Do POLST (Physician Orders for Life-Sustaining Treatment) Forms Pose Ambiguity?
Nitasa Sahu*, Cynthia Woods, Rohit Jain and Hyma Polimera
PennState Hershey Medical Center, USA
Submission: September 13, 2019; Published: September 18, 2019
*Corresponding author: Nitasa Sahu, PennState Hershey Medical Center, USA
How to cite this article:Nitasa S, Cynthia W, Rohit J, Hyma P. Do POLST (Physician Orders for Life-Sustaining Treatment) Forms Pose Ambiguity?. Palliat Med Care Int J. 2019; 3(1): 555602. DOI: 10.19080/PMCIJ.2019.03.555602
Abstract
With the average life expectancy increasing to 78 years old in the U.S according to the CDC, many patients have chronic progressive illnesses that may or may not improve with medical management/hospitalization. Discussing goals of care are important for every person, so they can manage their illness in certain circumstances. The National POLST (Physician Orders for Life Sustaining Treatment) Paradigm is, “an approach to end-of-life planning that emphasizes eliciting, documenting and honoring patients’ preferences about the medical treatments they want to receive during a medical crisis or as they decline in health.” Many states utilize these forms and may be worded differently, however, essentially have the same information. We present a case scenario for an encephalopathic patient who had previous advanced directives indicating, “Limited additional interventions,” “no antibiotics,” and “no hydration/artificial nutrition by tube.” The surrogate, however, did want intravenous (IV) nutrition. The question is, does Total Parental Nutrition (TPN) coincide with the patient’s wishes given the statement on the POLST form mentions “no artificial nutrition by tube.” Should our POLST forms be revised to include the forms of artificial nutrition (IV or PEG) to avoid ambiguity?
Mini Review
The vision of the paradigm is to honor ones wishes for medical personnel at that moment of crisis with a POLST form. This form, however, is not intended for every individual, rather for those that have a severe illness, a life expectancy of less than 1 year, and/or a condition where one is not expected to recover. Many states utilize these forms and may be worded differently, however, essentially have the same information. It is vital that this form be explained in lay-man terms and discussed in detail of each section because it can be interpreted differently. One such example of the various sections of the Pennsylvania POLST form are seen below. One section to focus on is Section D labeled, “Artificially administered Hydration/Nutrition.” The check off boxes are displayed in the figure with attention given to the wording of “by tube.” Is this to be under the assumption it includes total parenteral nutrition (TPN)? Do providers mention such during their discussion? [1].
We present you a case of a 94 year old female wheelchair-bound admitted for encephalopathy secondary to UTI and worsening oral intake for the past week. The patient was accompanied by two daughters who were aware she had advanced directives that demonstrated “full code” back in 1998, however, knew of a more contemporary document with further wishes, but were unaware of details due to the third daughter being the surrogate. A POLST was found in her chart from 2016 showing “Limited additional interventions”, “no antibiotics”, and “no hydration and artificial nutrition by tube” with “no hydration” striked out with a penned in statement, “Fluids ok” as seen in Figure 1. This was discussed with the third daughter who agreed to this, however, wanted IV nutrition for her mother. The question is, does TPN coincide with the patient’s wishes given the statement on the POLST form mentions no artificial nutrition by tube [2-4].
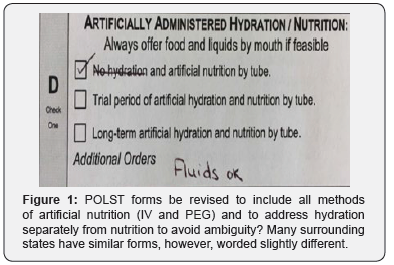
(Figure 1) Should our POLST forms be revised to include all methods of artificial nutrition (IV and PEG) and to address hydration separately from nutrition to avoid ambiguity? Many surrounding states have similar forms, however, worded slightly different. For example, Maryland’s Medical Orders for Life Sustaining Treatment (MOLST) form, delineates between artificially administered fluids and nutrition as separate entities seen below but do not mention IV and PEG.
a) May give artificially administered fluids and nutrition, even indefinitely, if medically indicated
b) May give artificially administered fluids and nutrition, if medically indicated, as a therapeutic trial
c) May give fluids for artificial hydration as a therapeutic trial, but do not give artificially administered nutrition
d) Do not provide artificially fluids or nutrition
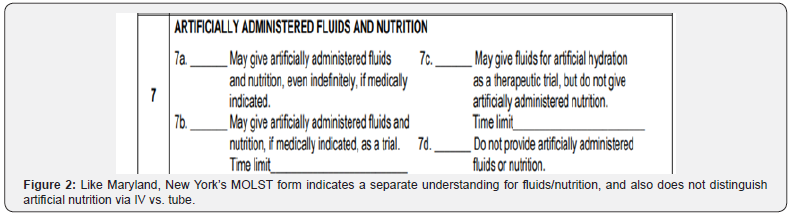
(Figure 2) Like Maryland, New York’s MOLST form indicates a separate understanding for fluids/nutrition, and also does not distinguish artificial nutrition via IV vs. tube.
a) No feeding tubes
b) A trial period of feeding tube
c) Long-term feeding tube if needed
d) no IV fluids”
e) trial of IV fluids
If we look at Pennsylvania’s below, hydration and nutrition are mentioned, however, it does not allow just one or the other. While it does mention “by tube,” it does not mention IV nutrition (Figure 3).
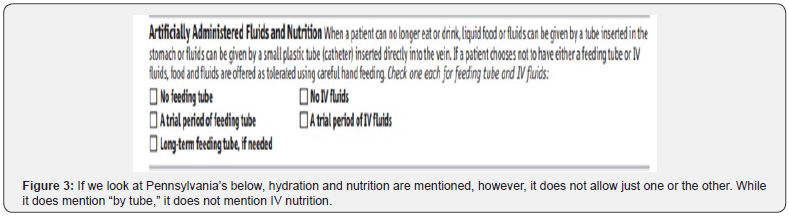
a) no hydration and artificial nutrition by tube
b) trial period of artificial hydration and nutrition by tube
c) Long-term artificial hydration and nutrition by tube
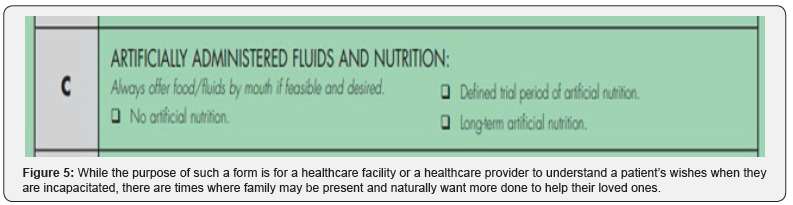
Similarly, New Jersey’s Practitioner’s Orders for Life Sustaining Treatment (POLST) seen below, there is no mention of hydration or explanation of the artificial method (Figure 4).
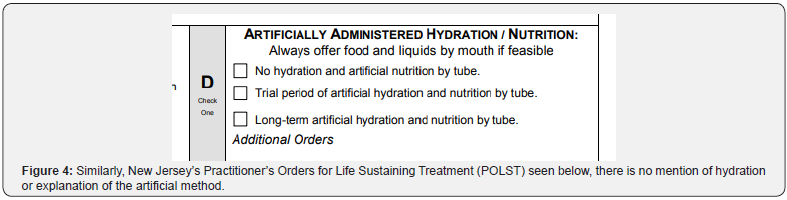
a) no artificial nutrition
b) defined trial period of artificial nutrition
c) long-term artificial nutrition.
While the purpose of such a form is for a healthcare facility or a healthcare provider to understand a patient’s wishes when they are incapacitated, there are times where family may be present and naturally want more done to help their loved ones. This, in turn may be against the patient’s actual wishes and may only hasten their loved one’s natural death (Figure 5). Some solutions to avoid ambiguity in these important forms include separately addressing hydration and artificial nutrition. Under artificial nutrition, it should delineate between tube vs. parenteral route. An additional recommendation is for every practitioner to thoroughly explain each choice carefully to both the patient and family and reassess periodically as their medical condition alters. Of the four forms, New York may exemplify the most thorough and simple to use that prompts practitioners to mention what each option entails rather than a checklist that may be ambiguous.