Sociodemographic, Health, and Caregiving Predictors of Labour Force Participation by Informal Caregivers Across the Palliative Care Trajectory
Denise Guerrierea1, Amna Husainb2, Denise Marshallc3, Brandon Zagorskia1, Julia Kennedya1 and Peter C Coytea1*
1Institute of Health Policy, Management and Evaluation, University of Toronto; 155 College Street; Toronto, Ontario, Canada
2Department of Family and Community Medicine, Temmy Latner Centre for Palliative Care, Mount Sinai Hospital; 60 Murray St; Toronto, Ontario, Canada
3Department of Family Medicine, McMaster University; 175 Longwood Road South; Hamilton, Ontario, Canada
Submission:April 14, 2025;Published: May 01, 2025
*Corresponding author:Peter C. Coyte, PhD Professor of Health Economics Institute of Health Policy, Management and Evaluation University of Toronto, Canada
How to cite this article: Denise G, Amna H, Denise M, Brandon Z, Julia K, et al. Sociodemographic, Health, and Caregiving Predictors of Labour Force Participation by Informal Caregivers Across the Palliative Care Trajectory. Palliat Med Care Int J. 2025; 4(5): 555648.DOI: 10.19080/PMCIJ.2025.04.555648
Abstract
Many caregivers of palliative care patients miss time from the labour market. This absence from employment has economic consequences for the family as well as for the labour force. This prospective, longitudinal study identified sociodemographic, health, and caregiving variables that influence Labour Force Participation for informal caregivers of home-based palliative care patients. Data were collected in bi-weekly telephone interviews to capture temporal changes in labour force activity, health service utilization, quality of life, and caregiving intensity over the course of a palliative care episode. Patient age and gender were obtained from the palliative care program databases. 262 caregiver-patient dyads were recruited from community-based palliative care programs within two regions. The probability of caregivers being employed full-time decreased by 26% for every 8-hour increase in caregiving time (p<0.01). Male caregivers had a lower probability of being not employed (p<0.05) and for every 10-year increase in care recipient age, the probability that the caregiver was unemployed increased by 13% (p<0.01). This information will be relevant to policy makers interested in reconfiguring the health system to better address the needs of palliative care patients and their families.
Keywords:Family caregivers; Labour force participation; Home-based palliative care
Introduction
Palliative care provides support to patients and their families when patients’ conditions are unresponsive to curative treatment and life-expectancy is relatively short [1-2]. Publicly financed home-based palliative care programs have been established to provide community and team-based multidisciplinary care, including practical and emotional support, to individuals at home. While care recipients receive a blend of publicly and privately financed home-based services [3], the viability of this care context relies on family members or close friends to provide the majority of the care [5-7]. The home palliative care environment is labour intensive and characterized by physical and emotional strain, where the informal caregiving demands can be enormous [5-8].
Current research demonstrates that many caregivers of palliative care patients miss time from the labour market [9-12] because of their expansive caregiving responsibilities in the home setting. This absence from employment has economic consequences for the family as well as for the labour force. Despite caregivers’ absence from the labour force, the opportunity cost of this foregone labour supply, has not been extensively studied. Moreover, because families and friends are intimately involved in the dying process and take on primary caregiving responsibilities, they bear significant financial, physical, and psychological costs. Although family and friends are the predominant care providers, there is a paucity of research exploring labour force participation (LFP) decisions during this profound, demanding time. In addition, a limited understanding of the variables that influence this participation decision exists.
There is an absence of quantitative research examining the effect of informal caregiving on LFP in a palliative care context. While some researchers have characterised family caregivers’ LFP in palliative care and advanced cancer settings using frequency counts and descriptive statistics [13-18], only two of these studies considered sociodemographic and care context predictors of presentism and absenteeism [4,17] and none considered determinants of LFP over time. Although a few studies [4,19] have measured home-based service utilization (e.g. personal support services) by palliative patients, the relationship between these services and LFP has not been examined. Moreover, Lilly and colleagues (2010) studied the intensity of caregiving and LFP using a cross-sectional survey, but this work was in the general caregiving context and focused on the threshold beyond which LFP became difficult for caregivers.
Accordingly, the purpose of this study was to assess the sociodemographic, health, and caregiving variables that influence caregivers’ participation in the labour force across the palliative care trajectory, that is, from palliative care admission to death. This study comprehensively assessed predictors of LFP that have not been previously considered in any caregiving environment, and particularly in the palliative setting. Temporal changes in factors such as labour force activity, health service utilization, and caregiving intensity that vary over the palliative care trajectory were measured. Longitudinal analyses allow for the identification of mechanisms that have currently been poorly documented in the literature to account for variations in LFP.
Methods
This study was a prospective, longitudinal cohort study designed to assess caregiver LFP and the relationship between an array of characteristics and intensity of LFP, from admission to death for two palliative care programs in Ontario, Canada. The framework used by Lilly and colleagues (2010) guided the selection, analysis and interpretation of predictors of LFP [21]. The factors used to predict the propensity (i.e. to be in or not in the labour force) and intensity (i.e. hours of work or full- or part-time employment) of LFP include: 1) sociodemographic variables (age, sex, marital status, education level, socioeconomic status); 2) health variables (functional status of patient, number of caregiver chronic conditions); and 3) caregiving environmental factors (amount of (publicly and privately financed) nursing, personal support and physician services, Emergency Department visits, hospitalizations, number of informal caregiving hours, and number of family caregivers.).
Study participants were recruited from two geographically distinct palliative care programs. In collaboration with existing care providers, these programs provide community and teambased multidisciplinary palliative care, including symptom and case management, and practical/emotional support to individuals at home 24 hours per day, 7 days per week. Each program is designed to shift the emphasis toward home-based end-of-life care and away from hospital-based care. These programs offer community-based palliative care in ethnically diverse regions; they have been in existence for several years, and therefore, reflect current practice in home-based palliative care.
Study participants were: 1) primary caregivers of patients who were admitted to one of the two palliative care programs within the past 14 days; 2) fluent in English; and 3) 18 years of age. In each palliative care program, the Research Officer telephoned eligible caregivers for the purpose of screening for inclusion and to ask if they would be interested in learning more about the study. The Research Officer verbally explained the study to interested participants and then mailed a written consent form to those who indicated that they wanted to participate. Fifteen potential predictors of LFP were measured. These predictors were chosen because they have been identified in previous studies, in general, and specifically related to LFP [21]. The predictor variables can be categorized into 3 domains: caregiving context; care recipient characteristics and caregiver characteristics.
Data were obtained from telephone interviews with participants and the databases for each of the palliative care programs. Study participants were interviewed every two weeks from admission into palliative care until death, and asked to report on LFP, health status, health service utilization, and quality of life (QOL) over the previous two weeks. LFP (the dependent variable) was assessed using an employment questionnaire developed and administered in previous studies [22-25] and that was adapted for this study by adding more questions regarding LFP. Respondents were asked if they were employed, and if so whether any changes had occurred, and the number of hours worked over the prior two weeks. Caregivers were classified according to our four employment categories: Full-Time (including self-employed individuals working >25 hours/week); Part-Time (including selfemployed individuals working <25 hours/ week); On-Leave; and Not-Employed (including retired, unemployed, and student). Each telephone interview lasted no more than 15 minutes. Two of the predictor variables (patient age and gender) were obtained from the respective palliative program databases. The remaining predictor variables were obtained from participant interviews using a demographic questionnaire. Caregiver QOL was measured by the Caregiver QOL Index – Cancer (CQOLC) [26-28]. Caregiver health status was assessed using the Canadian Community Health Survey Mental Health and Well-Being (Cycle 1.2) Chronic Conditions module (CCHS) (Statistics Canada, 2003). The CCHS consists of 33 questions addressing long-term conditions (6 months or longer) diagnosed by a health professional yielding the total number of chronic conditions. To collect data on the amount of privately and publicly financed services received, the Ambulatory and Home Care Record (AHCR), a comprehensive tool to measure the provision and receipt of services irrespective of payer [29]. The psychometric properties of the AHCR were evaluated in a study [29]; moderate to almost perfect agreement was found between participants’ responses on the AHCR and administrative data (kappa=0.41-1.00). The AHCR has been previously used in multiple studies for a range of clients and conditions [20, 24, 29, 30, 21, 31, 32, 33]. Functional Status was measured using the Palliative Performance Scale (PPS), also known as the modified Karnofsky Performance Scale [34,35]. The PPS assigns patient functional levels ranging from 0% (dead) to 100% (perfect functioning); the levels increase by 10% increments. An assessment of its reliability reported intraclass correlation coefficients ranging from 0.93 to 0.96 [34,35]. Neighbourhood income quintile for each care recipient was obtained by linking their postal code to the Statistics Canada Postal Code Conversion File (Statistics Canada). The variable was evaluated as an ordinal and categorical variable to identify non-linear relationships.
All data were linked using a patient anonymized identifier and stored in a relational database and programmed using SAS version 9.4 (SAS Institute). Ethics approval was obtained by all sites and the Universities. The multinomial logit regression model with marginal effects was fitted to estimate the effects of the covariates on the absolute additive increase in probability (i.e. percentage points) that a caregiver was in each employment category (e.g. Full Time). This model accommodates both fixed and time-varying covariates and adjusts the standard errors using both within and between caregiver variation. Multicollinearity was identified using variance inflation factor with a cut point above 2.5. Observations were excluded from analysis if there were missing values in any covariate. Data were modeled in Strata IC 14.2.
Results
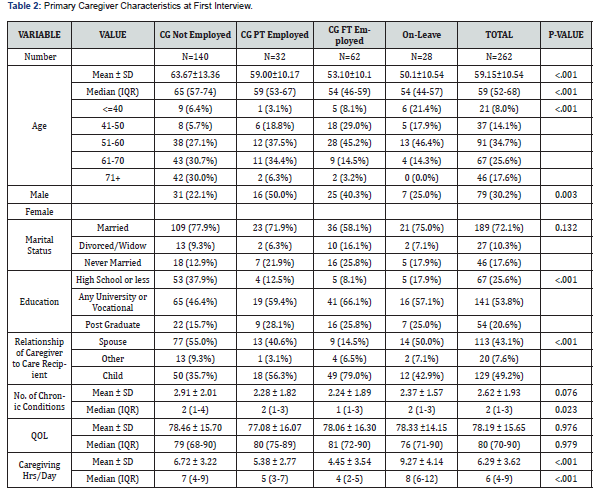
During the 26-month participant recruitment period (February 1, 2014 to April 5, 2016), 1,456 caregivers were identified as being potentially eligible for the study. The research officer contacted 964 (66.2% percent) eligible caregivers, with the remainder (n=492) unreachable by telephone. Some eligible caregivers (n=634) declined participation, and 57 care recipients died before their caregiver had been contacted. Consent to participate was given by 273 (28.3% of 964) caregivers. A further 11 caregivers were excluded because employment data were missing. Our results are based on a sample of 262 caregiver-patient dyads, yielding a total of 1,962 interviews. The mean and median number of days caregivers participated in the study (study entry until death of the care recipient) was 105 and 42, respectively. Tables 1 and 2 describe the sample of care recipients and caregivers, respectively, according to the caregivers’ employment status at the start of the study. The sample of care recipients was comprised of an equal number of males and females. Almost 70% of patients were >70 years of age. Most lived with at least one other person and the majority were married. Marital status of the care recipient differed by the caregiver’s employment status (p=0.01): Most caregivers were women, and more than half of the caregivers were between 51 and 70 years of age. On average, caregivers dedicated 6 hours per day to caregiving activities for the palliative care patient.
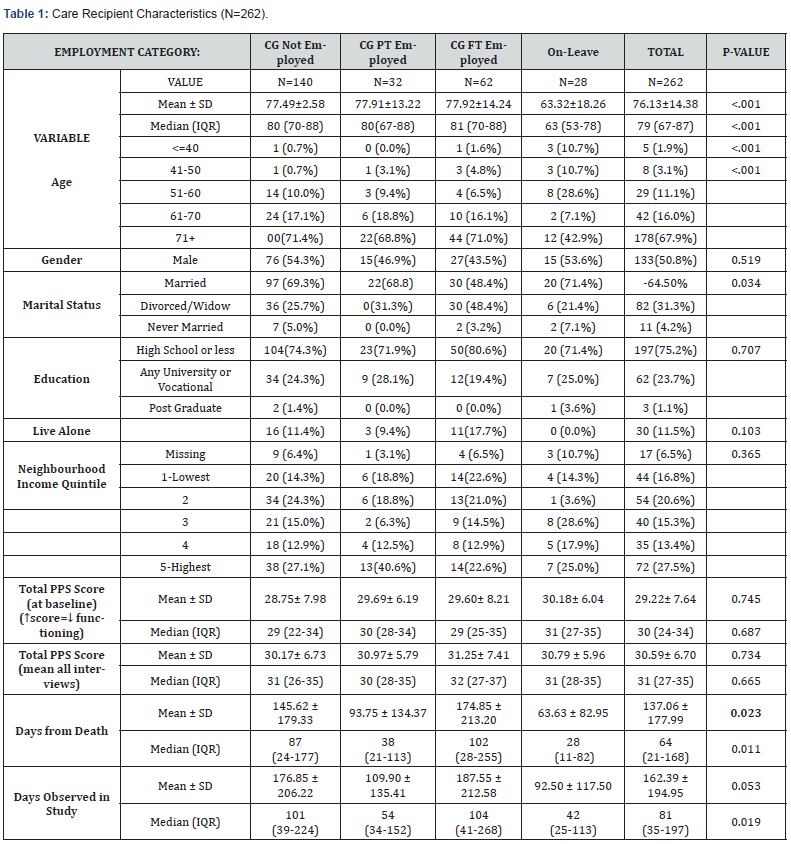
% = Column percentages
Table 3 reports the multinominal logit regression model after removing observations where some covariate data were missing for 28 caregivers, thereby yielding 1,611 interviews with 234 caregivers predicting 4 employment categories. The regression model yielded 6 statistically significant predictors of employment status; one is time dependent (caregiving hours per day) and five are time invariant covariates. Five of the six predictors significantly predicted FT employment, 2 predicted PT employment, 4 predicted On-Leave, and 6 predicted Not-Employed.
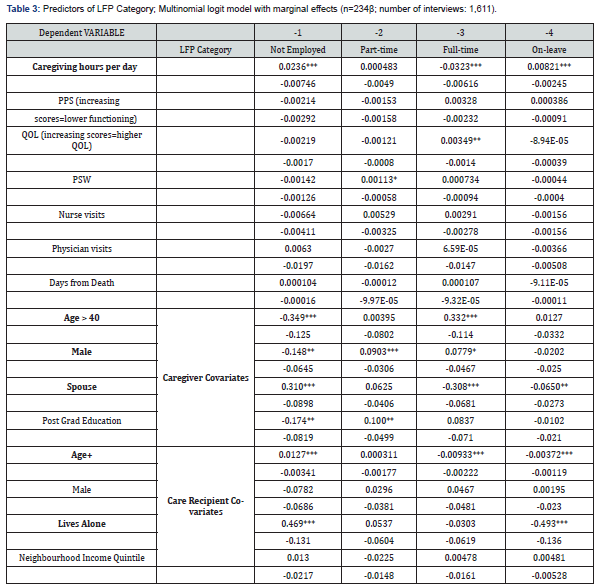
Caregiving Context Variables
One caregiving context variable was a statistically significant predictor of caregiver employment category on average, for each one hour increase in family caregiving time per day, the probability that a caregiver was employed FT decreased by 3% and the probability of being not employed or on-leave increased by 2% and 0.8%, respectively, over the trajectory. Therefore, for an 8 hour increase in caregiving hours per day, the probability of being employed FT would fall by 26%. [(8*0.0323) = 0.258 percentage points]. The provision of formal care services (Nursing, PSW, and physician) was unrelated to caregivers’ LFP category, however, there was a tendency towards a positive association between the receipt of PSW hours and being employed PT.
Caregiver Characteristics
Three caregiver characteristics were statistically significant predictors of caregiver LFP category. Caregivers older than 40 years of age, had a higher probability of being employed FT and a higher probability of being not employed. Male caregivers had a lower probability of being not employed and a higher probability of being employed PT. The probability that caregivers were unemployed increased by 30% when they were the spouse of the care recipient. Furthermore, the probability of being employed FT fell by 30% for spouses.
Care Recipient Characteristics
Two care recipient characteristics were statistically significant predictors of caregiver employment. The probability of being unemployed increased by 50% for those caregivers who were caring for a care recipient who lived alone while the probability of being on-leave decreased by the same percentage. As the age of the care recipient increased by one year, the probability of the caregiver being unemployed increased and the probability of being FT employed and on-leave fell. Specifically, for every 10- year increase in care recipient age, the probability of the caregiver being unemployed increased by 12.7% (1.27 x 10), while the probability of being employed FT fell by 9.3% and being On-leave fell by 3.7%.
Discussion
While family caregivers undertake most of the caregiving workload, there is a paucity of research that has comprehensively assessed this responsibility and how it affects economic and health outcomes. This study examined important issues in the provision of home-based palliative care. Understanding the determinants of LFP may inform the targeting of services to support families balance employment and caregiving. Herein, we compare our results to previous studies in the palliative care context, as well as to those studies outside of palliative care given the small number of studies addressing the same sets of predictor variables used in our study.
Because of the intensive caregiving demands, interventions designed to assist palliative caregivers should aim to support both their employment and their caregiving. Support can be offered to palliative caregivers by educating employers on the characteristics of the palliative care trajectory, which typically is relatively short in duration. Being more flexible when possible and allowing time off while maintaining employment are methods of assistance. Elsewhere, we discuss more detailed policy implications for informal palliative caregiving [36].
In this current study, a statistically significant relationship between LFP and physician, nursing or PSW services was not found. This was not surprising given the lack of consensus in the literature concerning these relationships [37-39]. In some cases, the provision of skilled [39] services, such as nursing, complements unpaid caregiving, and raise hours of unpaid caregiving. Alternatively, for some other services, such as those provided by PSWs, service provision substitutes for unpaid caregiving and reduces hours of unpaid caregiving [40-42]. Further investigation into the relationship between health care services and other variables such as quality of life is needed.
We found that female caregivers had a higher probability (15%) of being unemployed. Findings in the literature report incongruous results for gender, albeit in relation to employment variables that differ from our employment categories. In a study with terminal cancer patients, women were more likely to experience employment difficulties; the employment variable in their study comprised missed time from work and managing employment demands. Although Mazanec and colleagues (2011) did not find a relationship between gender and employment, their variable of interest was productivity loss, which consisted of hours missed from employment and workplace productivity [15]. Survey studies in the general caregiving context also reported that women who provided higher amounts of care were more likely to decrease working hours or to quit [42,43].
As the age of the care recipient increased, the probability that the caregiver was unemployed increased while the probability of being employed FT fell. The palliative care literature has not specifically examined the relationship between care recipient age and our categories of employment, and additionally, those studies have not corroborated our observation - care recipient age was neither a predictor of productivity loss [15] nor employment difficulties [17]. In our study, the probability that caregivers were unemployed increased when they were the spouse of the care recipient. Furthermore, the probability of being employed FT and on-leave fell for spouses [15]. A previous study reported that palliative caregivers who were married to the care recipient had a greater productivity loss, and those employed caregivers were more likely to be in a non-spousal relationship with the care recipient. In a general caregiving survey, female caregivers who cared for their spouse were more likely to leave the labour force than females who were not caregivers [43].
We report that when care recipients lived alone, the probability that the caregiver was unemployed increased 50%. This may be because providing care outside of one’s home requires more coordination as one physically moves in and out of a care recipients’ home. In addition, the probability of being on-leave fell for caregivers of care recipients living alone. Our results on cohabitation status have not been corroborated in the general caregiving literature, however, these studies used an employment variable that differed from our employment status variable. Contrary to our study, caregivers of frail elderly who did not live with the care recipient had the lowest risk of reducing their work hours [14]. Furthermore, another study reported that employed caregivers were more likely to not reside with the care recipient with advanced cancer (15). Finally, in a previous study in a non-palliative context, caregivers providing care to an individual in the same household were more likely to stop working [43]. Understanding that caregivers may vary in their employment status because of differences in their caregiving environments and the demographics of care recipients and caregivers, assists health professionals and employers in their assessment of those who may be at higher risk of not maintaining their employment over the palliative trajectory. Elsewhere, we outline details regarding supportive responses from employers and areas for improvement and outreach to caregivers during this extremely emotional and physically demanding time [36]. Given that these informal caregivers are providing care that would otherwise be provided in an institution, we need to ensure that all is done to protect their usual work life and provide compassionate support.
Limitations
The results of this study may lack generalizability as the study participants were drawn from two palliative care programs. The findings may not necessarily transfer to care recipients receiving services outside of these formal palliative care programs. However, the populations served by these two programs are diverse in terms of their clinical, demographic, and ethnic backgrounds, which may help to improve generalizability. Additionally, selection bias of respondents may exist in this study. However, this risk is likely minimal because the study sample is similar to caregivers in the broader population, and used in previous studies based on age, gender, and relationship to the care recipient [44-46]. Finally, participants’ responses regarding health care services and their caregiving time rely on their recall. However, a recall period of 2 weeks was chosen based on our previous work indicating that respondents’ recall over a two-week period is reliable when compared to administrative data33 [47-55].
Conclusion
Despite the need for the delivery of efficient and effective palliative care, a limited understanding of the predictors of LFP in the population of palliative caregivers currently exists. Care providers, administrators and other decision-makers across the policy spectrum are disadvantaged by this lack of knowledge. This study begins to build research capacity to respond to this shortfall in knowledge. A greater appreciation of the variables that predict LFP are necessary for practitioners, health managers, and policy decision makers to ensure that patients and their caregivers receive efficient and effective care as well as more general supports. By assessing determinants of labour force participation, issues concerning financial loss and other foregone opportunities are highlighted.
References
- Abu-Saad H (2001) Evidence based palliative care - across the life span. Oxford London: Blackwell Science Ltd.
- Twycross G (1997) Introducing Palliative Care. 2nd ed. Oxford: New York: Radcliffe Medical Press.
- Carstairs S (2000) Quality End-of-Life Care: The Right of Every Canadian. Standing Senate Committee on Social Affairs, Science and Technology
- Wolff JL, Dy SM, Frick KD , Kasper JD (2007) End-of-life care: Findings from a National Survey of Informal Caregivers. Arch Intern Med 167(1): 40-46.
- Munck B, Fridlund B, Mårtensson J (2008) Next-of-kin caregivers in palliative home care--from control to loss of control. J Adv Nurs 64(6): 578-586.
- Rabow MW, Hauser JM, Adams J (2004) Supporting Family Caregivers at the End of Life: “They Don’t Know What They Don’t Know.” JAMA 291(4): 483-491.
- Thomas C, Morris SM, Harman JC (2002) Companions through cancer: The care given by informal carers in cancer contexts. Soc Sci Med 54(4): 529-544.
- Brazil K, Bédard M, Willison K, Hode M (2003) Caregiving and its impact on families of the terminally ill. Aging Ment. Health 7(5): 376-382.
- Grunfeld ED, Coyle T, Whelan J (2004) Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ 170(12): 1795-801.
- Covinsky KE, Goldman L, Cook EF (1994) The impact of serious illness on patients’ families. JAMA 272(23); 1839-1844.
- Stommel MC, Given W, Given BA (1993) The cost of cancer home care to families. Cancer 71(5):1867-1874.
- Eldh AC, Carlsson E (2011) Seeking a balance between employment and the care of an ageing parent. Scandinavian Journal of Caring Sciences 25(2): 285-293.
- Rowland CB, Hanratty M, Pilling B (2017) The contributions of family caregivers at end of life: A national post-bereavement census survey of cancer carers’ hours of care and expenditures. Palliat Med 31(4): 346-355.
- Covinsky KE, Eng C, Lui LY (2001) Reduced employment in caregivers of frail elders: Impact of ethnicity, patient clinical characteristics, and caregiver characteristics. J Gerontol A Biol Sci Med Sci 56(11): M707-713.
- Mazanec SR, Daly BJ, Douglas SR, Lipson AR (2001) Work productivity and health of informal caregivers of persons with advanced cancer. Res Nurs Health 34(6):483-95.
- Cui J, Song LJ, Zhou LJ (2014) Needs of family caregivers of advanced cancer patients: A survey in Shanghai of China. Eur J Cancer Care 23(4): 562-569.
- Rossi PG, Beccaro M, Miccinesi G (2007) Dying of cancer in Italy: Impact on family and caregiver. The Italian survey of dying of cancer. J Epidemiol Community Health 61(6): 547-554.
- Addington-Hall JM, MacDonald MLDD, Anderson HRR (1992) Randomised controlled trial of effects of coordinating care for terminally ill cancer patients. BMJ 305(6865): 1317-1322.
- Brazil K, Bédard M, Willison K (2005) Service Preferences Among Family Caregivers of the Terminally Ill. J Paliatl Med. 8 (1): 69-78.
- Lilly MB, Laporte A, Coyte PC (2010) Do they care too much to work? The influence of caregiving intensity on the labour force participation of unpaid caregivers in Canada. J Health Econ 29(6): 895-903.
- Cai J, Zhang L, Guerriere DN, Coyte PC (2021) The determinants of the intensity of home-based informal care among cancer patients in receipt of home-based palliative medicine. Palliat Med 35(3): 574-583.
- Nonoyama ML, Katz SL, Amin R (2020) Healthcare Utilization and Costs of Pediatric Home Mechanical Ventilation in Canada. Pediatr Pulmonol 55(9): 2368-2376.
- Guerriere DN, Zagorski B, Fassbender K (2010) Cost variations in ambulatory and home-based palliative care. Palliat Med 24(5): 523-532.
- Guerriere DN, Husain A, Marshall D (2015) Predictors of place of death for those in receipt of home-based palliative care services in Ontario, Canada. J Palliat Care 31(2): 76-88.
- Guerriere DN, Husain A, Zagorski B (2016) Predictors of caregiver burden across the home-based palliative care trajectory in Ontario, Canada. Health Soc. Care Community 24(4): 428-438.
- Weitzner MA, Jacobsen PB, Wagner HJ (1999) The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res8(1-2): 55-63.
- Ozer ZC, Firat MZ, Bektas HA (2009) Confirmatory and exploratory factor analysis of the caregiver quality of life index-cancer with Turkish samples. Quality of Life Research 18(7): 913-921.
- Ozer ZC, Firat MZ, Bektas HA (2009) Confirmatory and exploratory factor analysis of the caregiver quality of life index-cancer with Turkish samples. Quality of Life Research 18(7): 913-921.
- Guerriere DN, Ungar WJ, Corey M, Croxford R, Tranmer JE et al. (2006) Evaluation of the ambulatory and home care record: Agreement between self-reports and administrative data. Int J Technol Assess Health Care 22(2): 203-210.
- Guerriere DN, Wong AYM, Croxford R (2008) Costs and determinants of privately financed home-based health care in Ontario, Canada. Health Soc. Care Community 16(12): 126-136.
- McGillion MH, Croxford R, Watt-Watson J (2008) Cost of illness for chronic stable angina patients enrolled in a self-management education trial. Can J Cardiol 24(10): 759-64.
- Stevens B, Guerriere DN, McKeever (2006) The economics and efficacy of home versus hospital breastfeeding support for newborns: A randomized controlled trial. J Adv Nurs 53(2): 233-43.
- Tsimicalis A, Stevens B, Ungar WJA (2011) prospective study to determine the costs incurred by families of children newly diagnosed with cancer. Psychooncology 21(10): 1113-1123.
- Downing M, Lau F, Lesperance M (2007) Meta-analysis of survival prediction with Palliative Performance Scale. J Palliat Care 23(4):245-252.
- Ho F, Lau F, Downing M, Lesperance M A (2007) Reliability and validity study of the Palliative Performance Scale. BMC Palliative Care 7(10).
- Guerriere DN, Husain A, Marshall D (2020) Transitions in Labour Force Participation over the Palliative Care Trajectory. Healthcare Policy 16(2): 25-40.
- Sun Z, Guerriere DN, de Oliveria C, Coyte PC (2019) Does informal care impact utilization of home-based formal care services among end-of-life patients? A decade of evidence from Ontario, Canada. Health Soc. Care Community 27(2): 437-448.
- Mentzakis E, McNamee P, Ryan M (2008) Who cares and how much: exploring the determinants of co-residential informal care. Rev Econ Household 7: 283-303.
- Bonsang E (2009) Does informal care from children to their elderly parents substitute for formal care in Europe? J Health Econ 28(1): 143-154.
- Van Houtven, CH, Norton EC (2004) Informal care and health care use of older adults. J Health Econ 23(6): 1159-1180.
- Bolin K, Lindgren B, Lundborg P (2008) Informal and formal care among single‐living elderly in europe. Health Econ 17(3): 393-
- Berecki-Gisolf JJ, Lucke R, Hockey R (2008) Transitions into informal caregiving and out of paid employment of women in their 50s. Soc Sci Med 67(1): 122-127.
- Carr E, Murray ET, Zaninotto P (2018) The Association Between Informal Caregiving and Exit from Employment Among Older Workers: Prospective Findings From the UK Household Longitudinal Study. J Gerontol B Psychol Sci Soc Sci 73(7): 1253-1262.
- Holley CK, Mast BT (2009) The Impact of Anticipatory Grief on Caregiver Burden in Dementia Caregivers. The Gerontologist 49(3): 388-396.
- Macchi ZM, Koljack CE, Miyasaki JM (2020) Patient and Caregiver Characteristics Associated with Caregiver Burden in Parkinson’s Disease: A Palliative Care Approach. Ann Palliat Med 9(Suppl 1): S24-S33.
- Pinto C, Bristowe K, Witt J (2018) Perspectives of Patients, Family Caregivers and Health Professionals on the Use of Outcome Measures in Palliative Care and Lessons for Implementation: A Multi-Method Qualitative Study. Ann Palliat Med 7(Suppl 3): S137- 50.
- Brazil K, Bédard M, Willison K, Hode M (2003) Caregiving and its impact on families of the terminally ill. Aging Ment. Health 7(5): 376-382.
- Brazil K, Bédard M, Willison K (2005) Service Preferences Among Family Caregivers of the Terminally Ill. J Paliatl Med. 8 (1): 69-78.
- Cai J, Zhang L, Guerriere (2021) Where do cancer patients in receipt of home-based palliative care prefer to die and what are the determinants of a preference for a home death? Int J Environ Res Public Health 18(1): 235.
- Guerriere DN, Tullis E, Ungar WJ (2006) Economic burden of ambulatory and home-based care for adults with cystic fibrosis. Treat Respir Med 5(5): 351-359.
- Stabile M, Laporte A, Coyte PC (2006) Household responses to public home care programs. J Health Econ 25(4): 674-701.
- SAS version 9.0, SAS Institute Inc., Cary, NC.
- Statistics Canada. Canadian Community Health Survey - Mental Health and Well-Being (Cycle 1.2), Chronic Conditions module.
- Twycross G (1997) Introducing Palliative Care. 2nd ed. Oxford: New York: Radcliffe Medical Press.
- Cancer pain relief and palliative care - Technical report series. Geneva: World Health Organization; 1990. Report No.: 804.






























