Abstract
Sleep disorders are a fairly common problem in patients with autism spectrum disorder (ASD). From a sample of 51 patients, aged 4 to 13 years, diagnosed with Autism Spectrum Disorder (ASD), 14 patients with comorbid sleep disorders were selected. These patients undergo therapy according to the principles of ABA- VB (Applied Behavioral Analysis and Verbal Behavior). During the neuropsychiatric examination and therapy sessions, specific instructions were given, which were implemented by the families with the support of the rehabilitation team. Families were also asked to complete sleep diaries to monitor the irregularity of the sleep- wake rhythm. The evolution of the sleep disorder was analyzed over one year (January 2023-January 2024); the results showed that 6 patients improved and 8 showed no improvement. Of these 8, 7 had sensory atypia and greater clinical severity. This study demonstrates the correlation between sensory atypia, clinical severity, and sleep disturbances in ASD and the effects of behavioral therapy on the disorder.
Keywords:Sleep Disorders; Neurodevelopmental Disorders; Parasomnias; Sleep Anxiety
Introduction
Sleep disorders are one of the most common comorbidities in children with autism spectrum disorder (ASD). A wide variety of sleep problems have been reported in children with ASD, with a prevalence ranging from 60% to 86% according to some studies, while other authors estimate the prevalence to be 40-80%, while in neurotypical children the prevalence is 25-50%. Autistic children are indeed more likely to have sleep difficulties than children with other neurodevelopmental disorders and typically developing [1-4].
It should also be emphasized that the reported prevalence of sleep disturbances in patients with ASD is likely underestimated due to a combination of factors, including the use of self-reporting or parental reporting and the use of different definitions of sleep disturbance (Dondur Balli et al). Studies using home actigraphs or laboratory-based polysomnography have mostly validated parent reports [5] and showed that children with ASD sleep, on average, 30-40 minutes less per night than typically developing children [6]. The etiology of sleep disorders in children with ASD is multifactorial, related to complex interactions between biological fac tors and psychological, socio-environmental, and family factors. Sleep irregularity in these children has been shown to worsen autism symptoms, and shorter sleep duration predicts greater impairment in social communication, hypersensitivity to the environment, higher rates of stereotyped behaviors, and dysfunctional routines [7,8].
Poor sleep can therefore have harmful effects on cognitive and adaptive functions, favoring the onset of aggression, irritability, inattention and hyperactivity in children with ASD. However, while some researchers have linked the severity of sleep disturbances with the severity of the main symptoms of ASD [9] others do not confirm this correlation [10,11]. These inconsistent findings suggest that sleep disturbances occur in many cases regardless of the severity, adaptive level, or cognitive abilities of the child with ASD..
Treatment of these conditions should therefore be a primary therapeutic goal, given their significant impact on the quality of life of patients and their families. The sleep characteristics most frequently described in the literature include above all: difficulty falling asleep, restless sleep, frequent night-time awakenings, early morning awakenings, low sleep efficiency [3], short-term and daytime insomnia. Nightmares, morning headaches, crying during sleep, sleep apnea, and sleepwalking are equally common.
Although sleep problems can be significant at all ages, problems with sleep duration (shorter) are more prevalent in adolescence compared to young children who tend to present more frequently resistance to bedtime, sleep anxiety, parasomnias and night awakenings [12, 13]. Some studies of adolescents have also reported that those with high-functioning autism were three times more likely to have sleep problems than their typically developing peers [14-15] investigated the importance of synaptic dysfunction in animal models : given the functions of sleep in promoting brain connectivity, neural plasticity, emotional regulation, and social behavior , all of critical importance in the pathogenesis of ASD, these authors hypothesize that synaptic dysfunction is an important mechanism linking ASD and SD.
Parental stress is usually relevant: in a Berloco sample Guerrera [16] found that one-third of children suffered from insomnia, which was associated with reduced adaptive behaviors and higher levels of parental stress, as well as behavioral and emotional problems. Therefore, appropriate interventions need to be developed to potentially alleviate the severity of clinical correlates and parental burden. Increased use of emergency services and emergency services is also reported [17]: children with ASD, with sleep disorders, were 1.72 and 2.71 times more likely to visit the emergency room and be admitted to hospital than their counterparts without this comorbidity. As reported by Verhoeff and colleagues in 2018, the association between sleep disturbances and autism spectrum disorder can be explained in two ways: sleep problems may precede and worsen behavioral outcomes in children with ASD or, conversely, they may be a consequence of autism spectrum disorder.
In this regard, the same authors compared children without ASD and children with ASD, highlighting that the two groups had similar sleep duration during early childhood, while starting at 30 months, the ASD group showed a reduction in sleep duration compared to the group of typically developing children. Regarding adolescence, a study cited by the same authors reported a higher prevalence of sleep-related problems in girls and boys with ASD compared to the typically developing population. Furthermore, as reported by Malhi and colleagues [18], research shows that greater and more persistent sleep difficulties in children with ASD compromise their social, emotional, and cognitive functioning, increase negative outcomes, and reduce the quality of life of the children themselves and their families. Sleep deprivation could, therefore, worsen these children’s difficulties, increasing cognitive dysfunction and exacerbating behavioral symptoms present throughout the day.
Several authors have reported the correlation between sleep disturbances and sensory abnormalities [19]. Although it is often assumed that abnormalities in all sensory domains are similarly associated with sleep problems, some studies suggest that tactile hypersensitivity in particular may play a significant and specific role. It is therefore hypothesized that hypersensitivity to touch interferes with sleep initiation and maintenance in many cases of ASD associated with severe sleep disturbances [10]. Other studies have also shown the association between irritability, sensory atypia, and sleep disturbances, indicating that sleep disturbances were significantly associated with irritability only in children with moderate to severe sensory sensitivity [20].
Various authors Mahli et al. [18] demonstrated that the severity of sleep disturbances was significantly related to the severity of maladaptive behaviors during the daytime routine, including both externalizing and internalizing problems. Further support for this thesis can also be found in the work of Mazurek & Sohl [21] in which the authors identified a strong correlation between sleep disturbances and daytime functioning; in particular, they found that physical aggression, hostility, inattention and hyperactivity were correlated with sleep duration, night-time awakenings and parasomnias. Furthermore, sleep-related anxiety was positively correlated with both irritability and hyperactivity while daytime sleepiness was only related to irritability.
Materials and Methods
We selected a sample of 51 patients, 40 m and 11 f, all diagnosed with ASD and all treated according to the principles of ABA - VB (Applied Behavioral Analysis and Verbal Behavior). There are 12 patients who have comorbid sleep disorders and showed sensory atypia. The children in the study group met the following inclusion criteria: (a) age range 4 to 13 years, (b) diagnosis of ASD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM, APA 2022) criteria, and (c) criteria for ASD in Autism Diagnostic Observation Schedule - Second Edition (ADOS-2, Lord [21].
Patients with known genetic or chromosomal abnormalities, neuromotor disorders, significant sensory impairment (such as profound bilateral sensorineural hearing loss and profound bilateral visual impairment), or a diagnosis of epilepsy were excluded from the study, as these conditions could independently impact sleep quality. Children with other diagnoses of neurodevelopmental disorders or those receiving antiepileptic or antihistamine medication were also excluded.
A group of 50 neurotypical, regularly educated individuals, aged 4-14 years, 301 males and 19 females, was used as a control group. Of these, 9 (17.6%) presented sleep disorders. Of our sample with ASD, 14 subjects (27.45%), 12 males and 2 females, had sleep disorders. Of these, 3 were taking melatonin-based drug therapy. One patient was being treated with risperidone. Recommendations on sleep hygiene for children have recently been organized into a mnemonic tool – “ABCs of SLEEPING,” whose characteristics are summarized in a series of behavioral interventions. These include specific strategies, based on learning and behavioral principles, aimed at developing sleep-promoting habits, as well as the ability to relax and manage anxiety.
On the basis of these studies, during the neuropsychiatric visit
and subsequent checks, the following indications were provided
to parents for the management of sleep disorders:
i. Structure daily routines in which the child goes to sleep
almost always at the same time, after at least an hour and without
having had a too large meal,
ii. Create goodnight rituals that guide your child to sleep
time,
iii. Avoid putting children to bed well before bedtime, as
this reduces their ability to fall asleep,
iv. Gradually delay bedtime to “reset” the circadian rhythm
and improve morning awakenings, sleep latency and night awakenings,
v. co-sleeping habits. Parents should gradually increase
their distance from their children until they can fall asleep. It is
therefore necessary to teach children to fall asleep in their own
room, under the care of their parents, and then let them sleep
alone.
vi. Don’t give prominence to the child’s behaviors that contribute
to altering sleep,
vii. Provide positive reinforcement in the morning, after
waking up,
viii. Implement these strategies consistently, even though
they are often challenging and burdensome, with the help of experienced
operators.
The rehabilitation team, through parent training and specific therapy sessions, helped families implement these principles into home-based behavioral treatment. Patients’ parents completed a sleep diary, recording their bedtime and wake-up times, sleep duration, any nighttime awakenings, daytime sleepiness, and other sleep- related details.
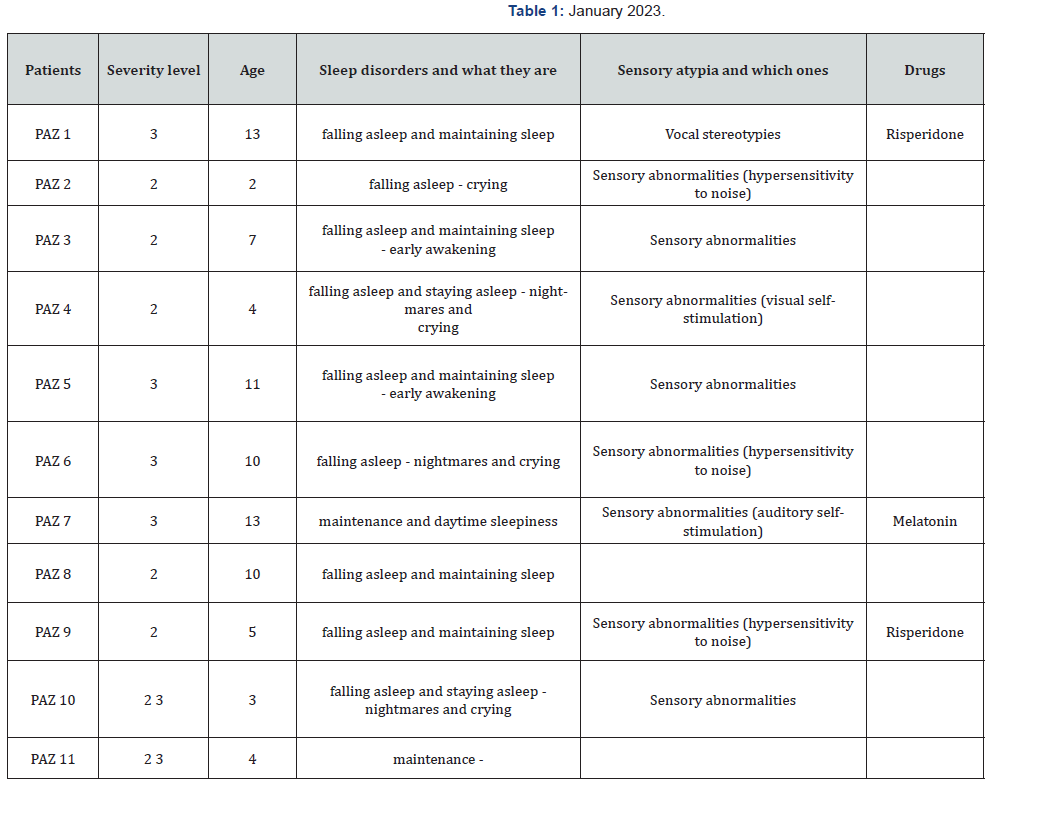
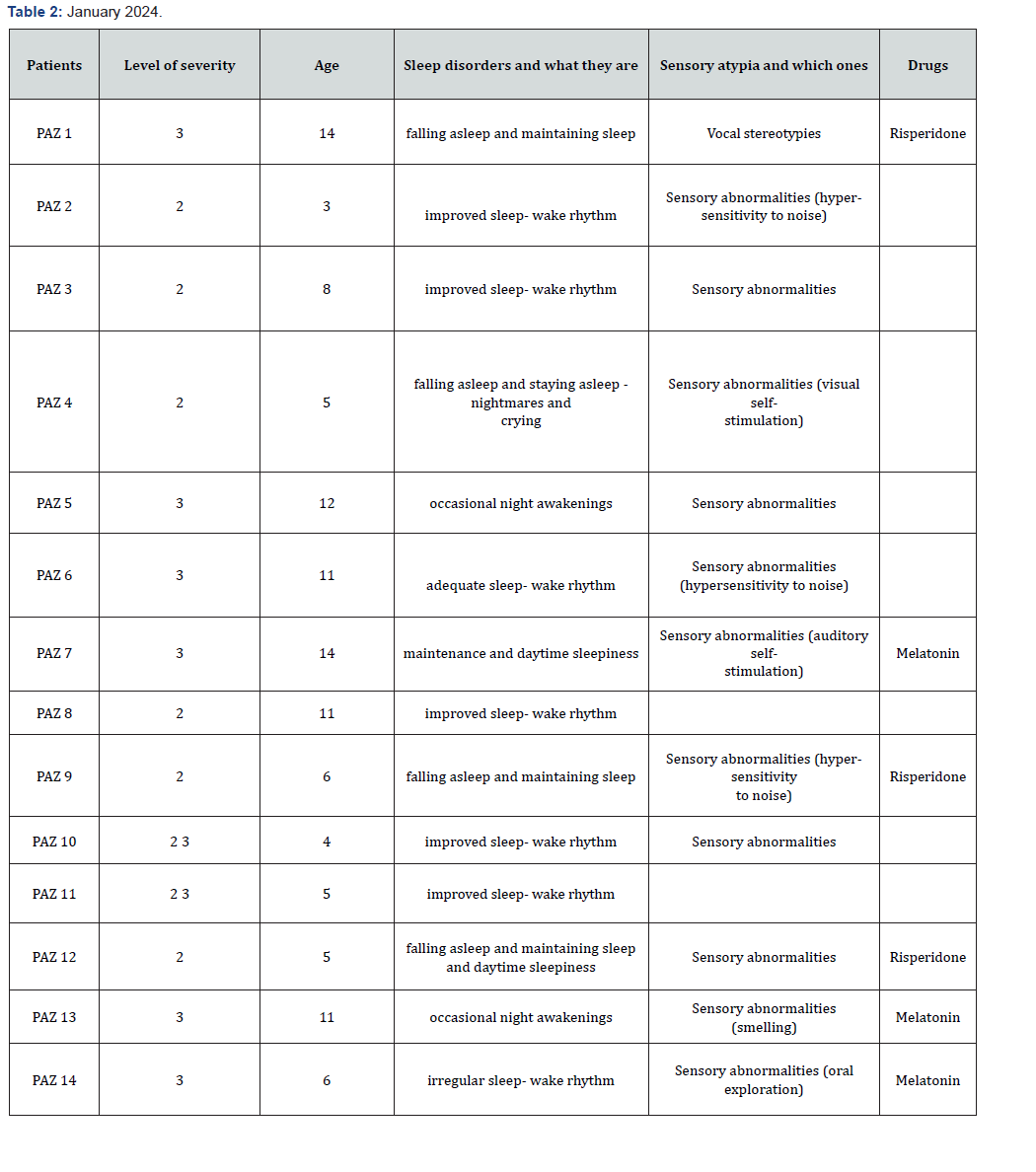
The following tables (Tables 1 & Table 2) show the analysis of the ABA forms, which are completed during periodic neuropsychiatric visits to renew treatment plans. Specifically, the data reported in January 2023 are compared with those reported in January 2024.
Results
After one year of treatment with behavioral therapy (ABA-VB), improved sleep was observed in 6 of 14 patients. Of the patients who had not improved, 7 of 8 still had sensory atypia and exhibited more severe clinical features. Among the patients treated with melatonin, only one reported clinically significant improvements, demonstrating that the therapies should be combined. In the control group, 9 children (17.6%) had sleep disorders. Of these, after 1 year, 2 children had improved, thanks to family interventions without any therapeutic support, and 7 children had not improved.
Discussion
Applied Behavior Analysis (ABA) therapy includes sessions delivered at home, at school, and in community settings, as well as supervision and parent training. Several meta-analyses demonstrate that ABA improves various outcome measures, including socialization, communication, and expressive language, in patients with ASD [22,23]. In our sample, patients received between 32 and 60 hours of behavioral treatment per month, including supervision and parent training. In cases with comorbid sleep disorders, in our sample, specific therapeutic sessions were dedicated, both to children and family members, relating to the time of falling asleep and to all sleep-related behaviors, especially using fading, extinction and positive reinforcement.
Of these, 6 patients showed improvements, associated with a general improvement in behavior. After one year of therapy, 8 patients showed no significant improvement. The correlates of the lack of improvement are due to the families’ partial adherence to behavioral treatment, the severity of the condition, and the presence of sensory atypia in 7 out of 8 patients. However, in our sample, the percentage of patients with sleep problems is below the data found in the literature, rather approaching the percentage of the neurotypical population, as in the control group (27.4 vs. 17.6%).
It is therefore important to consider the extent to which this type of problem impacts family life. Intervening on sleep disorders in children with ASD could reduce the occurrence of challenging behaviors and therefore also impact parental stress levels and family well-being. As underlined by the authors Mahli et al. [18], Mazurek & Sohl, et al. [21], it is important that children with ASD are screened for these difficulties and that the most appropriate interventions are subsequently activated, such as psycho-education on sleep hygiene, cognitive- behavioral treatment and pharmacological treatment.
Guidelines for the treatment of sleep disorders in children and adolescents with ASD, published by the American Academy of of Neurology, Buckley et al. [23] recommend, as a first approach, parental consultation to impart knowledge regarding behavioral techniques and sleep hygiene, as confirmed by several authors Kirkpatrock [24]. A 2017 meta-synthesis of previously published systematic reviews showed that sleep education programs have marked positive effects – particularly on nighttime awakenings – and moderate or weak positive effects on all other sleep domains. However, it should be taken into account that different possible ways of providing sleep education can influence its outcome.
As regards sleep psychoeducation, we recall the document produced by the Autism Treatment Network (ATN) entitled “Strategies to Improve Sleep in Children with Autism Spectrum Disorders”. Literature shows that behavioral treatment guarantees favorable effects, especially in younger patients, but in recent years several studies have been conducted regarding the effectiveness of the aforementioned therapy also in older children and adolescents [25].
In the study by McCrae [26] and colleagues which included 17 children aged 6 to 12 years, the intervention consisted of eight 50-minute sessions of CBT-CI, administered one week apart, supplemented by one hour per week of group or individual supervision. Results showed significant improvements in sleep and daytime functioning in both children and their parents. After 12 weeks of treatment and during the 25-26 week follow- up, moderate improvements were observed in the child’s subjective perception and objective sleep, sleep/wake regulation, and daytime behavior, including sleepiness, irritability, and stereotypy.
In parents, however, there was an immediate improvement in subjective perception of sleep, objective sleep, and inappropriate fatigue. In a 2016 study by Loring [27], 23 adolescents aged 11 to 18 and their parents were treated with two individual sleep education sessions, one week apart, based on relaxation techniques. This was complemented by homework and behavioral notes by the family, and two follow-up telephone calls, one and two weeks apart. Significant improvements in sleep stability, as well as cognitive and behavioral changes, were achieved. However, mean insomnia latency did not change, so perhaps behavioral techniques are not enough for adolescents.
Lunia and Smith observed the correlation between sleep and well-being in young adult students diagnosed with autism spectrum disorders. Various factors, such as gender, age, culture, and internet and smartphone use, appear to impact the relationship between autistic traits, sleep quality, and well-being in college students. Treatment options range from lifestyle modifications and behavioral interventions to drug therapies.
They require a combination of 1) parental psychoeducation to better understand sleep disturbances; 2) implementation of bedtime rituals appropriate to the child’s age and unique characteristics; 3) specific behavioral strategies, including extinction and positive reinforcement of adaptive behaviors. From a pharmacological point of view, melatonin, both rapid and slow release, plays an important role in the therapeutic efficacy Gringras P [28], Sadeh et al. [29]. Sleep problems in children with ASD should therefore always be addressed gradually, with increasing intensity on a case-by-case basis when lower-level strategies appear ineffective.
As a general principle in developmental age, non-pharmacological intervention is the first treatment option before starting any drug therapies. One type of behavioral intervention is Bedtime Fading with Response Cost (BFRC) [30] uses parents as agents of change by implementing treatment in the home environment. Results indicate that the BFRC was effective in eliminating unwanted co-sleeping, frequent nighttime awakenings, and dependent sleep onset. Secondary improvements include reduced sleep onset latency, bedtime resistance, and disruptive sleep-related behaviors.
Physical activity (PA) intervention [31-37] is also a promising behavioral intervention that has received increasing attention, but its effects on sleep are still unclear. However, compared with no-treatment control groups, PA interventions had positive effects on parent-reported general sleep problems, nighttime awakenings, sleep resistance, sleep duration, and sleep quality.
Conclusion
i. Our contribution demonstrates the importance of sleep disturbances in the clinical picture of children with ASD, and the importance of identifying and treating this issue, especially with behavioral techniques. A notable finding in our sample is that sleep disturbances were present in a percentage very close to that of neurotypical subjects, represented by the control group. This experience nonetheless confirms the correlation between sleep disturbances, sensory atypia, and the clinical severity of the disorder, albeit in a rather small sample. The study still has room for improvement and requires a larger sample size, although it offers interesting insights into ASD and the behavioral treatment of sleep disorders.
References
- Souders MC, Mason TB, Valladares O, Bucan M, Levy SE, Mandell DS, et al. (2009) Sleep behaviors and sleep quality in children with autism spectrum disorders. Sleep 32(12):1566–1578.
- Souders MC, Zavodny S, Eriksen W, Sinko R, Connell J, et al. (2017) Sleep in Children with Autism Spectrum Disorder. Curr Psychiatry Rep 19(6): 34.
- Hodge DCarollo TM, Lewin M, Hoffman CD (2014) Sweeney DP. Sleep patterns in children with and without autism spectrum disorders: developmental comparisons. Res Dev Disabil 35(7): 1631–1638.
- Johnson KP, Zarrinnegar P (2024) Autism Spectrum Disorder and Sleep. Psychiatr Clin North Am 47(1): 199-212.
- Yavuz Kodat E, Reynaud E, Geoffray MM, Limousin N, Franco P, et al. (2020) Disturbances of Continuous Sleep and Circadian Rhythms Account for Behavioral Difficulties in Children with Autism Spectrum Disorder’s Clin Med 9(6): 1978.
- Van der Heijden KB, Stoffelsen RJ, Popma A, Swaab H (2018) Sleep, chronotype, and sleep hygiene in children with attention-deficit / hyperactivity disorder, autism spectrum disorder, and controls. Eur Child Adolescent Psychiatry 27(1):99-111.
- Carmassi C, Palagini L, Caruso D, Masci I, Nobili L, et al. (2019) Systematic Review of Sleep Disturbances and Circadian Sleep Desynchronization in Autism Spectrum Disorder: Toward an Integrative Model of a Self-Reinforcing Loop. Front Psychiatry 10: 366.
- Favarin S (2023) Sleep, Insomnia, and Autism. Some Remedies for Sleep Disorders. Asperger's Online.
- Veatch, OJ, Maxwell Horn AC and Malow BA (2015) sleep in autism spectrum disorders. Curr Sleep Medicine Rep 1: 131–140.
- Tzischinsky O, Meiri G, Manelis L, Bar Sinai A, Flusser H, et al. (2018) Sleep disturbances are associated with specific sensory sensitivities in children with autism. Mol Autism 9: 22.
- Wiggins LD, Tian LH, Rubenstein E, Schieve L, Daniels J, (2022) Features that best define the heterogeneity and homogeneity of autism in preschool children: a multicenter case control analysis replicated on two independent samples. Autism Research 15 (3): 539-550.
- Richdale AL, Prior MR (1995) Sleep/wake patterns in children with autism. Eur Child Adolescent Psychiatry 4(3): 175-186.
- Fletcher FE, Foster Owens MD, Conduit R, Rinehart NJ, Riby DM, et al. (2017) The developmental trajectory of parent-reported and objective sleep profiles in autism spectrum disorder: Associations with anxiety and bedtime routine. Autism 21(4): 493-503.
- Baker E, Richdale A, Short M, Gradisar M (2013) An investigation of sleep patterns in adolescents with high- functioning autism spectrum disorder compared with typically developing adolescents. Dev Neurorehabil 16(3):155-165.
- Doldur Balli F, Imamura T, Veatch OJ, Gong NN, Lim DC, et al. (2022) Synaptic dysfunction connects autism spectrum disorder and sleep disturbances: A perspective from studies in model organisms. Sleep Med Rev 62: 101595.
- Berloco B, Guerrera S, Fucà E, Menghini D, Valeri G, et al. (2023) Insomnia in children with autism spectrum disorder: a cross-sectional study of clinical correlates and parenting stress. Journal of Autism and Developmental Disorders 53(4):1733.
- Solomon S, Elbedour L, Meiri G, Michaelovski A, Sadaka Y, et al. (2024) Sleep disturbances are associated with greater healthcare utilization in children with autism spectrum disorder. J Neurodev Disord 16(1): 29.
- Malhi P, Kaur A, Singhi P, et al. (2019) Sleep Dysfunction and Behavioral Daytime Problems in Children with Autism Spectrum Disorders: A Comparative Study. Indian J Pediatrician 86: 12–17.
- Lane SJ, Leão MA, Spielmann V (2022) Sleep, Sensory Integration /Processing, and Autism: A Scoping Review. Front Psychol 13: 877527.
- Molcho Haimovich A, Tikotzky L, Meiri G, Ilan M, Michaelovski A, et al. (2023) Sleep disturbances are associated with irritability in ASD children with sensory sensitivities. J Neurodev Disord 15(1): 21.
- Mazurek MO, Sohl K (2016) Sleep and behaviour problems in children with autism spectrum disorder. J Autism Dev Disord 46(6):1906-1915.
- Lord G, Rutter M, DiLavore PC, Risi S Luyster RJ, Gotham K, et al. (2013) ADOS-2-Autism Diagnostic Observation Schedule-Second Edition.
- Buckley WA, Hirtz D, Oskoui M, Armstrong MJ, Batra A, et al. (2020) Practice guideline: Treatment for insomnia and disrupted sleep behavior in children and adolescents with autism spectrum disorder: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 94(9): 392-404.
- Kirkpatrick B, Louw JS (2019) Leader G Efficacy of parent training incorporated in behavioral sleep interventions for children with autism spectrum disorder and/or intellectual disabilities: a systematic review. Sleep Med 53: 141-152.
- Pattison E, Papadopoulos N, Marks D, McGillivray J, Rinehart N (2020) Behavioral Treatments for Sleep Problems in Children with Autism Spectrum Disorder: a Review of the Recent Literature. Curr Psychiatry Rep 22(9): 46.
- McCrae CS, Chan WS, Curtis AF, Nair N, Deroche CB, et al. (2020) Cognitive behavioral telehealth therapy for insomnia in children with autism spectrum disorder: A pilot examining feasibility, satisfaction, and preliminary findings. Autism 25(3): 667-680
- Loring WA, Johnston R, Gray L, Goldman S, Malow B (2016) A Brief Behavioral Intervention for Insomnia in Adolescents with Autism Spectrum Disorders. Clinical Practice in Pediatric Psychology 4(2): 112-124.
- Gringras P, Nir T, Breddy J, Frydman Marom A, Findling RL (2017) Efficacy and Safety of Pediatric Prolonged-Release Melatonin for Insomnia in Children with Autism Spectrum Disorder. J Am Acad Child Adolescent Psychiatry 56(11): 948-957.
- Sadeh H, Meiri G, Zigdon D, Ilan M, Faroy M, et al. (2023) Adherence to treatment and parents ' perspective about effectiveness of melatonin in children with autism spectrum disorder and sleep disturbances. Child Adolescent Psychiatry Mind Health 17(1): 123.
- Gitimoghaddam M, Chichkine N, McArthur L, Sangha SS, Symington V (2022) Applied Behavior Analysis in Children and Youth with Autism Spectrum Disorders: A Scoping Review. Perspect Behav Sci 45(3): 521-557.
- Yu Q, Li E, Li L, Liang W (2020) Efficacy of Interventions Based on Applied Behavior Analysis for Autism Spectrum Disorder: A Meta-Analysis. Psychiatry Investigation 17(5): 432-443.
- Lunia D, Smith AP (2024) Exploring the Associations between Autistic Traits, Sleep Quality and Well-Being in University Students: A Narrative Review. Healthcare (Basel) 12(20): 2027.
- Sanberg SA, Kuhn BR, Kennedy AE (2018) Outcomes of a Behavioral Intervention for Sleep Disturbances in Children with Autism Spectrum Disorder. J Autism Dev Disord 48(12): 4250-4277.
- Liang X, Haegele JA, Tse AC, Li M, Zhang H, et al. (2024) The impact of physical activity intervention on sleep in children and adolescents with autism spectrum disorder: A systematic review and meta-analysis. Sleep Med Rev 74: 101913.
- American Psychiatric Association DSM 5-TR 2022.
- Autism treatment network (2005) Strategies to Improve Sleep in Children with Autism Spectrum Disorders.
- Verhoeff ME, Blanken LME, Kocevska D, Mileva Seitz VR, Jaddoe VWV, et al. (2018) The bidirectional association between sleep problems and autism spectrum disorder: a population-based cohort study. Mol Autism 9:8.






























