Recovery From Post-Earthquake Psychopathology Among Survivors of the 1988 Armenian Earthquake 23 Years After the Event
Vahe Khachadouriana,b*, Haroutune K Armenianc, Armen Goenjiand,e, Anahit Demirchyana and Varduhi Petrosyana
aTurpanjian College of Health Sciences, The American University of Armenia, Yerevan, Armenia
bDepartment of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, NY, United States
cDepartment of Epidemiology, Fielding School of Public Health, UCLA, Los Angeles, CA, United States
dDepartment of Psychiatry and Biobehavioral Sciences, Geffen School of Medicine at UCLA, Los Angeles, CA, United States
eCenExel- CNS Clinical Research, Garden Grove, CA, United States
Submission: August 25, 2022; Published: September 06, 2022
*Corresponding author: Vahe Khachadourian, Turpanjian College of Health Sciences, The American University of Armenia, Yerevan, Armenia and Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, NY, United States
How to cite this article: Khachadourian, V, Armenian HK, Goenjian A, Anahit D, Varduhi P. Recovery From Post-Earthquake Psychopathology Among Survivors of the 1988 Armenian Earthquake 23 Years After the Event. Psychol Behav Sci Int J. 2022; 19(2): 556010. DOI: 10.19080/PBSIJ.2022.19.556010.
Abstract
Background: A significant proportion of disaster survivors develop mental disorders. However, studies evaluating determinants for long-term recovery from psychopathology are scarce. This study identifies factors associated with recovery from post-disaster psychopathologies among 1988 Armenian earthquake survivors.
Methods: This is part of a longitudinal epidemiologic study among survivors of the 1988 Spitak earthquake. A nested cohort of 544 subjects was assessed in 1991 and 2012. Subjects had one-or-more baseline psychopathologies, including depression, PTSD and anxiety disorder. Based on our 2012 psychological assessment, individuals formed two groups: those who recovered from all psychopathologies and those who did not. The associations of socio-demographic characteristics and earthquake-related and life-time experiences with recovery from psychopathologies were explored using multivariable logistic regression.
Results: About 60% of individuals with one-or-more psychopathologies in 1991 were free of psychopathology in 2012. After controlling for confounders, we found access to healthcare services (OR=1.80, CI: 1.21-2.68) and perceived average/high socioeconomic status during the 10 years following the earthquake (OR=1.64, CI: 1.12-2.39) were positively associated with recovery. Each additional negative stressful life event decreased the likelihood of recovery from psychopathologies (OR=0.88, CI: 0.80-0.97). Those with severe financial/material losses had 61% lower odds of recovery (OR=0.39, CI: 0.19-0.78). Among those with severe losses, post-earthquake financial/material support contributed to recovery (OR=5.57, CI: 2.01-14.85).
Discussion: Earthquake-related losses have long-lasting negative impacts on the mental health of survivors. Post-disaster adversities and harsh living conditions aggravate the sequel of psychopathology among victims. Timely financial/material support and access to healthcare services helps recovery, particularly for those experiencing severe losses.
Keywords: Psychopathology; Earthquake; Mental health; Post-traumatic stress disorder; Trauma
Abbreviations: PTSD: Post-Traumatic Stress Disorder; DIS: Diagnostic Interview Schedule; PCL-C: PTSD Checklist for Civilians; SCL-90-R: Symptom Checklist-90-Revised
Introduction
Natural disasters such as earthquakes are unexpected and unpredictable events affecting lives of millions annually. There is a large body of evidence showing that catastrophic earthquakes are associated with adverse health outcomes [1-4]. Armenian et al. [1] found that disaster survivors have higher rates of myocardial infarction, migraine, and arthritis. In the aftermath of disasters, a large proportion of survivors also suffer from psychopathology including post-traumatic stress disorder (PTSD), depression, and anxiety [3,5-8]. For instance, Norris et al. [9] in a study of flood survivors in Mexico, six months after the event, found the prevalence of PTSD was 24%. In another study, six months after the Newcastle earthquake, Carr et al. [5] showed that among survivors who had experienced a threat and disruption, the PTSD rates were about 40%. Following PTSD, depression and anxiety are the second and third common disorders studied among disaster survivors [10]. Research has shown that these three disorders are highly comorbid [11-13].
During the last decades, a growing number of studies have investigated the concept of resilience with an operational definition of the ability to maintain functionality despite high levels of distress [14,15]. Among the majority of people with PTSD, symptoms resolve within months to few years [10,16,17]. However, in a minority the disorder may become disabling for a long period, even decades following the traumatic event [18- 21]. In a prospective study of psychopathology after the Spitak earthquake, subjects exposed to severe trauma and multiple post disaster adversities did not show improvement in their PTSD symptoms from 1.5 to 4.5 years after the earthquake [22]. Variations in severity of the disorder depend on multiple factors including victim’s sex, age, ethnicity, pre- and post- disaster adversities, and traumas, most importantly, the severity of trauma [10,16,23].
Kessler and colleagues [13] showed that one-third of survivors diagnosed with PTSD remained symptomatic even a decade after the event. Bland et al. [24] suggested that the psychological sequel of earthquakes among survivors can last for over a decade. Lazaratou et al. [25] showed that the effect of a catastrophic earthquake on psychological reactions can be substantial even half-a-century after the event. In a review article on PTSD following disasters, Neira et al. [26] noted that the course of PTSD after disaster remains unclear and that no study to date has assessed adequately the course of PTSD over a long enough period of time. High rates and persistence of psychopathologies for long periods after catastrophic disasters underscore the importance of evaluating long-term risk and protective factors. A better understanding of such factors would help mental health professionals and public health policy makers to better organize post-disaster interventions.
On December 7, 1988, an earthquake with a magnitude of 6.9 on the Richter scale struck northern Armenia, resulting in over 25,000 deaths and 100,000 injured and left half-a-million people without a shelter. Post-disaster studies in this population have reported high rates of PTSD and depression among the survivors, years after the disaster [3,4,6,27]. Studies in this population have found genetic factors, gender, lower education, severe financial loss, closer location to the epicenter, post-earthquake adversities and exposure to trauma and lack of social support to be associated with mental health conditions including depression and PTSD [3,4,6,27-29]. The objective of this study among adults exposed to the 1988 Spitak earthquake was to evaluate the association of socio-demographic variables, pre- and post-earthquake experiences, and health related factors with the recovery from psychopathology over two decades later.
Methods
A geographically stratified sub-sample of 725 individuals from a more extensive four-phase post-earthquake epidemiological study of a survivor cohort was followed from 1990-2012. The original cohort, consisting of more than 32,000 individuals, included Ministry of Health employees and their families who resided in the earthquake- damaged zone at the time of the earthquake. Further details on this are provided elsewhere [4]. To identify the factors associated with recovery from psychopathology during the study period of 1991 to 2012, a nested cohort of 544 participants who had reported at least one psychopathology (depression, PTSD, or anxiety disorder) in 1991, out of the total of 725, was selected for the analysis.
Baseline data from the initial phase of the study conducted between 1990 and 1992 included age, gender, education, and dichotomized measures of health behavior including smoking, drinking, and physical exercise. Earthquake-related exposure data included distance from the epicenter (location of residency), serious injuries, death among nuclear family members, and selfreported earthquake- related financial loss divided into none to moderate, and severe loss. Post-earthquake factors included change in employment status after the earthquake and financial/ material aid received. Follow-up data used in the current study were collected in 2012 and included major negative stressful events over the lifetime period, financial status over the 10 years following the earthquake, and access to healthcare services when needed.
Additionally, the life time event checklist collected data on divorce, serious personal illness, serious injury/illness of a nuclear family member, separation from a nuclear family member, detention, violence, and life threatening accidents.
The financial status of participants over the 10 years following the earthquake was measured by a self-reported question with a 5-option ordinal scale, the responses to which were dichotomized by combining very good, good, and average responses vs. poor, and very poor. Psychological assessments conducted in 1991 and 2012 included measurement of PTSD, clinical depression and generalized anxiety. The assessments in 1991 were conducted using scales based on the DSM-III-R criteria, which were current at the time of the assessment. The items in the scales were adopted from Diagnostic Interview Schedule (DIS) [30], an easyto- administer instrument with high inter-rater agreement [31] and high validity, correlating with other measures of PTSD and depression [32,33]. The Armenian translation of the instrument was pretested and its diagnostic accuracy was checked against a trained psychiatrist’s diagnosis, demonstrating high sensitivity (1.00) and specificity (0.80). More details on the development and structure of the phase II psychological instruments are provided elsewhere [3,4].
In 2012, we utilized the widely used PTSD Checklist for Civilians (PCL-C) to measure severity of symptoms [34]. The Armenian translation of the PCL-C has shown a very good diagnostic accuracy. At a cut off score of 51, it showed a sensitivity of 0.85 and specificity of 0.82 [35]. Major depression was assessed using the modified validated Armenian version of CES-D [36], at a cut-off of 17 it demonstrated a sensitivity of 0.89 and a specificity of 0.76 [36,37]. The anxiety subscale of the Symptom Checklist-90-Revised (SCL-90-R) was used to screen for general anxiety disorder [38]. The SCL-90-R is a highly valid and reliable instrument commonly used to measure psychopathologies in epidemiologic studies. It has a 5-point severity rating scale ranging from 0 (Not at all) to 4 (extremely) [38]. The Armenian translation of this instrument has been used before in the same target population [39]. We used a cut off score of 11 to diagnose general anxiety disorder.
Analysis
The nested cohort was divided into two groups based on their psychopathological status in 2012. We considered those with at least one psychopathology (PTSD, depression or anxiety disorder) in 2012 as not recovered and those with no discernible psychopathology as recovered. Recovery status in 2012 was the outcome variable in the analysis. We used chi-square and t-test statistics to compare the measured variables between the recovered and not recovered groups for socio-demographic and other variables of interest. multivariable logistic regression analysis was used to evaluate the associations between the outcome psychopathology status and the independent variables after controlling for potential covariates.
Results
Table 1 shows the cross-tabulated percentages of individuals with any psychopathology in 1991 and 0 to 3 psychopathologies in 2012.
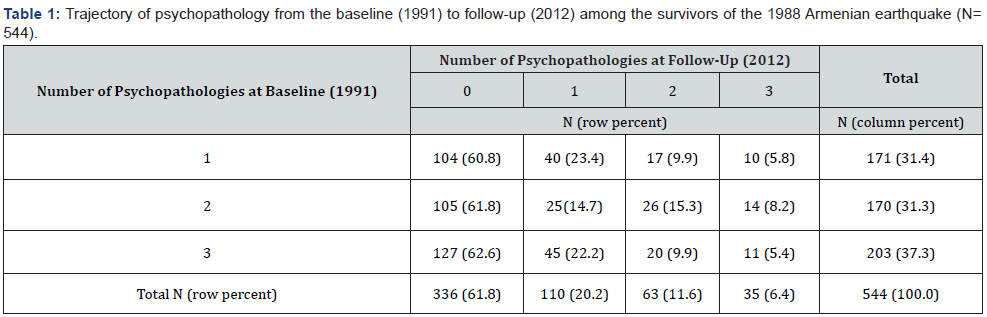
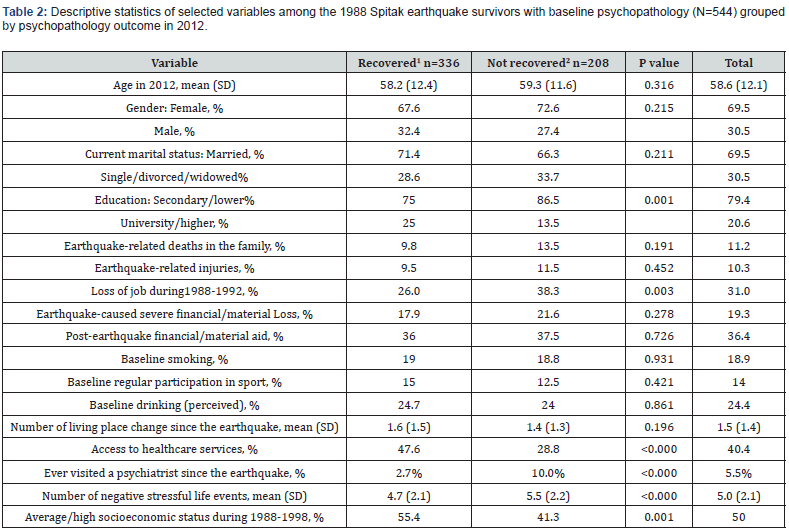
At baseline, 31% of the 544 participants had one psychopathology, 31% had two, and 37% had all three. Based on the psychological assessment conducted in 2012, 62% of individuals (N=336) had no psychopathology, and the remaining 38% (N=208) had at least one of the three psychopathologies. (Table 2) shows the comparisons of the rates for socio-demographic, earthquake and post-earthquake variables of interest between the recovered and not-recovered groups. The mean age of the sample was 59 years, 30% were males and 70% were married. A significantly higher proportion of participants who had recovered from baseline psychopathologies had higher education, better access to health care whenever needed, and better socioeconomic status during the 10 year period following the earthquake. More than a third of survivors lost their job during the post-earthquake four years. Compared to those who recovered, higher proportion of those who did not recover, reported loss of job after the earthquake.
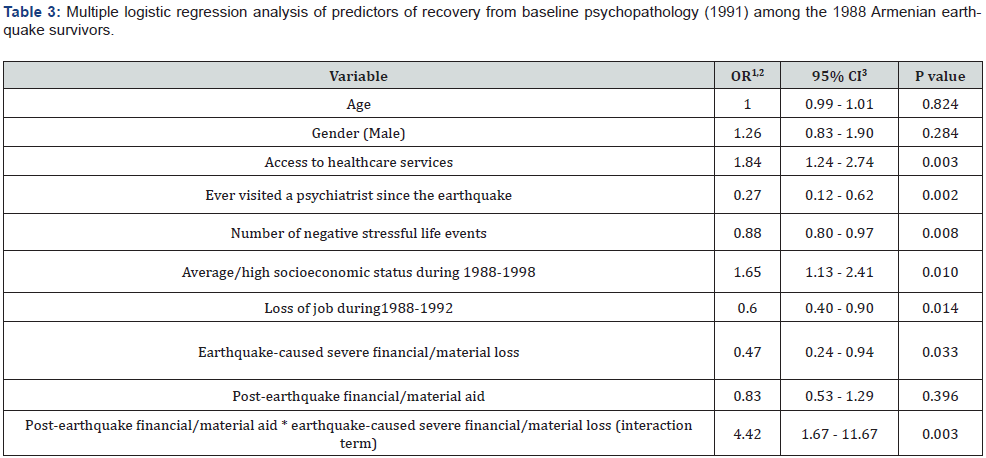
The recovered group reported significantly lower number of lifetime negative stressful events. There were no differences between the groups with regard to earthquake-related experiences; including earthquake-related injuries, earthquakerelated deaths among nuclear family members, severe financial/ material loss due to the earthquake, and acquiring postearthquake material/financial aid. Baseline health-related behaviors including smoking, drinking and active participation in sports, were also not associated with recovery status. (Table 3) presents the results from multivariable logistic regression analysis. It shows that easier access to healthcare services and average/high socioeconomic status during the 10 years following the earthquake were independently associated with higher likelihood of recovery from psychopathologies.
1Free from any psychopathology at follow-up.
2Suffers from at least one psychopathology at follow-up.
1OR: odds ratio
2Direction of the OR is toward recovery
3CI: confidence interval
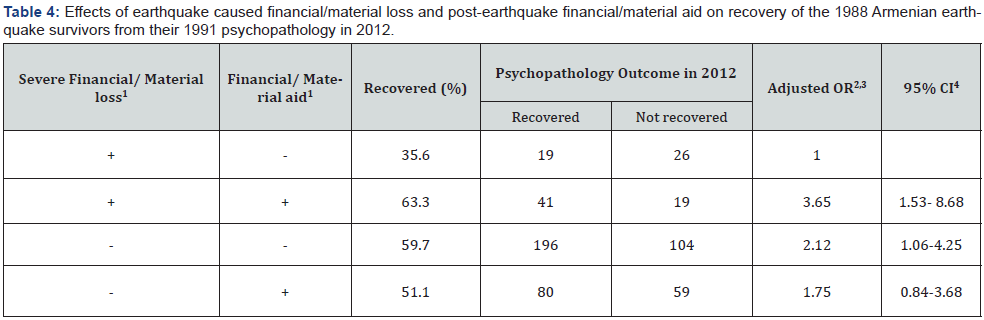
Although earthquake related financial/material loss and postearthquake financial/material aid were initially not associated with recovery, after including an interaction term comprising of severe earthquake loss and post-earthquake financial/material aid, the data showed a significant association between earthquake related severe loss and recovery, which was modified by postearthquake financial/material aid (Table 3). Among those with severe loss, individuals who received financial aid had more than 4 times higher odds of recovery than those who did not receive aid. Post-earthquake loss of job, history of visiting a psychiatrist or psychologist, and higher number of experienced negative stressful life events were also independently related to a lower likelihood of recovery. (Table 4) presents the effects of earthquake related financial/material losses and post-earthquake financial/ material aid on the recovery of survivors from psychopathology.
1Plus sign (+) indicates presence of the condition; minus sign (-) indicates its absence
2OR: odds ratio
3Odds ratios were adjusted for age, gender, access to healthcare services, BMI, number of negative stressful life events, history of visiting a psychiatrist/ psychologist, socioeconomic status during 1988-1998, and loss of job during 1988-1992.
4CI: confidence interval
Discussion
This study evaluated whether socio-demographic characteristics, earthquake and post-earthquake variables among the survivors were associated with successful recovery from early post-disaster psychopathology 23 years after the disaster. During the baseline assessment in 1991, the majority of the initial cohort met the diagnostic criteria for at least one psychopathology (PTSD, clinical depression, and/or anxiety). During the follow-up assessment in 2012, 62% of the sample did not fulfill criteria for any psychopathology (PTSD, clinical depression, and/or anxiety). We found that earthquake related financial/material loss was negatively associated with recovery from psychopathology extending our previous findings on the association between earthquake related financial/material loss and psychopathology [3,4]. The second important finding indicates that those with severe loss who received early post-earthquake financial/material aid had significantly better odds of recovery than their peers with severe losses who did not receive any financial/material aid.
These findings highlight the importance of identification of survivors with severe losses and provision of timely financial/ material aid to them for achieving better recovery outcomes. The results also showed that post-earthquake financial/material aid was only beneficial among those with severe losses. Those without such loss who received help did not have better odds of recovery. This finding can be of value for policy makers planning post disaster interventions, especially when the resources are limited. The finding of an association between loss of job during the postearthquake period and current psychopathology may be due to loss of self-worth and dignity, increased feeling of insecurity due to lack of financial resources, and restricted social interactions. The finding indicates the importance of the provision of employment opportunities to the survivors to prevent job loss and employment related problems among them. Since the significant association between loss of job and long-lasting psychopathology was robust even after controlling for socioeconomic status and access to healthcare, we have hypothesized that psychological factors such as social network disruption and dignity could have been responsible for such an association.
The results showed that negative stressful life events considerably decreased the odds of recovery from psychopathology. Negative life events are well- established risk factors for PTSD, depression and anxiety [40]. Such events have been found to be associated with the development of depression [41]and the chronic course of PTSD [42]. Schnurr and colleagues [43]showed that current social support and recent stressful life events were associated with chronicity of PTSD. There is an established strong association between socioeconomic status and health outcomes including mental morbidity [44]. It is noteworthy that socioeconomic status during the decade following the earthquake was associated with the recovery from post-earthquake psychopathology in the current study. Another important factor associated with the recovery was access to healthcare services. This remained a significant determinant of recovery even after controlling for socioeconomic status.
Although primary care is formally free in Armenia, because of the widespread practice of informal payments for care during the last decades, access to healthcare services was a significant problem [45], particularly for individuals living in the earthquake region, as the proportion of population living under poverty line was the highest here (more than 40%) [46]. The present finding provides empirical evidence for providing appropriate medical care and ensuring access to healthcare as a priority for disaster survivors with high rates of physical and psychiatric conditions [1,27]. Those who reported a history of receiving consultation from a psychiatrist or a psychologist during their life time had a significantly reduced likelihood of recovery from psychopathology. Their use of mental health services suggests the presence of a preexisting/chronic mental health problem (prior to the earthquake). Despite high needs for mental health services in Armenia, the utilization of these services is low [47], mainly due to the existing negative stigma about mental illness and low level of recognition of the existence of such problem among the general population [47].
Several potential limitations of this study should be acknowledged. Misclassification of individuals at the baseline psychological assessment had a potential to bias our findings. However, we believe that it was not a serious threat to the robustness of our findings because of several reasons: first of all the instruments utilized during that assessment were based on internationally accepted measures and were pretested and compared against clinical diagnosis showing high diagnostic validity [3,4]. Second, the majority of the participants with psychopathology during the baseline had multiple psychopathologies (69%), which makes it even less likely to have false positive cases, and finally only a small portion of the studied cohort did not have a psychopathology at baseline, which shrunk the chances of false negative cases, thus, reducing overall chances of misclassification.
Since this study conducted a cross sectional assessment of psychopathology at two phases, it was possible that some of the individuals who underwent the recent psychological assessment and were identified as being recovered were in a remission phase during the assessment. Nonetheless, we expect such potential bias to be toward the null. We were limited in making conclusions about whether the factors identified were associated with the duration of the disease or incidence rates of psychopathology that affected their chances of full recovery. Differentiation of these two categories (duration of psychopathology and incidence) would require more frequent and comprehensive assessments of the survivors. Based on our findings we suggest further studies exploring these factors in depth to determine their role on the incidence and course of post-disaster psychopathologies.
Conclusion
The study’s uniqueness is in that it followed the course of the psychopathology of subjects exposed to a disaster over two decades. The identified risk factors (earthquake related losses, post-earthquake stressful life events, and , unemployment) and the benefits of early intervention (post-earthquake aid, access to healthcare) in altering the trajectory of psychopathology could assist clinicians to better identify post disaster high risk groups and for policy makers to allocate appropriate resources accordingly in reduce psychopathology.
Acknowledgement
We would like to acknowledge the generous support of the Turpanjian Family Educational Foundation. This work was supported in part by a grant from the National Institute of Mental Health (Dr. Khachadourian [Award number T32-MH122394]). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies or the authors’ employers.
References
- Armenian HK, Melkonian AK, Hovanesian AP (1998) Long term mortality and morbidity related to degree of damage following the 1998 earthquake in Armenia. Am J Epidemiol 148(11): 1077-1084.
- Watanabe H, Kodama M, Tanabe N, Nakamura Y, Nagai T, et al. (2008) Impact of earthquakes on risk for pulmonary embolism. Int J Cardiol 129(1): 152-154.
- Armenian HK, Morikawa M, Melkonian AK, Hovanesian A, Akiskal K, et al. (2002) Risk factors for depression in the survivors of the 1988 earthquake in Armenia. J Urban Health 79(3): 373-382.
- Armenian HK, Morikawa M, Melkonian AK, Hovanesian AP, Haroutunian N, et al. (2000) Loss as a determinant of PTSD in a cohort of adult survivors of the 1988 earthquake in Armenia: implications for policy. Acta Psychiatr Scand 102(1): 58-64.
- Carr VJ, Lewin TJ, Webster RA, Kenardy JA, Hazell PL, et al. (1997) Psychosocial sequelae of the 1989 Newcastle earthquake: II. Exposure and morbidity profiles during the first 2 years post-disaster. Psychol Med 27(1): 167-178.
- Goenjian AK, Pynoos RS, Steinberg AM, Najarian LM, Asarnow JR, et al. (1995) Psychiatric comorbidity in children after the 1988 earthquake in Armenia. J Am Acad Child Adolesc Psychiatry 34(9): 1174-1184.
- Papadatos Y, Nikou K, Potamianos G (1990) Evaluation of psychiatric morbidity following an earthquake. Int J Soc Psychiatry 36(2): 131-136.
- Zhang Z, Shi Z, Wang L, Liu M (2012) Post-traumatic stress disorder, anxiety and depression among the elderly: a survey of the hard-hit areas a year after the Wenchuan earthquake. Stress Health 28(1): 61-68.
- Norris FH, Murphy AD, Baker CK, Perilla JL (2004) Postdisaster PTSD over four waves of a panel study of Mexico's 1999 flood. J Trauma Stress 17(4): 283-292.
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, et al. (2002) 60,000 Disaster Victims Speak: Part I. An Empirical Review of the Empirical Literature, 1981–2001. Psychiatry 65(3): 207-239.
- Green BL, Lindy JD, Grace MC, Leonard AC (1992) Chronic posttraumatic stress disorder and diagnostic comorbidity in a disaster sample. J Nerv Ment Dis 180(12): 760-766.
- McFarlane AC, Papay P (1992) Multiple diagnoses in posttraumatic stress disorder in the victims of a natural disaster. J Nerv Ment Dis 180(8): 498-504.
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB (1995) Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 52(12): 1048-1060.
- Bonanno GA (2004) Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol 59(1): 20-28.
- Castleden M, McKee M, Murray V, Leonardi G (2011) Resilience thinking in health protection. Journal of public health 33(3): 369-377.
- Galea S, Nandi A, Vlahov D (2005) The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev 27: 78-91.
- Pietrzak RH, Tracy M, Galea S, Kilpatrick DG, Ruggiero KJ, et al. (2012) Resilience in the face of disaster: prevalence and longitudinal course of mental disorders following hurricane Ike. PLoS One 7(6): e38964.
- Engdahl B, Dikel TN, Eberly R, Blank A (1997) Posttraumatic stress disorder in a community group of former prisoners of war: a normative response to severe trauma. Am J Psychiatry 154(11): 1576-1581.
- Sutker PB, Allain AN, Winstead DK (1993) Psychopathology and psychiatric diagnoses of World War II Pacific theater prisoner of war survivors and combat veterans. Am J Psychiatry 150(2): 240-245.
- Morgan L, Scourfield J, Williams D, Jasper A, Lewis G (2003) The Aberfan disaster: 33-year follow-up of survivors. Br J Psychiatry 182: 532-536.
- Marshall GN, Schell TL, Elliott MN, Berthold SM, Chun CA (2005) Mental health of Cambodian refugees 2 decades after resettlement in the United States. JAMA 294(5): 571-579.
- Goenjian AK, Steinberg AM, Najarian LM, Fairbanks LA, Tashjian M, et al. (2000) Prospective study of posttraumatic stress, anxiety, and depressive reactions after earthquake and political violence. Am J Psychiatry 157(6): 911-916.
- Wolfe J, Erickson DJ, Sharkansky EJ, King DW, King LA (1999) Course and predictors of posttraumatic stress disorder among Gulf War veterans: a prospective analysis. J Consult Clin Psychol 67(4): 520-528.
- Bland SH, Valoroso L, Stranges S, Strazzullo P, Farinaro E, et al. (2005) Long-term follow-up of psychological distress following earthquake experiences among working Italian males: a cross-sectional analysis. J Nerv Ment Dis 193(6): 420-423.
- Lazaratou H, Paparrigopoulos T, Galanos G, Psarros C, Dikeos D, et al. (2008) The psychological impact of a catastrophic earthquake: a retrospective study 50 years after the event. J Nerv Ment Dis 196(4): 340-344.
- Neria Y, Nandi A, Galea S (2008) Post-traumatic stress disorder following disasters: a systematic review. Psychol Med 38(4): 467-480.
- Goenjian AK, Najarian LM, Pynoos RS, Steinberg AM, Manoukian G, et al. (1994) Posttraumatic stress disorder in elderly and younger adults after the 1988 earthquake in Armenia. Am J Psychiatry 151(6): 895-901.
- Najarian LM, Goenjian AK, Pelcovitz D, Mandel F, Najarian B (2001) The effect of relocation after a natural disaster. J Trauma Stress 14(3): 511-526.
- Goenjian AK, Noble EP, Walling DP, Goenjian HA, Karayan IS, et al. (2008) Heritabilities of symptoms of posttraumatic stress disorder, anxiety, and depression in earthquake exposed Armenian families. Psychiatr Genet 18(6): 261-266.
- Robins LN, Helzer JE, Croughan J, Ratcliff KS (1981) National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry 38(4): 381-389.
- Eaton WW, Regier DA, Locke BZ, Taube CA (1981) The Epidemiologic Catchment Area Program of the National Institute of Mental Health. Public Health Rep 96(4): 319-325.
- Watson CG, Juba MP, Manifold V, Kucala T, Anderson PE (1991) The PTSD interview: rationale, description, reliability, and concurrent validity of a DSM-III-based technique. J Clin Psychol 47(2): 179-188.
- Hendricks LE, Bayton JA, Collins JL, Mathura CB, McMillan SR, et al. (1983) The NIMH Diagnostic Interview Schedule: a test of its validity in a population of black adults. J Natl Med Assoc 75(7): 667-671.
- Weathers F, Litz B, Herman D, Huska J, Keane T (1993) The PTSD checklist: reliability, validity, & diagnostic utility. Annual Meeting of the Internationl Society of Traumatic Stress studies, San Antonio, TX.
- Movsisyan A (2013) Diagnostic Accuracy of Post-traumatic Stress Disorder Checklist - Civilian Version and Modified Versions of Center for Epidemiologic Studies Depression Scale among 1988 Spitak Earthquake Survivor: A Cross-Sectional Study: American University of Armenia.
- Radloff LS (1977) The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurements 1(3): 385-401.
- Demirchyan A, Petrosyan V, Thompson ME (2011) Psychometric value of the Center for Epidemiologic Studies Depression (CES-D) scale for screening of depressive symptoms in Armenian population. J Affect Disord 133(3): 489-498.
- Derogatis LR, Unger R (2010) Symptom Checklist‐90‐Revised. Corsini Encyclopedia of Psychology.
- Najarian LM, Sunday S, Labruna V, Barry I (2011) Twenty-year follow-up of adults traumatized during childhood in Armenia. J Affect Disord 135(1-3): 51-55.
- Hammen C (2011) Association between recent stressful life events and prevalence of depression, anxiety and PTSD differs according to exposure to childhood adversity. Evid Based Ment Health 14(1): 9.
- Kendler KS, Karkowski LM, Prescott CA (1999) Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry 156(6): 837-841.
- Pietrzak RH, Van Ness PH, Fried TR, Galea S, Norris FH (2013) Trajectories of posttraumatic stress symptomatology in older persons affected by a large-magnitude disaster. J Psychiatr Res 47(4): 520-526.
- Schnurr PP, Lunney CA, Sengupta A (2004) Risk factors for the development versus maintenance of posttraumatic stress disorder. J Trauma Stress 17(2): 85-95.
- Hudson CG (2005) Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry 75(1): 3-18.
- Erica R (2013) Armenia: Health system review. Health Syst Transit 15(4): 1-99.
- NSS (2012) Social Snapshot and Poverty in Armenia. Yerevan: National Statistical Service of the Republic of Armenia.
- van Baelen L, Theocharopoulos Y, Hargreaves S (2005) Mental health problems in Armenia: low demand, high needs. Br J Gen Pract 55(510): 64-65.






























