Dignity at the Termination of Life Care: An Integrative View
Ashu Chaudhary* and Ashima Sharma
Department of Chemistry, Kurukshetra University, India
Submission: July 18, 2019; Published: August 13, 2019
*Corresponding author: Ashu Chaudhary, Department of Chemistry, Kurukshetra University, India
How to cite this article: Ashu Chaudhary, Ashima Sharma. Dignity at the Termination of Life Care: An Integrative View. Palliat Med Care Int J. 2019; 2(5): 555598. 10.19080/PMCIJ.2019.02.555598
Abstract
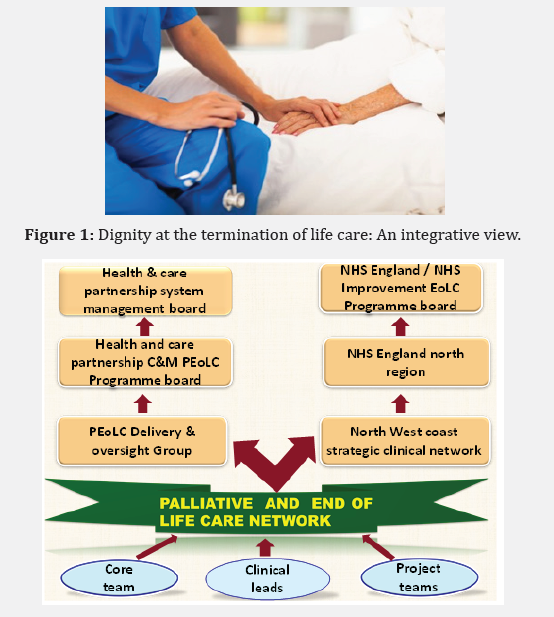
Dignity is a life long, common need that is mandatory to a person wellbeing. It means feeling a perception of worth or honour. Near the end of life, most people have less control over their entity due to illness. Dignity is well known concept in nursing. Grandeur during end-of-lifecare has become one of the most critical issue facing patients facing during hospitalization .In this article end-of-life care include hospice and palliative care, both of which aim to improve the quality of life of patients facing life threatening illness and their families . Dignity is perceived as a basic requirement that must be met in caring for dying patients. The basic tenets of end-of-life care could be summarized as improving the quality of life and maintaining the dignity of the dying person. Furthermore, human dignity is an essential value embedded in nursing practice, it is a component of the International Council of Nurses (ICN) Code of Ethics, and it is an overarching value which shapes the delivery of service to dying individuals. Understanding dignity as a concept is crucial to developing knowledge in health-related disciplines; the concept will influence people’s understanding, attitudes, and behaviors toward caring with dignity in health-care situations. Maintaining patient dignity is something we often hear mentioned when discussing the principles of palliative care; however it is possible that this almost becomes a phrase of vain repetition with little relevance to the quality of care the patient actually receives (Figure 1) (Graphical abstract).
Keywords: Dignity; Palliative care; Dying with dignity; End-of-life care
Abbrevations: ICN: International Council of Nurses;
Introduction
Dignity is considered to be an attribute of a good death for terminal patient [1]. Human dignity has become an important aspect of health and social care. It has been explored using several methods, including critical and philosophical thinking, analyzing the concept historically, asking or observing people to understand their perceptions of dignity, and empirically examining how certain groups of persons use the word [2,3]. Dignity is considered to be an attribute of a good death for terminal patients. End-of-life care, with the purpose of relieving suffering through intensive physical and psycho-spiritual care, is often philosophically rooted in the acknowledgment of the inherent dignity of each person. Firstly, one may ask the question ‘What is dignity’? The word dignity originates from two Latin words, dignitus (merit) and dignus (worth). The International Council for Nurses Code of Ethics 2012 instructs that the observance of dignity should not be limited by the individual’s age, colour, creed, culture, gender, sex, nationality, race, social status, or health status. However, while dignity is accepted as a universal need which is fundamental to the well-being of every individual in all societies, the actual ‘practical’ meaning of dignity remains complex and unclear because it is a multi-dimensional.
Loss of Dignity
Talking about loss of dignity I would propose that there is no clear distinction between dignity being present or lost in end-oflife care; rather loss of dignity is a spectrum and is subjectively experienced. A case report highlighted aspects of losing one’s dignity as ‘insults’; in this example the lady was most bothered by junior members of staff addressing her by her forename and having to wear poorly-fitting hospital gowns. A longitudinal study found that a downward trend in the sense of dignity following admission to a nursing home was associated with the feeling of a loss of control and a loss of self-worth [4].
Importance of Dignity
Unsurprisingly, no-one appears to have studied whether or not patients and/or healthcare professionals believe dignity in end-of-life care is important, nor have they tried to quantify ‘how much’ dignity is required. “The secret of the care of the patient is in caring for the patient” are words which were delivered by Dr. Francis Peabody in his famous address to Harvard medical students in 1925 18. Why? I‘caring’ aspect of care is lacking. A lack of caring may result in the patient t is no surprise that patients and families are less satisfied with medical encounters when the being less forthcoming with concernsleading to missed treatment opportunities, medical errors, and ultimately compromised patient safety. Furthermore, studies consistently show that most complaints against healthcare professionals derive, not from medical errors, but from a failure to communicate and the absence of caring – in other words, compromised patient dignity [5].
Promotion of Dignity
As touched on previously, dignity can be upheld by measures such as symptom control; promoting independence, privacy, social support and a positive tone of care ; listening, giving appropriate information, having a caring bedside manner [6]; and showing respect, empathy and companionship. Spiritual care has been shown to be facilitated by having sufficient time, employing effective communication, and reflecting on one’s personal experiences. It is clear that involvement of the palliative care team encourages a sense of dignity as the emphasis is less on the disease and more on the person. Measures such as getting acquainted with new living structures or involvement with staff and other residents have been shown to encourage a sense of dignity among nursing home residents-measures which may be transferred to palliative care units [7].
Factors that Influence Dignity
Demographic factors
Compared with older patients, younger patients tended to have a fractured sense of dignity. Women were more likely to relate more factors to their perceptions of dignity than men [8]. Individuals with more education tended to assign dignity implications to more factors than individuals with less education
Treatment- and care-related factors
Treatment and care are important issues that influence dying patients’ dignity. Poor symptom management, or treatment without empathy and affection, combined with the effects of illness, can result in diminished dignity. Poor medical care diminishes dignity at the end of life, while appropriate and qualified care maintains and improves it [9]. However, as the illness progresses, the increasing need for help and care represents a major threat to dignity.
Other Factors
Lack of resources and poor organization, including insufficient time to provide care, lack of competent staff, and lack of teamwork, can erode a dying person’s dignity. A safe, calm, and private living environment promotes the patient’s sense of dignity. Social support from a helpful community of friends, family, and health-care providers was identified as a factor that positively affected patients’ dignity.
Conclusion
This review clarified the meaning of dying with dignity by identifying themes across studies that can be easily understood by readers and synthesized common aspects of dignity in end-oflife care. As a basic human right, all humans have the right to die with dignity. As a subjective experience, dignity is intrinsically constructed with a particular self and perceived in terms of personal values and standards, thus dying with dignity may mean different things to different individuals. Simple measure such as the PDQ and life storytelling can help healthcare professionals view the patient receiving end-of-life care as a person; thereby helping them to promote patient dignity and address needs which would otherwise not be known
Acknowledgement
One of the authors Ashima Sharma would like to express special thanks of gratitude to Dr. Monika Verma, Principal, Tika Ram PG Girls College, Sonipat, Haryana for supporting this work
References
- Yalden BJ, McCormack B (2010) Constructions of dignity: a pre-requisite for flourishing in the workplace? Int J Older People 5(2): 137-147.
- Gallagher A, Li S, Wainwright P (2008) Dignity in the care of older people-a review of the theoretical and empirical literature. BMC Nurs 7: 11.
- Sulmasy DP (2013) The varieties of human dignity: a logical and conceptual analysis. MedHealth Care Philos 16(4): 937-944.
- Oosterveld-Vlug MG, Pasman HR, Gennip VIE, Willems DL, Onwuteaka-Philipsen BD, et al. (2013) Changes in the personal dignity of nursing home residents: a longitudinal Qualitative Interview study. PLoS One 8(9): e73822.
- Chochinov HM (2013) Dignity in care: time to take action. J Pain Symptom Manage 46(5): 756-759.
- Beach MC, Forbes L, Branyon E, Aboumatar H, Carrese J, et al. (2015) Patient and family perspectives on respect and dignity in the intensive care unit. NarratInq Bioeth 5(1A): 15A-25A.
- Chochinov HM, Kristjanson LJ, Hack TF, Hassard T, McClement S, et al. (2006) Dignity in the terminally ill: revisited. J Palliat Med 9(3): 666-672.
- Chochinov HM (2002) Dignity-conserving care-a new model for palliative care: helping the patient feel valued. JAMA 287(17): 2253-2260.
- Enes SPD (2003) An exploration of dignity in palliative care. Palliative Med 17(3): 263- 269.






























