Palliative Care in the Brazilian Health System
Araujo Laís Záu Serpa1*, Araujo Carolina Záu Serpa2, Barros Luiz Henrique Rosendo3, Espírito Santo Matheus Nascimento4 and Guilherme Fábio da Silva5
1Professor of Bioethics and Medical Ethics, Universidade Estadual de Ciências da Saúde de Alagoas, Brazil
2Clinical Oncologist and Palliative Care Specialist, Hospital Santa Casa de Misericórdia de Maceió, Brazil
3Resident Physician of Psychiatry, Hospital de Saúde Mental Professor Frota Pinto, Brazil
4Resident Physician of Orthopedics, Hospital Geral do Estado de Alagoas, Brazil
5Physician of the Brazilian Army, Brazil
Submission:June 21, 2019; Published: June 27, 2019
*Corresponding author: Laís Záu Serpa de Araujo, Professor of Bioethics and Medical Ethics, Universidade Estadual de Ciências da Saúde de Alagoas, Brazil
How to cite this article: Araujo Laís Záu Serpa, Araujo Carolina Záu Serpa, Barros Luiz Henrique Rosendo, Espírito Santo Matheus Nascimento, Guilherme Fábio da Silva. Palliative Care in the Brazilian Health System. Palliat Med Care Int J. 2019; 2(4): 555595 10.19080/PMCIJ.2019.02.555595
Abstract
Palliative care is indicated for patients with life-threatening illness. The goal is to promote relief from the suffering of patients and to treat their needs, not only physical pain but also spiritual, social and emotional pain. A necessary condition is that such care should be developed by a transdisciplinary team and also applicable to the family. Objective: identify palliative care services in the Brazilian health system. Method: descriptive research, through official documents about the health system. The sample consisted of documents on palliative care services in Brazil, available on the internet. The results show that there are palliative care services in all regions of Brazil, with a greater concentration in the Southeast region. It was also found that most of the services work in hospitals and most attend patients of the public health system. Conclusion: in Brazil the number of palliative care services is small in relation to demand and most are specialized for cancer patients. It is necessary to create new palliative care services in Brazil, that there is disclosure to doctors, other health professionals, patients and family members. It is necessary to create new palliative care services in Brazil, that there is disclosure to doctors, other health professionals, patients and family members. It is also necessary to create a State policy so that palliative care can be valued so that the culture of palliative care can be developed and so relieve the suffering of patients and, consequently, improve the quality of life.
Descriptors: Palliative Care; Public Health; Quality of Life
Introduction
Palliative care is a modality of attention to the patient with life-threatening disease. The alternative of palliative care favors the continuity of the patient’s life, involving physical, emotional, social, spiritual and cultural aspects, in order to improve the quality of life, reducing the signs and symptoms of the disease [1,2]. Palliative care follows principles and is indicated since the diagnosis to give quality of life to the patient. It is estimated that 20 million people in the world die without access to palliative care, which could minimize the suffering and pain of patients and their families. Palliative care is considered a part of the health care systems and a fundamental element of citizens’ rights [3]. Should be directed according to the patient’s needs, considering its values, preferences, dignity and autonomy [4,5].
Palliative Care services can be offered by private institutions, whether or not for profit, with or without public resources, and also by the public health system itself. In Brazil, the public health system is regulated by Law 8080/19906, whose article 2nd establishes that: “Health is a fundamental right of the human being, and the State must provide the conditions necessary for its full exercise.” Thus, it is evident that health, besides being a fundamental right, it is for the State to promote the conditions for citizens to exercise this right. However, when the state does not fulfill its obligations and disrespects this fundamental right, invariably it will increase the suffering of the patients.
Palliative Care
The term palliative originates in the Latin word palliun, which means mantle, protection, that is, to protect those whom curative medicine no longer welcomes [1]. Its concept originated in the movement hospice, idealized Dame Cecily Saunders, in the United Kingdom in 1967, having described the philosophy of the patient care that is dying [6,7]. Palliative care follows the precepts of reaffirming the importance of life. Palliative care is defined as active and integral care oriented to patients with diseases that no longer respond to healing therapies, and it aims to improve the lives of those individuals and their family members by relieving pain and biopsychosocial and spiritual issues [1].
Palliative Care has basic principles to guide care. The field of action is broad to accommodate the needs of patients and families, even in mourning8. Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual [1]. Palliative care: provides relief from pain and other distressing symptoms; affirms life and regards dying as a normal process; intends neither to hasten or postpone death; integrates the psychological and spiritual aspects of patient care; offers a support system to help patients live as actively as possible until death; offers a support system to help the family cope during the patients illness and in their own bereavement; uses a team approach to address the needs of patients and their families, including bereavement counselling, if indicated; will enhance quality of life, and may also positively influence the course of illness; is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life, such as chemotherapy or radiation therapy, and includes those investigations needed to better understand and manage distressing clinical complications [1].
The definition and principles of palliative care of the World Health Organization (WHO) establishes that care is also extended to the family environment. Thus, in order for there to be a good relationship with family members, professionals need understand and respect the moment they are going through and the relationship between doctors, patients and family members should develop from a medical behavior compatible with the situation of uncertainty [8,9]. In this sense, empathy on the part of the medical team is imperative, since the sensitivity to conduct this relationship through honest and effective communication is a very important factor in empowering and developing family resilience [9].
One of the necessary conditions of palliative care is the multidisciplinary team, since this assistance requires that several behaviors that depend on other health professionals be adopted. Imperiously palliative care is an interprofessional teamwork [10]. The interprofessional actions allow a real interaction among all members of the team to establish and provide the best possible care for the patient. The palliative care team has an important role, understands better the end-of-life problems and pays attention to the specificities of each patient [11].
The correct indication of the patients to be treated in Palliative Care is essential to avoid the therapeutic obstinacy and the suffering of these patients. One criterion for being eligible for PC is that the patient suffer from at least one of the following diseases or conditions: Alzheimer’s and other types of dementia, cancer, cardiovascular diseases (excluding sudden deaths), cirrhosis of the liver, congenital anomalies, meningitis, immune and hematological disorders, neonatal conditions, Chronic Obstructive Pulmonary Disease (COPD), diabetes, Human Immunodeficiency Virus Infection (HIV/AIDS), renal failure, multiple sclerosis, Parkinson’s disease, rheumatoid arthritis and resistant tuberculosis [12]. These situations are eligible for patients to be accompanied in a Palliative Care service. However, there is still difficulty in establishing these eligibility criteria and also in deciding on these “terminal” diagnoses [13]. The goal should be to avoid therapeutic obstinacy and futile treatments that do not return the health to the patient, or revert your condition and simply provoke more suffering. Unfortunately, patients with life-threatening illness accumulate in hospitals, invariably receiving inadequate care [8]. It is necessary that the doctors know the principles of Palliative Care to elucidate the patient about his situation and direct him to the appropriate care. Palliative Care should be part of the integral health policy and ethically justified by the principles of quality of life and non-maleficence, because the goal of health care cannot only be to heal people, but also to relieve pain and other symptoms, alleviating suffering and not causing further damaging for patients whose life-threatening illness [14].
Clinical Aspects
It is understood as the terminality of life when all possibilities of recovery of the patient’s health conditions are exhausted and the possibility of death seems close and inevitable [15]. Most of the time, it is very difficult to establish when a patient is in the terminal phase of the disease, since many are the symptoms that these patients can present, such as xerostomia, anorexia, dyspnea, behavioral alterations, impairment of mobility and personal care, among others [16]. Of the physical disorders that cause the most disability and reduction in the quality of life is pain, being an unpleasant experience, sensitive and emotional, with variable duration periods, being considered chronic with duration greater than six months [17]. Pain is the symptom most feared by patients who have cancer and many other terminal conditions. Approximately 40% of hospitalized dying patients have moderate-to-severe pain in the final 3 days of life [18].
Pain is something primary, individualized and must be treated properly. Often pain is the starting point for the patient care plan, and perhaps this is why it is a universal concern among the professionals working with these patients. Pain is a problem with great impact on public health, since its prevalence is high, becoming the main complaint in 40% of the primary care services [19]. Thus, as a function of pain, hospitalized patients report a significant worsening of their functionality and greater suffering [20]. Treating pain is one of the most important behaviors, for pain beyond discomfort also causessuffering. Several factors contribute, mainly the ignorance of the pain phenomenon and inadequate treatment. Pain is a form of suffering, however suffering is not restricted to pain.
Therapeutic activities without a healing purpose mitigate suffering and comfort the patient, an example is empathy that establishes a relationship of help, doing something for the other, and also for their families, because they feel comfortable to realize that the loved one is not suffering [21]. Communication is the transmission of information from one person to another. The need for transmission of information received and understood by the professionals of care is necessary for interaction of practitioners, nurses and other professionals involved in the palliative process, reducing the suffering of patients and families [21]. There are care practices that tend either towards therapeutic futility or towards care based on measures that limit the therapeutic effort, with a view to alleviating suffering [22], this should be the chosen alternative.
Quality of Life
The continuity of life involving physical, emotional, social, spiritual and cultural aspects, in order to improve the quality of life, reducing the signs and symptoms of the disease [1,2]. Palliative care provides the patient, whose illness no longer responds to the healing treatment, comfort, pain relief and suffering, as well as improvement in the quality of life in the physical, psychological, social and spiritual aspects, with emphasis on the protection of the family during the process of illness, death and mourning [23]. The Palliative Care generates benefits and improves the quality of life of patients and their families. Palliative care services can reduce the distress caused by symptoms and improve the quality of life of patients near the end of life [18]. However, even if there is progress in research with the intention of establishing prognostic indexes and quality of life, there is still something that can be used universally, this makes this definition more difficult, since it must be private and individualized. Some factors make this expression less imprecise, such as clinical, laboratory, imaging, functional, and even team experience [24]. The recognition that the patient is out of curative therapeutic possibilities does not mean that there is nothing more to be done, that sensitivity of inserting the patient in this thin line is important and will define much about his quality of life [15].
Palliative Care in Brazil
In Brazil, palliative care began in the 1980s, with significant growth in the 2000s, but still much progress has to be made [24], because about 80% of the patients who should be in a palliative care service are treated in hospitals [12]. Moreover, there is a problem in the training of professionals for this kind of care, since in most of the courses the subject is not approached in the graduation. The subject Palliative Care should be worked on in the training of health professionals at the three levels [25].
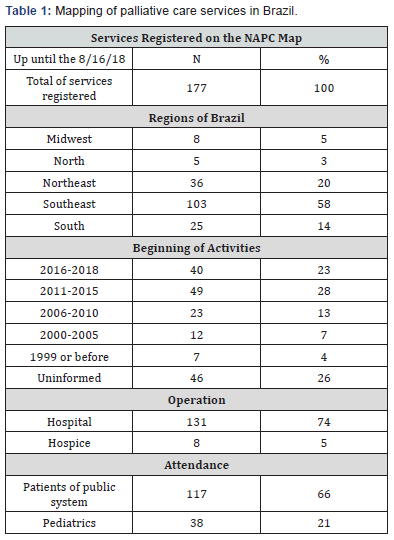
The National Academy of Palliative Care (NAPC) conducted a survey on the palliative care services available in the country in 2018 and through this mapping, it found 177 palliative care services in Brazil by August/2018 [23]. The identified palliative care services, 58% are in the southeast region, and the region with the least number of services was the northern region, with only 3% [23]. The survey carried out by the National Academy of Palliative Care evidenced a great inequality of service availability by regions in the country. This situation shows that there is no State policy for the implementation of palliative care services.
The services that care for cancer patients in Brazil and are accredited in the public health system, Center for High Complexity in Oncology Care (CACON, in Portuguese), must provide assistance in palliative care and respect the principles of this kind of care [26]. Although the provision of palliative care is mandatory for a facility to be accredited as a CACON, there is no regulation for the operation of a hospice. Therefore, in Brazil, most of the palliative care services offered by the public health system are linked to oncology [3] and therefore this situation causes a false impression that palliative care is only for cancer patients.
Another important finding identified by the National Academy of Palliative Care (NAPC) was that 74% of palliative care services operated in hospitals and only 5% operated in hospices [23]. This result is worrying, since centralized care in hospitals demands a higher cost for the public health system, and sometimes does not provide optimal and adequate care for patients. Still according to the Academy mapping, 48% of palliative care services were created between the years 2006 and 2015 and in the period from 2016 to October 2018, 23% of the services were created [23]. These data demonstrate a substantial increase in the availability of palliative care services, probably because oncological centers, when accredited in the health ministry, are obliged to offer palliative care.
An important result refers to the attention in the health system, of the total of palliative care services, 66% attend patients of the public system, that is 117 services [23]. However, this absolute number shows that the needs are not solved, since the supply is small when compared to the demand. Moreover, the patient who is in this situation and is treated in the public health system, requires the attending physician to recognize the case and the correct indication. Another relevant fact is that only 21% of palliative care services attend pediatrics [22]. Besides the availability of palliative care services, another important situation to analyze is the offer of palliative care education in undergraduate courses in the health area in the country. A necessary condition of Palliative Care is to be multidisciplinary, for this, the other courses in the health area should also include Palliative Care in the curriculum [14]. According to NAPC (2018) [23], in Brazil there is no qualification of professionals according to what the demand. Of the 302 undergraduate medical courses in the country, only 42 (14%) offer a palliative care discipline, and only 18 courses (6%) are compulsory subjects [23]. In Europe the situation is quite different because the medical courses in Europe generally have the subject palliative care, because improving quality of life in serious illness is an international priority [27] (Table 1).
There are also in Brazil an increasing number of residences in palliative medicine and palliative care, the latter aimed at nonmedical health professionals, as well as postgraduate courses and specialization in palliative care, however, there is still no regulation a matrix of competencies that guides these courses or residences [23]. In Japan, the Residents learn palliative care during the entire course of illness, and the contents of the course range from training in making accurate pain diagnoses and treating the pain to training in home-based palliative care [28].
The teaching of end-of-life care in Brazil has limitations, requiring extensive discussion, and more efforts should be directed at improving the reality of this important issue in medical education, not only by medical schools, but by health and education agencies in Brazil [29]. The training courses are few and there is still resistance to the debate on the subject, reinforcing the idea that only with a substantial change in knowledge management and in the undergraduate curriculum of health professionals palliative care will have the opportunity to consolidate in Brazil [30]. This situation is alarming, because if there are no professionals qualified to work with Palliative Care, we can conclude that many patients with life-threatening illness are suffering because they do not receive the necessary and adequate attention to their case [14].
Bioethical Approach
Humanization is a complex definition, since it refers to a change of behavior that goes beyond the specific clinical practices and techniques of each health professional, requiring in addition a behavioral change in response to the patient’s demands [3]. In contemporary thought the maxim in human relationships is “do unto another as he would have it done unto him,” no longer use the thought “do unto another as you would have it done unto you.” Each person knows what is best for themselves and what is good for one, may not be good for the other, so respect for autonomy is an essential condition in the doctor-patient relationship. The autonomous individual acts freely according to a plan chosen by himself [31]. The patient with severe and advanced disease, if he has sensory conditions, has the right to decide, to have his autonomy respected, so the patient must be informed about the treatment. The information as a basis of the autonomous decision and it is the responsibility and obligation of the physician to give all the necessary information so that the patient decides autonomously and that he receives the best and adequate attention for his case [14]. And to ensure the principle of autonomy, respect the desire and the will of the patient, it is necessary for the patient to receive all the information about his case, to understand what Palliative Care is and to accept this kind of attention [14]
The quest for immortality is intrinsic to the human being, death in some Western societies is not yet accepted as a natural consequence of life. However, death is inexorable, can not be combated at all costs, acceptance of the finitude of human life is imperative for the moment to occur respecting dignity. The definition of dying with dignity recognizes unconditional intrinsic human values, such as physical comfort, quality of life, autonomy, purpose, preparation, and interpersonal connection [32]. Therefore, the understanding of the health professionals before the process of finitude is fundamental, above all for allowing the recognition of the human being.
Another important bioethical principle is the beneficence that has as its statement: giving the patient what is best for his situation, also ensures that another ethical principle is respected, the principle of beneficence, that is, maximize the benefits [14], however, it is important to remember that what can be good for one patient, for another patient can cause harm and suffering, so a bioethical principle that must be applied correctly is the principle of non-maleficence, whose maxim is not to cause harm
Last but not least, the principle of justice is based on equity and the equitable distribution of goods and services and benefits and fair distribution. The principle of justice that is expressed, in this case, through equity, give each one according to necessity, this principle indicates what should be done for the patient and should be according to the needs of the patient [14].
Conclusion
The characteristics and purposes of palliative care, such as relieving pain, reducing suffering, providing comfort, improving quality of life, and extending family actions are essential and are principles of palliative care. Besides that, it is critical that physicians and other health professionals know how to recognize palliative care clearly, although this is rarely addressed in undergraduate and postgraduate courses in Brazil.
Therefore, in addition to professional experience, maintaining the habit of study and updating, allows the professionals the knowledge necessary to offer the patient the best attention they need. Knowing the principles of palliative care and knowing which patients to indicate them is of fundamental importance, since the doctors who work in the public health system are responsible for the initial referral. When properly indicated it avoids patients being subjected to futile and disproportionate treatments for their case.
It remains to be seen whether physicians refer patients to palliative care services, if they do not, because that happens, probably the reasons is that in Brazil the number of palliative care services is small in relation to demand and most are specialized for cancer patients. However, palliative care is not only indicated for these patients. It is necessary to create new palliative care services in Brazil, that there is disclosure to doctors, other health professionals, patients and family members. It is also necessary to create a State policy so that palliative care can be valued so that the culture of palliative care can be developed and so relieve the suffering of patients and, consequently, improve the quality of life.
References
- World Health Organization (WHO) (2004) Beter palliative care for older people. Geneva (CH), Switzerland.
- Fonseca AC, Mendes-Junior WV, Fonseca MJM (2012) Palliative care of elderly patients in intensive care units: a systematic review. Rev Bras Ter Intensiva 24(2): 197-206.
- Chover-Sierra E, Martínez-Sabater A, Lapeña-Moñux Y (2017) Knowledge in palliative care of nursing professionals at a Spanish hospital. Rev Latino-Am Enfermagem 25: e2847.
- Gómez-Batiste X, Blay C, Roca J, Fontanals MD (2012) Innovaciones conceptuales e iniciativas de mejora en la atención paliativa del siglo XXI. Med Paliat 19(3): 85-86.
- Recomendación Rec (2003) 24 del Comité de Ministros de los estados miembros sobre organización de cuidados paliativos, pp. 5-52.
- Lei 8.080, de 19 de setembro de (1990) Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Diário Oficial da União, Brasília, Brazil.
- Floriani CA, Schramm FR (2010) Casas para os que morrem: a história do desenvolvimento dos hospices modernos. Hist Cienc saude-Manguinhos 17(suppl 1): 165-180.
- Matsumoto DY (2006) Cuidados paliativos: conceitos, fundamentos e princí In: Academia Nacional de Cuidados paliativos. Manual de cuidados paliativos. Rio de Janeiro: Diagraphic, p. 14-19.
- Nunes ECDA, Sousa JO (2017) Limitação do suporte de vida na terapia intensiva: percepção mé Rev Bioét 25(3): 554-562.
- Gomes ALZ, Othero MB (2016) Cuidados paliativos. Estudos Avançados 30(88): 155-166.
- Silveira NR, Nascimento ERP, Rosa LM, Jung W, Martins SR, et al. (2018) Cuidado paliativo e enfermeiros de terapia intensiva: sentimentos queficam. Rev Bras Enferm 69(6): 1074-1081.
- OMS-Organização Mundial da Saúde (2014) How many people at the end of life are in need of palliative care worldwide? In: WPCA- Worldwide Palliative Care Alliance. Global Atlas of Palliative Care at the end of life. WPCA: Londres, UK.
- Paz CRP, Pessalacia JDR, Zoboli ELCP, Souza HL, Granja GF, et al. (2015) Novas demandas para a atenção primária à saúde no Brasil: os cuidados paliativos. Investigación y Educación en Enfermería 34(1): 46-57.
- Laís ZSdA, Carolina ZSdA (2018) Importance of Education in Palliative Care. Palliat Med Care Int J 1(2): 1-2.
- Gutierrez PL (2001) O que éo paciente terminal? Rev Assoc Med Bras 47(2): 92.
- Andrade C (2012) Cuidados paliativos ao Paciente Idoso: uma Revisão Integrativa da Literatura. Revista Brasileira de Ciências da Saúde 16(3): 411-418.
- Peres MFP, Arantes ACLQ, Lessa PS, Caous CA (2007) A importância da integração da espiritualidade e da religiosidade no manejo da dor e dos cuidados paliativos. Rev psiquiatr clín 34(Suppl 1): 82-87.
- Blinderman CD, Billings JA (2015) Comfort Care for Patients Dying in the Hospital. N Engl J Med 373(26): 2549-2561.
- Mäntyselkä P, Kumpusalo E, Ahonen R, Kumpusalo A, Kauhanen J, et al. (2001) Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain 89(2-3): 175-180.
- Dalpai D, Mendes FF, Asmar JAVN, Carvalho PL, Loro FL, et al. (2017) Pain and palliative care: the knowledge of medical students and the graduation gaps. Rev dor 18(4): 307-310.
- Donato SCT, Matuoka JY, Yamashita CC, Salvetti MG (2016) Effects of dignity therapy on terminally ill patients: a systematic review. Rev esc enferm USP 50(6): 1014-1024.
- Silva DS, Evangelista CLS, Santos RD, Paixão GPN, Marinho CLA, et al. (2016) Percepção de enfermeiras intensivistas de hospital regional sobre distanásia, eutanásia e ortotaná Rev Bioét 24(3): 579-589.
- Manual de Cuidados paliativos ANCP (2012) Academia Nacional de Cuidados Paliativos. In: (2nd edn), Manual de cuidados paliativos. Rio de Janeiro: Diagraphic, Brazil.
- Pineli PP, Krasilcic S, Suzuki FA, Maciel MGS (2016) Cuidado Paliativo e Diretrizes Curriculares: Inclusão Necessá Revista Brasileira de Educação Médica 40(4): 540-546.
- Ministério Da Saúde (2005) Portaria nº 741, de 19 de dezembro de 2005, Brazil.
- Kavalieratos D, Corbelli J, Zhang D, Dionne-Odom JN, Ernecoff NC, et al. (2016) Association Between Palliative Care and Patient and Caregiver Outcomes: A Systematic Review and Meta-analysis. JAMA 316(20): 2104-2114.
- Oya H, Matoba M, Murakami S, Ohshiro T, Kishino T, et al. (2013) Mandatory Palliative Care Education for Surgical Residents: Initial Focus on Teaching Pain Management. Jpn J Clin Oncol 43(2):170-175.
- Toledo AP, Priolli DG (2012) Cuidados no fim da vida: o ensino médico no Brasil. Rev bras educ med, Rio de Janeiro 36(1): 109-117.
- Fonseca A, Geovanini F (2013) Cuidados paliativos na formação do profissional da área de saú Rev bras educ med Rio de Janeiro 37(1): 120-125.
- Beauchamp TL, Childress JF (2002) Princípios de Ética Biomé São Paulo: Loyola, Brazil.
- Coelho CBT, Yankaskas JR (2017) Novos conceitos em cuidados paliativos na unidade de terapia intensiva. Rev bras ter intensiva 29(2): 222-230.
- Queiroz TA, Ribeiro ACM, Guedes MVC, Coutinho DTR, Galiza FT, et al. (2018) Cuidados paliativos ao idoso na terapia intensiva: olhar da equipe de enfermagem. Texto & Contexto - Enfermagem 27(1): e1420016.






























