Beta Thalassemia: an Indian Perspective
Pranab Roy*
Department of Molecular Biology Unit, Institute of Child Health, India
Submission: September 11, 2019; Published: September 19, 2019
*Corresponding author: Pranab Roy, Department of Molecular Biology Unit, Institute of Child Health, Kolkata -700017, India
How to cite this article: Pranab Roy. Beta Thalassemia: an Indian Perspective. Adv Biotechnol Microbiol. 2019; 14(4): 555893. DOI: 10.19080/AIBM.2019.14.555892
Mini Review
Beta-thalassemia’s are a group of hereditary blood disorders which are characterized by anomalous synthesis of the beta chains of hemoglobin. They result in variable phenotypes ranging from severe anemia to clinically asymptomatic individuals. The total annual incidence of symptoms is estimated at about 1 in 100,000 individuals throughout the world. There are three main forms of thalassemia. thalassemia major, thalassemia intermedia and thalassemia minor. Individuals who have thalassemia major are seen to have severe anemia and require regular red blood transfusions. Observations in patients with thalassemia who were untreated or poorly transfused, as seen in some developing countries, are growth retardation, jaundice, poor musculature, pallor, hepatosplenomegaly, leg ulcers, and development of masses from extra medullary hematopoiesis. Skeletal changes may also result due to the expansion of bone marrow. Regular transfusion therapy, although necessary for survival, can lead to iron overload-related complications including endocrine complications (growth retardation, diabetes mellitus, failure of sexual maturation, and insufficiency of the parathyroid, thyroid, pituitary, and less commonly, adrenal glands), dilated myocardiopathy, liver fibrosis and cirrhosis)[1,-3].
Thalassemia intermedia is seen in older patients with moderate anemia and they do not require regular blood transfusions. Main clinical features are gallstones, painful leg ulcers, increased predisposition to thrombosis, hypertrophy of erythroid marrow with medullary and extramedullary hematopoiesis and its complications which include osteoporosis, masses of erythropoietic tissue that primarily affect the liver, spleen, lymph nodes, chest and spine, and bone deformities and typical facial changes. Thalassemia minor is clinically asymptomatic but moderate anemia is observed in some individuals. Beta-thalassemias are caused by point mutations or, more rarely, deletions in the beta globin gene on chromosome 11, leading to reduced (beta+) or absent (beta0) synthesis of the beta chains of hemoglobin. Transmission is autosomal recessive in most cases; however, reports have also shown dominant mutations. Diagnosis is based on hematologic and molecular genetic testing [4-8].
Presently prevalence of Thalassemia carrier in India is 3.7% of its total population. Annual increment of Thalassemia carrier is 50,000. Both Alpha and Beta Thalassemia are found in West Bengal, but Beta Thalassemia is most common in West Bengal.
Among the various Hemoglobinopathies, α- and β- thalassemia are common throughout the world. β-thalassemia is an autosomal recessive disorder of β- globin gene and about 7% of the global population are the carriers of this genetic trait. In Indian subcontinent, 2-3% of the general population and as high as 17% of certain high-risk communities are affected by β-thalassemia. App. 20,000 children are born each year in India with β-thalassemia major. Prenatal diagnosis holds the key role in prevention of this disease. Diagnosis of β-thalassemia in the 1st trimester by DNA analysis is a popular test because of the safety of termination of pregnancy if needed. The identification of the mutations in the parents and the fetus is carried out using various techniques. Altogether 785 mutations are already identified in β-globin gene and its flanking regions, of which 232 mutations are in β-globin gene causing phenotype of β-thalassemia. Β-globin gene cluster is a segment of DNA on chromosome 11 in humans which is about 60 kilo base pairs long (Figure 1&2).


The four related genes are arranged sequentially
During embryonic development, these genes are switched on and off by selective methylation and demethylation of the genes (Epigenetics). The chronological order of expression of these genes from the conception to childbirth is ε to δ to γ to β- globin sequence. Though fetal hemoglobin may persist after child birth, this genetic abnormality is known as Hereditary Persistence of Fetal Hemoglobin (HPFH). Both point mutations and insertion/ deletion of DNA sequences are known in β-globin gene. The correlation between genotype and phenotype are known in some cases of β- thalassemia but a lot remains to be understood. The most common mutation found in β-thalassemia both in western and eastern India is the point mutation G>C at position 5 in the first intervening sequence (IVS I, 5). The next most prevalent mutation is the deletion of 619 base pairs in the 3rd exon of β-globin gene in Sindhi population (Figure 3).

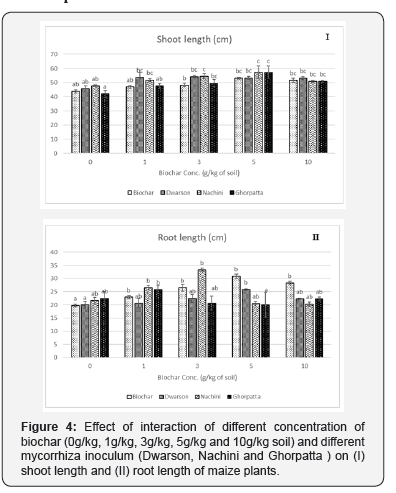
The two intervening sequences or introns separating the three exons should be spliced out during the processing of the heterogeneous nuclear (hnRNA) or pre-mRNA. But splicing defects due to mutations in or around the splice junctions produce abnormal hemoglobin. The following table from the article by Dr Chitra Thakur (Mahadik) published in Cardiovascular & Hematological Agents in Medicinal Chemistry (2012) gives the distribution of the mutations in three groups of high-risk population of western India (Total n = 371) (Table 1). This study was carried out at Wadia Hospital, Mumbai with patients from Maharashtra, Gujarat having a sizable Sindhi population. A similar study was carried out at Kolkata with Eastern Indian population (n= 660). The distribution of the different mutations is somewhat different (Figure 1). But the most prevalent mutation is the same IVS I-5 (G>C) all over India. However, not all the mutations were covered in both the studies (Figure 4).
References
- Orphanet Journal of Rare Diseases (2010).
- https://medlineplus.gov/ency/article/000587.htm
- https://ghr.nlm.nih.gov/condition/beta-thalassemia#genes.
- Thein SL (2013) The molecular basis of β-thalassemia. Cold Spring Harb Perspect Med 3(5): a011700.
- Nienhuis AW, Nathan DG (2012) Pathophysiology and Clinical Manifestations of the β-Thalassemias. Cold Spring Harb Perspect Med 2(12): a011726.
- Nelson Textbook of Pediatrics, 19th (Ed).
- Essentials of Haematology, 2nd (Ed) by Shirish M Kawthalkar.
- Bhattacharyya DM, Mukhopadhyay A, Basak J (2014) Descriptive profile of β-thalassemia mutations in West Bengal population: a hospital-based study 99(3): 345-353.