infection that cannot be managed by other measures, a non-healing ulcer that is accompanied by a higher burden of disease than would result from amputation. In some cases, for example, complications in a diabetic foot render it functionally useless and a well performed amputation is a better alternative for the patient.
C. Ultra-MIST Therapy, non-contact, low frequency, nonthermal ultrasound has a pain-free delivery through a fluid/ saline mist that acts as the medium to deliver energy to the diabetic wound and induce fast healing.
Steps to Avoid Amputation: Implementing A Global Wound Care Plan
Diagnosis of diabetes (+/_ peripheral sensory neuropathy)
AIM: Prevent the development of a diabetic wound
a. Implement diabetic wound prevention care plan that includes treatment of co-morbidities, good glycemic control and pressure offloading
b. Annually perform general foot examination:
c. Use 10g monofilament to assess sensory status
d. Inspection of the feet for deformities
e. Inspection of footwear for wear and tear and foreign objects that may traumatize foot
f. Maintain skin hydration (consider emollient therapy) for skin health
g. Offer patient education on checking feet for trauma
h. Ensure regular review and provide patient education
Development of diabetic wound
AIM: Treat the ulcer and prevent infection
a. Determine cause of ulcer
b. Agree treatment aims with patient and implement wound care plan:
c. Debride and regularly cleanse the wound
d. Take appropriate tissue samples for culture if infection is suspected
e. Select dressings to maintain moist wound environment and manage exudate effectively
f. Initiate antibiotic treatment if infection suspected and consider topical antimicrobial therapy if increased bio burden is suspected
g. Review offloading device and ensure footwear accommodates dressing
h. Optimize glycemic control for diabetes management
i. Refer for vascular assessment if clinically significant limb ischemia is suspected
j. Offer patient education on how to self-manage and when to raise concerns
Development of vascular disease
AIM: Prevent complications associated with ischemia
a. Ensure early referral to vascular specialist for arterial reconstruction to improve blood flow in patients with an ischemic or neuro ischemic ulcer
b. Optimize diabetes control
Ulcer becomes infected
AIM: Prevent life- or limb-threatening complications
a. For superficial (mild) infections-treat with systemic antibiotics and consider topical antimicrobials in selected cases
b. For deep (moderate or severe) infections-treat with appropriately selected empiric systemic antibiotics, modified by the results of culture and sensitivity reports
c. Offload pressure correctly and optimize glycemic control for diabetes management
d. Consider therapy directed at biofilm in wounds that are slow to heal
Active management of the ulcer and co-morbidities should aim to prevent amputation
a. Where amputation is not avoidable:
b. Implement skin and wound care plan to manage surgical wound and optimize healing
c. Review regularly and implement prevention care plan to reduce risk of recurrence or further diabetic wound on contralateral limb
Prevention of diabetic wound
a. Inspect feet daily: The CDC recommends people with diabetes inspect their feet every day for cuts, blisters, calluses, red spots, swelling and other abnormalities. Regularly trim toenails straight across to avoid ingrown toenails. If cannot see or reach the feet, use a mirror or ask for the assistance of a doctor, family member or caregiver. In addition to daily examination, have the doctor or podiatrist check your feet at least once per year.
b. Protect the feet from infection: Washing the feet each day is an important part of the diabetic foot care routine. Wash feet in lukewarm water (not hot water, which can scald and blister feet), and dry feet thoroughly afterward. Once dry, rub moisturizing lotion or cream on the tops and bottoms of feet. Do not apply lotion between toes, as this could foster bacterial growth. Don’t forget to put on socks and shoes, even if you are just staying in your home, to avoid stepping on something sharp and becoming injured.
c. Manage/ control diabetes mellitus: Keeping the blood sugar, blood pressure and cholesterol levels in check can prevent most of the complications related to diabetes, including nonhealing diabetic foot ulcers. Work with primary care physician to develop a diabetes self-management plan that may include healthy diet, regular exercise, blood sugar monitoring, smoking cessation and adherence to medication as directed.
Summary
A diabetic wound is an open sore or wound that occurs in approximately 15 percent of patients with diabetes and is commonly located on the bottom of the foot. This article review gives a brief knowledge regarding diabetes it’s signs and symptoms, how to manage diabetic wound and other complication. Physical examination of the extremity having a diabetic ulcer can be useful in the management of diabetic wound. The staging of diabetic foot wounds is based on the depth of soft tissue and osseous involvement. A complete blood cell count should be done, along with assessment of serum glucose and creatinine levels. The management of diabetic wound requires offloading the wound by using appropriate therapeutic footwear, daily saline or similar dressings to provide a moist wound environment, debridement when necessary, antibiotic therapy if osteomyelitis or cellulitis is present, optimal control of blood glucose, and evaluation and correction of peripheral arterial insufficiency. As a human being we all have the responsibility to protect our body parts from such chronic diseases.
Conclusion
As per various evidence-based reviews clearly states that 84% of lower limb amputations have a history of diabetic wound. Diabetic wound and amputations significantly reduce the quality of life. Also, while checking on hospital admission, most of patients got admitted with diabetes. Therefore, it’s a very much important in caring diabetic patients with effective diabetic wound care for improving their quality of life.
References
- Abetz L, Sutton M, Brady L, (2002) The diabetic foot ulcer scale: a quality of life instrument for use in clinical trials. Pract Diab Int 19: 167-175.
- Brownrigg JR, Davey J, Holt PJ (2012) The association of ulceration of the foot with cardiovascular and all-cause mortality in patients with diabe- tes: a meta-analysis. Diabetologia 55(11): 2906-2912.
- Brem H, Balledux J, Bloom T, Kerstein MD, Hollier L (2000) Healing of diabetic foot ulcers and pressure ulcers with human skin equivalent: a new paradigm in wound healing. Arch Surg 135(6): 627-634.
- Bennett SP, Griffiths GD, Schor AM, Leese GP, Schor SL (2003) Growth factors in the treatment of diabetic foot ulcers. Br J Surg 90(2): 133- 146.
- Diabetes UK (2011) Putting feet first: national minimum skills framework. Joint initiative from the Diabetes UK, Foot in Diabetes UK, NHS Diabetes, the Association of British Clinical Diabetologists, the Primary Care Diabetes Society, the Society of Chiropodists and Podiatrists. Diabetes, London, UK.
- Guzman-Gardearzabal E, Leyva-Bohorquez G, Salas-Colín S, Paz- Janeiro JL, Alvarado-Ruiz R, et al. (2000) Treatment of chronic ulcers in the lower extremities with topical becaplermin gel .01%: a multicenter open-label study. Adv Ther 17(4): 184-189
- Singh N, Armstrong DA, Lipsky BA (2005) Preventing foot ulcers in patients with diabetes. JAMA 293(2): 217-228.
- Bakker K, Apelqvist J, Schaper NC (2012) on behalf of the International Work-ing Group on the Diabetic Foot Editorial Board. Practical guidelines on the management and prevention of the diabetic foot 2011. Diabetes Metab Res Rev 28(Suppl 1): 225-231.
- Ramsay SD, Newton K, Blough D (1999) Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care 22(3): 382-387
- Rathur HM, Boulton AJM (2007) The diabetic foot. Clin Dermatol 25: 109-120.
- Young MJ, McCardle JE, Randall LE (2008) Improved survival of diabetic foot ulcer patients 1995-2008: possible impact of aggressive cardiovascular risk management. Diabetes Care 31(11): 2143-2147.
- Hinchcliffe RJ, Andros G, Apelqvist J (2012) A systematic review of the effectiveness of revascularisation of the ulcerated foot in patients with diabetes and peripheral arterial disease. Diabetes Metab Res Rev 28(Suppl 1): 179-217
- Muller IS, Bartelink ML, Wim JC (2002) Foot ulceration and lower limb amputation in type 2 diabetic patients in Dutch Primary Health Care. Diabetes Care 25(3): 570-574.
- Dutta P, Bhansali A, Mittal BR, Singh B, Masoodi SR (2006) Instant 99mTc-ciprofloxacin scintigraphy for the diagnosis of osteomyelitis in the diabetic foot. Foot Ankle Int 27(9): 716-722.
- National Institute for Health and Clinical Excellence (2011) Diabetic foot problems: inpatient management of diabetic foot problems. Clinical guide- line 119. NICE, London, UK.
- Veves A, Falanga V, Armstrong DG, Sabolinski ML (2001) Graftskin, a human skin equivalent, is effective in the management of noninfected neuropathic diabetic foot ulcers: a prospective randomized multicenter clinical trial. Diabetes Care 24(2): 290-295.






























