Fibrinolytic, Platelets and Endothelial Microparticles Abnormalities among Obese Type 2 Diabetic Patients
Mohammed H Saiem Al-Dahr*
Department of Medical Laboratory Technology, King Abdulaziz University, Saudi Arabia
Submission: February 07, 2017; Published: February 28, 2017
*Corresponding author: Mohammed H Saiem Al-Dahr, Department of Medical Laboratory Technology, Faculty of Applied Medical Sciences, King Abdulaziz University, PO Box 80324, Jeddah, 21589, Saudi Arabia, Email;drsiem@hotmail.com
How to cite this article: Mohammed H S A. Fibrinolytic, Platelets and Endothelial Microparticles Abnormalities among Obese Type 2 Diabetic Patients. Curre Res Diabetes & Obes J. 2017; 1(3): 555565. DOI: 10.19080/CRDOJ.2017.1.555565. DOI:10.19080/CRDOJ.2017.01.555565
Abstract
Background: The prevalence of cardiovascular disorders is progressively increased among type diabetic (T2DM) patients. While, the influence of association between obesity and T2DM on the level of platelets and endothelial microparticles remain to be fully elucidated.
Objective: The aim of this was to measure the abnormalities of Fibrinolytic parameters, fibrinogen, platelets and endothelial microparticles among obese T2DM patients.
Materials and Methods: Fifty non-smokers obese type 2 diabetic patients were included in this study. The mean age was47.13±5.42 year and mean body mass index was 33.34±4.11 kg/m2 refers as the first group (A). Initially, a physician at King Abdulaziz University Hospital examined all participants; their medical history was taken to collect information about general condition, physical activity and current medications if any. All subjects with any cardiovascular conditions (those with a known history of uncontrolled hypertension, congenital and rheumatic heart diseases), any pulmonary disease (obstructive or restrictive lung diseases), were excluded from the study. In the other hand another fifty non-diabetic subjects not suffering of any disease, were participated in the study as a control group refers as (B).
Results: FDetailed baseline characteristics of the patients with T2DM and healthy controls showed a significant difference for all characteristics of the diabetic patient’ svs controls, except in the age. However, the comparison between values of BMI, tPA: Ag, fibrinogen, PAI-1: Ac, PMP CD41+ and EMP CD144+ for group (A) and group (B), there were statistical significant differences. However, the relationship between tPA: Ag, fibrinogen, PAI-1: Ac, PMP CD41+, EMPCD144+ and BMI , both groups showed a strong direct relationship.
Conclusion: There was a positive association between obesity and the elevated biomarkers of endothelial, platelets microparticles and Fibrinolytic parameters abnormalities among type 2 diabetic patients.
Keywords: Obesity: Melanocortin type-4 receptor; MC4R; Pharmacological agent; Diet; Bariatric surgery; Weight loss
Keywords: Sleeve gastrectomy; Roux en Y gastric bypass leak; Fistula; Restrictive surgery
Introduction
The prevalence of both diabetes associated with obesity is on the rise [1]. The worldwide estimation of diabetics was 171 million in 2000, however this number will be projected to 366 million by 2030 [2] along with increase in mortality rate among patients with diabetes [3]. However, the economic impact of diabetes is great which 147 billion US dollars was in 2008 [4,5]. Cardiovascular complications are more common among obese individuals with type 2 diabetes (T2DM) [6] which is the main cause of higher mortality rate among obese T2DM [7]. Moreover, level of microparticles (MPs) can be considered as essential biomarkers of cardiovascular risk [8].
Endothelial microparticles are indicators for vascular tone, coagulation, endothelial inflammation and stress/damage of the endothelial cell [9]. However, platelet micro particles that released from activated platelets are indirect biomarker for endothelial dysfunction as it indicates increased inflammation and abnormal coagulation [10-17]. The aim of this was to measure the abnormalities of Fibrinolytic parameters,fibrinogen, platelets and endothelial microparticles among obese T2DM patients.
Materials and Methods
Subjects
Fifty non-smokers obese type 2 diabetic patients visiting King Abdulaziz University Hospital, Jeddah, Saudi Arabia, were included in this study. The mean age was 47.13±5.42 year and mean body mass index was 33.34±4.11 kg/m2 refers as the first group (A). Initially, a physician at King Abdulaziz University Hospital examined all participants; their medical history was taken to collect information about general condition, physical activity and current medications if any. All subjects with any cardiovascular conditions (those with a known history of uncontrolled hypertension, congenital and rheumatic heart diseases), any pulmonary disease (obstructive or restrictive lung diseases), were excluded from the study. In the other hand another fifty non-diabetic subjects not suffering of any disease, were participated in the study as a control group refers as (B). The Ethics Committee of the Faculty of Applied Medical Sciences, King Abdulaziz University, approved this study. All participants signed a written informed consent.
Evaluated parameters
Overnight fasting venous blood samples were taken from ante cubital vein puncture were used for the study of lipid profile analysis, while the other two tubes contained (EDTA) for complete blood count, HbA1c and sodium citrate for coagulation and microparticles studies using a fully automated analyzer machine(Dimenition RxL, Diagnostics) at king Abdulaziz University Hospital.
Centrifugation of the whole blood at 1500 xg for 10 min was done to have the platelet poor plasma which was then separated and stored at (-80°C) until analysis.
Analysis of coagulation and Fibrinolytic parameters
The PPP samples were processed with an enzyme linked immune absorbent assay (ELISA) kits for the determination of plasma tPA and PAI-1 activities and antigens and the measurement for activities was performed using Chromolize™ tPA and Spectrolyse® pL PAI Biopool, Umea, Sweden). However, fibrinogen level was measured using Zymutest Fibrinogen, ELISA, Hyphen Biomed, France.
Microparticles preparation and quantification
Flow cytometric analysis was used for the measurement of changes in platelets activities in type 2 diabetic patients.50 μ PPP was incubated with different monoclonal antibodies (5 μl CD41 FITC and 5μl CD144 PE) for 30 min at 4oC in a dark place. The measurement of these markers was performed by using four color FACSCalibur®cytometer.Prior to flow cytometric analysis 30μl of flow Trucount Beads (BD Biosciences),was added to microparticles quantization allowing the calculation of circulating endothelial and platelet derived microparticles (EMP) number / μl PPP [18,19].
Evaluation of anthropometric parameters
Measurements of weight and height for both participant groups were performed by using a digital stadiometer (JENIX DS 102, S. Korea), for the height and body weight were measured on a balance scale (HC4211, S. Korea) then, Body Mass Index (BMI) was computed as Body weight/Height2.
Statistical analysis
Independent “t” test was used to compare the investigated parameters between both groups (P<0.05). However, the degree of correlation body mass index and Fibrinolytic, endothelial and platelets microparticles was calculated with Pearson’s correlation coefficients (r).
Results

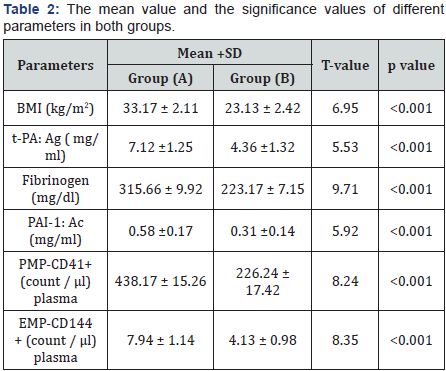
Detailed baseline characteristics of the patients with T2DM and healthy controls were presented in Table 1. There was a significant difference for all characteristics of the diabetic patient’s vs controls, except in the age (Table 1). Concerning the comparison between values of BMI, tPA: Ag, fibrinogen, PAI-1: Ac, PMP CD41+ and EMP CD144+ for group (A) and group (B), there were statistical significant differences as seen in (Table 2). The relationship between tPA: Ag, fibrinogen, PAI-1: Ac, PMP CD41+, EMPCD144+ and BMI, both groups showed a strong direct relationship (Table 3).

Discussion
The cardiovascular disorders are three times more frequent among diabetics and mortality rate may reach about 50–75% of diabetic population due to coronary artery disease [20,21]. MPs are biomarkers that can be of value in prediction of risk factors of cardiovascular disease, and as potential targets of therapy [22]. Therefore, this study was a trial to measure the coagulation parameters, platelet and endothelial MPs in T2DM patients compared to control subjects.
The principal findings of in this study included an increased BMI that were positively correlated with higher values of t-PA: Ag, PAI-1: Ac, EMP-CD144+ and PMPCD41+levels in obese T2DM patients. These findings agreed with many previous studies [23- 29]. The obtained results in this study, indicated that PMP-CD41+ were significantly increased among T2DM patients compared to the healthy control group which agreed with Tan et al. [30] who are the first to prove that the symptomatic atherosclerosis is usually associated with increased PMPs in T2DM patients. In addition, results in this study illustrated a significant increase in the circulating levels of EMP-144+ among T2DM compared to the healthy subjects. Moreover, Meigs et al. [31] found that CD62E+ (E selecting) EMPs are elevated among T2DM patients.
However, Tramontano et al. [32] and Helal et al. [33] stated that diabetic patients have relatively high level of CD31+ EMPs than non-diabetic subjects. Moreover, MP levels have been shown in multiple studies to be higher in diabetics than nondiabetics [30-32]. While, Koga et al. [30] conducted a study on 232 diabetics and 102 non-diabetics in Japan, endothelial MP levels were about twice as high among the diabetics. In addition, Jung et al. reported an association between endothelial MPs with macro vascular complications among diabetics [30].
Our study founded a positive association between BMI and EMP& PMP, which may be caused by the deleterious impact of visceral fat depot in over production of the MP as obesity induce a state of low systemic inflammatory state and causing chronic oxidative stress that, trigger release of MP [33,34].Finally, our results proved that levels of PAI-1 and t-PA were significantly increased among T2DM patients in comparison to healthy subjects.
Conclusion
There was a positive association between obesity and the elevated biomarkers of endothelial, platelets microparticles and Fibrinolytic parameters abnormalities among type 2 diabetic patients.
References
- Cheung B, Ong K, Cherny S, Sham P, Tso A, et al. (2009) Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. AmJ Med 122(5): 443-453.
- Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27(5): 1047-1053.
- seshasai S , Kaptoge S, Thompson A, Di Angelantonio E, Gao P, et al. (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl JMed 364(9): 829-841.
- Dall T, Zhang Y, Chen Y, Quick W, Yang W, et al. (2010) The economic burden of diabetes. Health Aff (Millwood) 29 (9): 297-303.
- Finkelstein E, Trogdon J, Cohen J, Dietz W, (2009) Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 28(5): w822-w831.
- Jonsson S, Hedblad B, Engström G, Nilsson P, Berglund G, et al. (2002) Influence of obesity on cardiovascular risk. Twenty three year followup of 22,025 men from an urban Swedish population. Int J Obes Rel at Metab Disord 26(8): 1046-1053.
- Gu K, Cowie C, Harris M (1998) Mortality in adults with and without diabetes in a national cohort of the U.S. population, 1971–1993. Diabetes Care 21(7): 1138-1145.
- Puddu P, Puddu G, Cravero E, Muscari S, Muscari A (2010) The involvement of circulating microparticles in inflammation, coagulation and cardiovascular diseases. Canadian Journal of Cardiology 26( 4): e140-e145.
- Leroyer A, Anfosso F, Lacroix R, Sabatier F, Simoncini S, et al. (2010) Endothelial derived microparticles: biological conveyors at the crossroad of inflammation, thrombosis and angiogenesis. Thromb Haemost 104(3): 456-463.
- Azevedo L, Pedro M, Laurindo F (2007) Circulating microparticles as therapeutic targets in cardio vascular diseases. Recent Pat Cardiovasc Drug Discov 2(1): 41-51.
- Shantsila E, Kamphuisen P, Lip G (2010)- Circulating microparticles in cardiovascular disease: implications for atherogenesis and atherothrombosis. J Thromb Haemost 8(11): 2358-2368.
- Boulanger C, Amabile N, Tedgui A (2006) Circulating microparticles: a potential prognostic marker for atherosclerotic vascular disease. Hypertension 48(20): 180-186.
- Nomura S, Suzuki M, Katsura K, Xie G, Miyazaki Y, et al. (1995) Platelet-derived microparticles may influence the development of atherosclerosis in diabetes mellitus. Atherosclerosis 116(2): 235-240.
- George J, Thoi L, McManus L, Reimann T (1982) Isolation of human platelet membrane microparticles from plasma and serum. Blood 60(4): 834-840.
- Sims P, Wiedmer T, Esmon C, Weiss H, Shattil S (1989) Assembly of the platelet prothrombinase complex is linked to vesiculation of the platelet plasma membrane. Studies in Scott syndrome: an isolated defect in platelet procoagulantactivity. J BiolChem 264(29): 17049- 17057.
- Ramacciotti E, Hawley A, Farris D (2009) Leukocyte- and plateletderived microparticles correlate with thrombus weight and tissue factor activity in an experimental mouse model of venous thrombosis. Thromb Haemost 101(4): 748-754.
- Anfossi G, Russo I, Trovati M (2009) Platelet dysfunction in central obesity. Nutrition Metabolism and Cardiovascular Diseases 19(6): 440-449.
- Jung C, Sorensson P, Saleh N, Arheden H,Ryen L, et al. (2012) Circulating endothelial and platelet-derived micro particles reflect the size of myocardium at risk in patients with ST-elevation myo cardialin farction. Atherosclerosis 221(1): 226-231.
- Jy W, Horstman LL, Jimenez JJ, Ahn YS, Biró E, et al. (2004) Measuring circulating cell-derived microparticles. J Thromb Haemost 2(10): 1842-1851.
- Helal O, Defoort C, Robert S, Marin C, Lesavre N, et al. (2011) Increased levels of microparticles originating from endothelial cells, platelets anderythrocytes in subjects with metabolic syndrome: Relationship with oxidative stress.Nutrition, Metabolism and Cardiovascular Diseases 21(9): 665-671.
- Howard BV, Rodriguez BL, Bennett PH, Harris MI, et al. (2002) Prevention Conference VI: Diabetes and Cardiovascular disease: Writing Group I: epidemiology. Circulation 105(18): e132-137.
- Saydah S, Eberhardt M, Loria C , Brancati F (2002) Age and the burden of death attributable to diabetes in the United States. Am J Epidemiol 156(80): 714-719.
- Viera A, Mooberry M, Key N (2012) Microparticles in cardiovascular disease patho physiology and outcomes. Journal of the American Society of Hypertension 6(4): 243-252.
- Eibl N, Krugluger W, Streit G, Schrattbauer K, Hopmeier P, et al. (2004) Improved metabolic control decreases platelet activation markers in patients with type-2 diabetes. Eur J Clin Invest 34(30): 205-209.
- Esposito K, Ciotola M, Giugliano D (2006) Pioglitazone reduces endothelialmicroparticles in the metabolic syndrome. Arterioscler Thromb Vasc Biol 26(8): 1926.
- Pirro M, Schillaci G, Paltriccia R, Bagaglia F, Menecali C, et al. (2006) Increased ratio of CD31+/CD42-microparticles to endothelial progenitors as a novel marker of atherosclerosis in hypercholesterolemia. Arterioscler Thromb VascBiol 26(11): 2530- 2535.
- Enjeti S, Lincz L, Seldon M (2007) Detection and measurement of microparticles. ThrombHemost 33(8): 771-779.
- Tan K, Tayebjee M, Lynd C, Blann A, Lip G (2005) Platelet microparticles and soluble P selectin in peripheral artery disease: relationship to extent of disease and platelet activation markers. Ann Med 37(1): 61- 66.
- Meigs JB, Hu FB, Rifai N, Manson JE (2004) Biomarkers of endothelial dysfunction and risk of type 2 diabetes mellitus. JAMA 291(16): 1978- 1986.
- Tramontano AF, Lyubarova R, Tsiakos J, Palaia T, Deleon JR, et al. (2010) Circulating endothelial microparticles in diabetes mellitus. Mediators Inflamm 2010: 250476.
- Koga H, Sugiyama S, Kugiyama K, Watanabe K, Fukushima H (2005) Elevated levels of VE cadherin-positive endothelial microparticles in patients with type 2 diabetes mellitus and coronary artery disease. J Am Coll Cardiol 45(10): 1622-1630.
- Nozaki T, Sugiyama S, Koga H, Sugamura K, Oh ba K, et al. (2009) Significance of a multiple biomarkers strategy including endothelial dysfunction to improve risk stratification for cardiovascular events in patients at high risk for coronary heart disease. J Am Coll Cardiol 11 54(7): 601-608.
- Jung KH, Chu K, Lee ST, Bahn JJ, Kim JH, et al. (2011) Risk of macrovascular complications in type 2 diabetes mellitus: endothelialmicroparticle profiles. Cerebrovasc Dis 31(50): 485-493.
- Keaney JF Jr, Larson MG, Vasan RS, Wilson PW, Lipinska I, et al. (2003) Obesity and systemic oxidative stress: clinical correlates of oxidative stress in the Framingham Study. Arterioscler Thromb Vasc Biol 23(3): 434-439.
- Juhan-Vague I, Pyke SD, Alessi MC, Jespersen J, Haverkate F, et al. (1996) Fibrinolytic factors and the risk of myocardial infarction or sudden death inpatients with angina pectoris. ECAT Study Group. European Concerted Action on Thrombosis and Disabilities. Circulation 94(9): 2057-2063.
- Held C, Hjemdahl P, Rehnqvist N, Wallén NH, Björkander I, et al. (1997) Fibrinolytic variables and cardiovascular prognosis in patients with stable angina pectoris treated with verapamil or metopro lol. Results from the Angina Prognosis study in Stockholm. Circulation 95(10): 2380-2386.
- Thögersen AM, Jansson JH, Boman K, Nilsson TK, Weinehall L, et al. (1998) High plasminogen activator inhibitor and tissue plasminogen activator levels in plasma precede a first acute myocardial infarction in both men and women: evidence for the fibrinolytic system as an independent primary risk factor. Circulation 98(21): 2241-2247.






























