COVID-19 Mental Health Challenges: A Systematic Review, Logistic Regression and Principal Component Analysis
Savita J Gaur, Usha Panjwani* and Bhuvnesh Kumar
Department of Neurophysiology, Defence Institute of Physiology and Allied Sciences (DIPAS), India
Submission: May 27, 2020; Published: July 17, 2020
*Corresponding author: Usha Panjwani, Department of Neurophysiology, Defence Institute of Physiology and Allied Sciences (DIPAS), DRDO, Delhi -54, India
How to cite this article: Savita J G, Usha P, Bhuvnesh K. COVID-19 Mental Health Challenges: A Systematic Review, Logistic Regression and Principal Component Analysis. Psychol Behav Sci Int J .2020; 15(1): 555905. DOI: 10.19080/PBSIJ.2019.10.555905.
Abstract
Background: World Health Organization (WHO) declaredCOVID-19 (SARS-COV2) viral infection as Pandemic on January 31, 2020. The virus is a highly transmittable and pathogenic displaying primary symptoms of elevated temperature, cough, headache and to some extent loss of taste or smell. However, there are imperceptible psychological effects that are difficult to assess and cure than relevant physical indicators. COVID-19 Positive patients and Medical staff are at high risk to get affected psychologically. Therefore, the mental health status is required to be monitored on priority basis. This study aims to review, synthesize, and analyse published evidence on the prevalence of, anxiety, depression and insomnia among patients, medical staff and others (general population) during the Covid-19 outbreak.
Method: Based on PRISM Statement systematic search and review of published data till May 2020 on SARS-COV2 related psychological factors was carried. Logistic regression and PCA was carried out to assess the prevalence of specific psych-factor. Findings: The studies in included in the review, assessed anxiety, depression, distress, insomnia, and suicidal cases in relation to COVID-19. Participants reported psychological burden and high prevalence rates of depression, anxiety and insomnia were observed. Interpretation: COVID-19 patients, frontline medical staff, are at higher risk of mental health challenges. The study recommends psychological prescription to COVID-19 patients, medical staff and general population.
Keywords:COVID-19; Psychological anxiety; Logistic regression; PCA
Introduction
COVID-19 or SARS-COV2is an infectious virus newly discovered in the coronavirus family. World Health Organization (WHO) declaredCOVID-19 (SARS-COV2) viral infection as Pandemic on January 31, 2020 [1]. The COVID-19 virus is mainly transmitted by coming in close proximity of a person who is COVID-19 positive. The virus spreads through droplets generated when a person coughs, sneezes, or exhales. To control the spread of viral infection around 4 billion i.e. half of the world population have been ordered by respective Governments to follow home confinement that is apparently the largest psychological experiment ever. Till date, Globally, there have been 4, 904, 413 confirmed cases of COVID-19, including 323,412 deaths, reported to WHO [1]. According to reported researched during epidemic and/or deadly illnesses there are enormous mental pressure on affected population. Social distancing, isolation, and fear of COVID-19, inadequate PPEs are making people vulnerable to mental health problems specifically on patients and frontline medical staff [2,3]. During quarantine, home confinement and while carrying out essential health care duties it’s likely that one feels anxious, depressed and concurrently loses sleep [4]. Increased workload, physical exhaustion, inadequate and nosocomial transmission, fear of corona virus is supposed to elevate the most common emotion that is anxiety. Also, persons who had mental health history may face novel psychological challenges or their condition may worsen during Corona Quarantine. A dramatic decline in physical and mental well-being has also triggered some suicide cases related to COVID-19. Therefore, the Psychological support during COVID-19 Pandemic is vital towards enhancing resilience and good mental health. The aim this study is to carry out Review of COVID-19 related Psychological disorders. We will compile and evaluate the data set that gives evidence of psychological issues due to COVID infection and find out emerging prevalence of Anxiety, Depression, and Insomnia. This will help in crafting precautionary measures to mitigate the toxic mental health effects of COVID-19.
Material and Methods
Study design
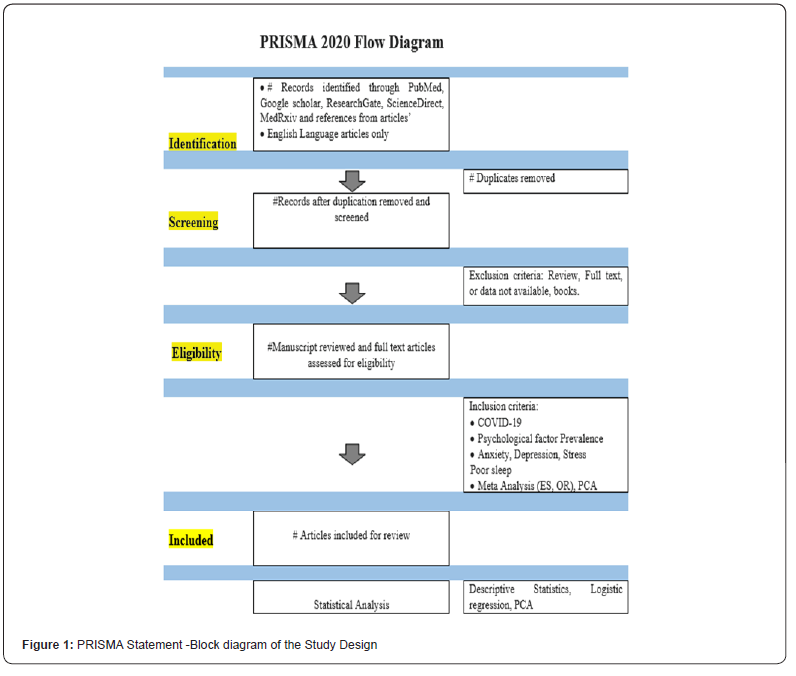
The study design was Systematic Review of published researched articles, extraction of data based on inclusion and exclusion criterion set and result interpretation after statistical analysis. The methodical literature review and selection criteria to extractCOVID-19 data was in accordance with the PRISMA statement depicted in Figure 1.
Data extraction
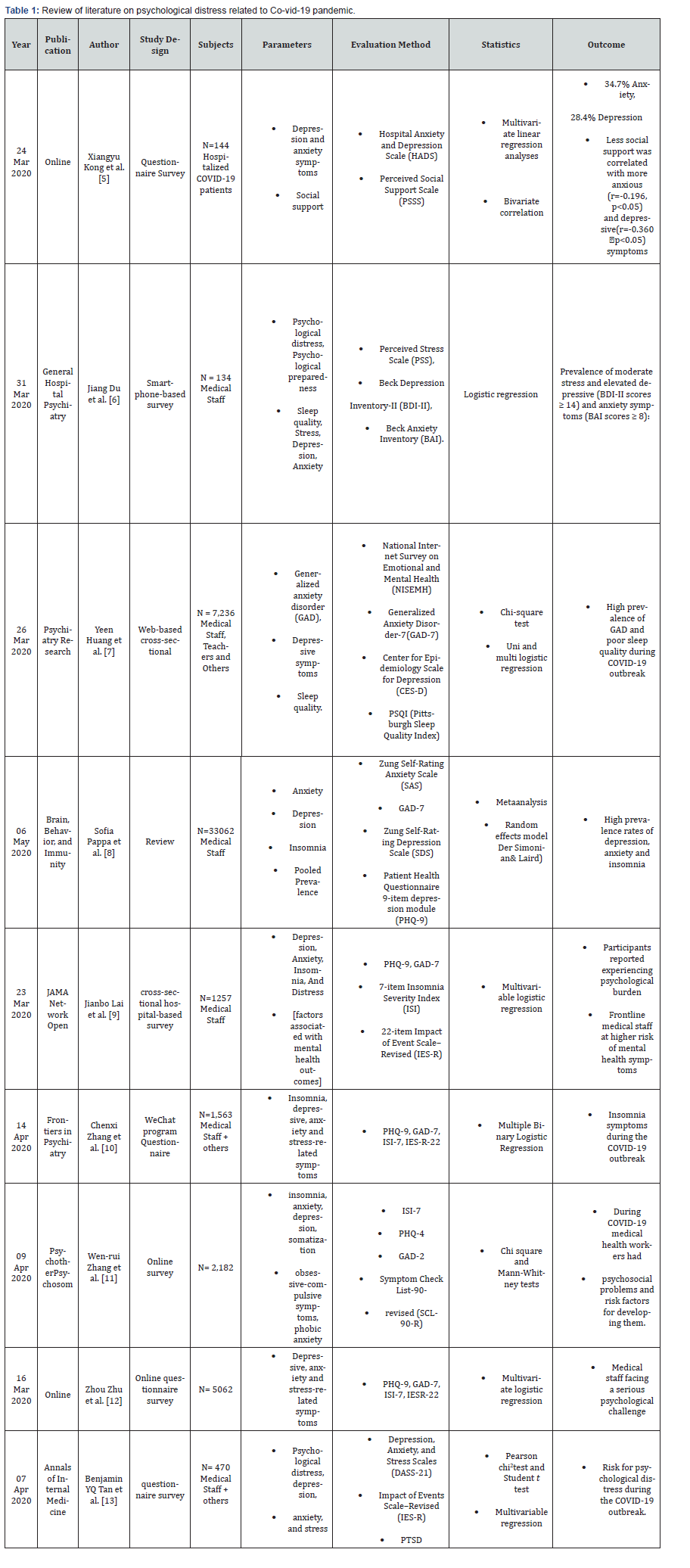
The psychological data of anxiety, depression, poor sleep, suicidal cases linked to the COVID-19 positive patients, Quarantine population, medical professionals and general population were extracted from published articles on PubMed, Google scholar, Research gate, ScienceDirect, MedRxiv sites [5-13]. Further the references from articles were used to increase data base. Only English Language articles were searched and retrieved. The few of the total reviewed journals are listed in Table 1.
Data synthesis and analysis
Microsoft Excel for Windows was utilized in the current study to synthesize and organise data. The data was arranged as Author, publication and year, sample population, evaluation test methods applied, sample size and sample characteristics, age and gender, statistical method applied for assessment, psychological parameters determined and result outcomes. Details are presented in Table 1. The primary psychological parameters retrieved were Anxiety, Depression, Insomnia, Distress (Figure 1).
Results and Discussion
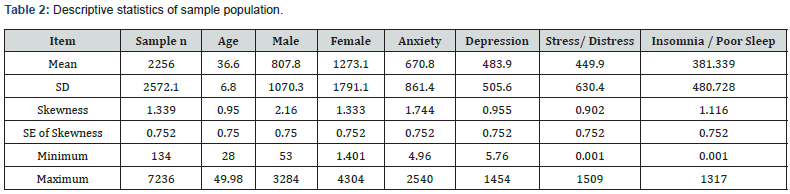
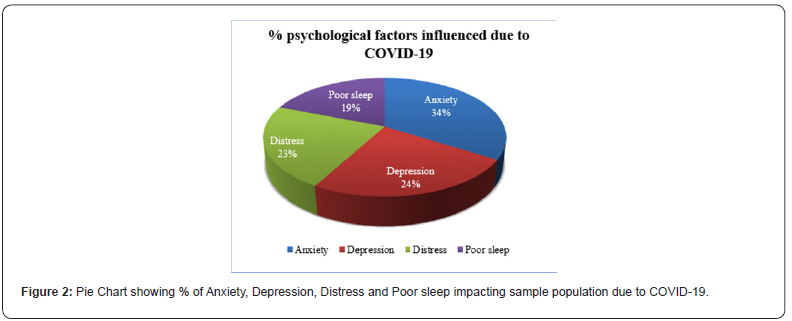
The statistics of the included sample in the study is shown in the descriptive statistics in Table 2. A total of n= 18,048 samples from the 8 studies where included in the analysis. All the studies reported the psychological factors like anxiety, depression, stress and insomnia in medical staff and general population during the COVID-19 pandemic. Some studies that were reviewed had also reported cases of PSTD, Suicide, fear and social connect factor related to lockdown. Out of 8 studies 6 was in mainland china and one was in Wuhan city and one was in Singapore (Figure 2).
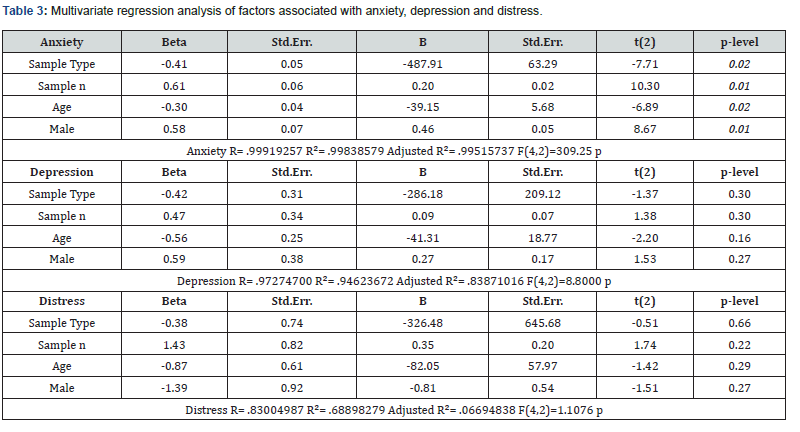
The multiple linear regression analysis (Table 3) showed that sample type (β=-0.41, p=0.02), Sample number (β 0.61, p=0.01), age (β=-0.30, p=0.02), and gender/male (β =0.58, p=0.01) were associated with anxiety for COVID-19. As compared to anxiety, depression and stress affected people due to COVID-19 to a lesser degree.
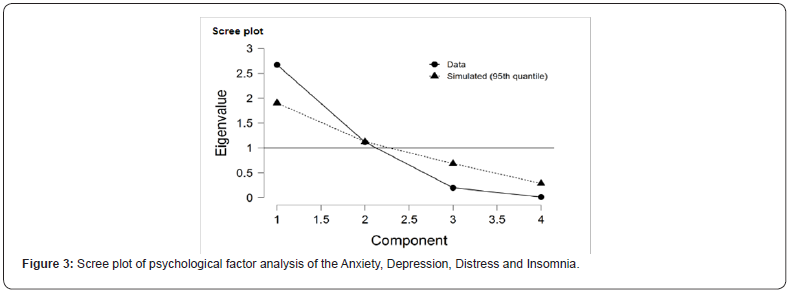
Principal component analysis results determined correlation between psychological factors. The principal component analysis revealed the existence of two components with eigen value over 1, that is Anxiety with eigen value (Ɛ=2.67) and Depression having eigen value (Ɛ=1.11).The % of variability among the samples is more by Principal Component analysis PC1(Anxiety) than PC2(- Depression) (Figure 3).
Conclusion
There is considerable evidence to conclude that patient of COVID-19 and general population experienced anxiety, depression and felt endangered during COVID-19 pandemic peak period. There were confirmed cases of suicide under distress of Corona virus. The present study recommends paying attention towards the mental health of patients, frontline health care workers in terms of providing good quality protection gears, psychological support and prescription and strong family support during and post the COVID-19 epidemic.
References
- (2020) World Health Organization.
- Sritharan, Jeavana, Sritharan Ashvinie (2020) Emerging Mental Health Issues from the Novel Coronavirus (COVID-19) Pandemic. In: Journal of Health and Medical Sciences 3(2): 157-162.
- Lai J, Ma S, Wang Y, Wang Y, Cai Z, et al. (2020) Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open 3(3): e203976.
- Fardin MA (2020) COVID-19 and Anxiety: A Review of Psychological Impacts of Infectious Disease Outbreaks. Arch Clin Infect Dis.
- Kong X, Zheng K, Tang M, Kong F, Zhou J, et al. (2020) Prevalence and Factors Associated with Depression and Anxiety of Hospitalized Patients with COVID-19.
- Du J, Dong L, Wang T, Chenxin Yuan, Rao Fu, et al. (2020) Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry.
- Huang Y, Zhao N (2020) Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional Survey. PII: S0165-1781(20): 30607-7.
- Pappaet S, Ntellac V, Gianna T, Giannakoulisc VG, Papouts E, et al. (2020) Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity.
- Laiet J, Simeng Ma, Wang Y, Cai Z, Hu J (2020) Factors Associated With Mental Health Outcomes Among Health CareWorkersExposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3(3): e203976.
- Zhang C (2020) Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Frontiers in Psychiatry. 11: 306.
- Wen-rui Zhang, Wang K, Yin L, Zhao W, et al. (2020) Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in china. Psychother Psychosom.
- Zhu Z, Xu S, Wang H, Liu Z, Wu J, et al. (2020) COVID-19 in Wuhan: Immediate Psychological Impact on 5062 Health Workers. Med Rxiv preprint.
- Benjamin YQ, Tan, Nicholas WS, Chew, Grace KH Lee, MD et al. (2020) Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Annals of Internal Medicine.
- Shacham M, Raz YM, Kolerman R, Mijiritsky O, Ben-Ezra M, et al. (2020) COVID-19 Factors and Psychological Factors Associated with Elevated Psychological Distress among Dentists and Dental Hygienists in Israel. Int. J. Environ. Res. Public Health 17: 2900.
- Wei-jie Guan, Wen-hua Liang, Yi Zhao, Heng-rui Liang, Zi-sheng Chen, et al. (2020) Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. EurRespir J 55: 2000547.
- Zhang Y, Ma ZF (2020) Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int J Environ Res. Public Health 17: 2381.
- Griffiths MD, Mamun MA (2020) COVID-19 suicidal behavior among couples and suicide pacts: Case study evidence from press reports. Psychiatry Research 289:113105.






























