The Relevance of the Psychosocial Dimension: Evaluation of the Psychosocial Aspects in Obese Patients who are Candidates to Bariatric Surgery
Telma Patrícia Queirós Santos1*, Sara Joana Santos Viveiros2, Ana Raquel Sousa e Silva3 and Maria del Carmen Palmira Coya García2
1Departamento de Psiquiatria e Saúde Mental, Centro Hospitalar do Baixo Vouga, E.P.E, Aveiro, Portugal
2Unidade de Psiquiatria de Ligação e Psicologia da Saúde, Centro Hospitalar do Porto(CHP), Portugal
3Faculdade de Ciências Sociais e Humanas da Universidade da Beira Interior, Portugal
Submission: June 08, 2019; Published: July 03, 2019
*Corresponding author: Telma Patrícia Queirós Santos, Departamento de Psiquiatria e Saúde Mental, Centro Hospitalar do Baixo Vouga, E.P.E, Aveiro, Portugal
How to cite this article: Telma Patrícia Queirós Santos*, Sara Joana Santos Viveiros, Ana Raquel Sousa e Silva and Maria del Carmen Palmira Coya García. The Relevance of the Psychosocial Dimension: Evaluation of the Psychosocial Aspects in Obese Patients who are Candidates to Bariatric Surgery. Psychol Behav Sci Int J. 2019; 12(3): 555965. DOI: 10.19080/PBSIJ.2019.12.555965
Abstract
Introduction: The objective of this study is to evaluate and characterize the psychosocial aspects of the patients eligible for bariatric surgery, which will allow a better understanding of the way people deal with the overweight and its influence on their emotional, social and personal experiences.
Material and Methods: It is a descriptive exploratory and transversal study. It is also inferential about the patients who were candidates for bariatric surgery in a hospital in the north of Portugal, focusing on the categories of anxiety level, depression and binge eating disorder. A questionnaire and two scales were used: Pre-Bariatric Surgery Questionnaire of the Program of the Surgical Treatment of Obesity (Porto Hospital); Binge Eating Scale; and Hospital Anxiety and Depression Scale.
Results: Results showed that 30.6% of the patients suffered from binge eating disorder, 56% from anxiety and 37% from depression. There was a significant difference between the genders, being females more prone to anxiety and binge eating disorder.
Conclusion: The psychopathologies investigated here were present only in a small number of candidates. However, this population seems to be more vulnerable than the general one, being suggested that the professional involved with mental health should be present along the surgical process.
Keywords: Obesity; Psychosocial, Bariatric Surgery
Introduction
According to the World Health Organization (WHO), obesity has increased almost three times in the world since 1975. In 2016 more than 1,9 billion adults were considered to be overweighted (Body Mass Index (BMI) > 25kg/m2) and, from those, 650 million were obese (BMI > 30 kg/m2). Another report from the WHO (2008) showed that 60% of the population from Portugal were overweited and 25% were obese, being the prevalence of overweight and obesity higher in adults, men (21,6%) and women (26,3%) [1,2].
In the past, genetic would be used to explain such disorders, being psychological factors and life style seen as secondary causes. However, some studies have highlighted the relationship between eating and mental disorders and the negative efect of being overweighted over the way the individuals experience their professional, academic and personal life [3]. Obesity is a chronic and complex disease, with social and psychological implications, that may affect people from different ages and socioeconomic groups [3-6]. Lately, it has been a consensus among health professionals that obesity is the result of more than only biochemical imbalances and physical-metabolic diseases, it is also caused by symptomatological and psychological disorders related to difficulties with social adaptation [5]. The change of the body image in the obese may be related to the devaluation of the self-image and the self-concept, which will affect their self-esteem [5] and, consequently, depressive and anxious symptoms, a decrease in the feeling of wellbeing and relational issues may arise [7]. The association between affective disorders and obesity has been empirically acknowledged and some studies have been trying to elucidate this relationship, but the results are still contradictory [2,7,8]. Conservative treatments for obesity may not work, especially when patients present class II (BMI >35 kg/m2) and III (BMI > 40 kg/m2) obesity, and, for these cases, the bariatric surgery has been indicated [9]. It is known that 2/3 of the population seeking bariatric surgery has psychiatric diagnosis, being depression the commonest, with a prevalence of 20-50% [2,4].
The association between morbid obesity, binge eating disorder, anxiety and depression is largely studied [10-12] and, lately, the interest in studies involving psychosocial variables associated to the bariatric surgery has been increasing significantly [13]. There seem to be clear evidences regarding the influence of these variables in the life of obese people and in the results of the treatment for obesity, as they affect the loss of weight, the adherence to post-operative period, and medication and diet compliances [13,14]. Accordingly, the General Health Department of the Portuguese government indicates the psychological and/or psychiatric evaluation of the individuals eligible for surgical treatment for obesity, indicating at least one consultation, but preferably two (pre and post-surgical). Such evaluations should use suitable tools that will allow a proper evaluation of the patient from the point of the view of the mental health/ disease [15].
Therefore, the objective of this study is to evaluate and characterize the psychosocial aspects of the patients eligible for bariatric surgery using standardized questionnaires and inventories to assess depression, anxiety and binge eating disorder. Data originated from this study will allow a better understanding of the way people deal with the overweight and its influence on their emotional, social and personal experiences, which could anticipate and improve the post-surgical outcome.
Material and Methods
Data was collected according to what is established by the General Health Department of the Portuguese government and as part of the multidisciplinary evaluation of the patients eligible for bariatric surgery in Porto Hospital (Portugal). The evaluation sessions were conducted by a psychiatrist and a psychologist. After the first interview, the candidates were conducted to a room where they received the questionnaires and filled them; if they had any doubts there were doctors in the room to help them to answer the questions.
The non-probabilistic sample comprised 339 patients with morbid obesity (class II or III) who were candidates to bariatric surgery and had been previously submitted to the multidisciplinary evaluation of the Hospital. The interviews were conducted in Portuguese and they were done between January 2016 and January 2018. It was a descriptive exploratory and transversal study. It was also inferential and evaluated the psychosocial dimensions of these patients, focusing on the categories of anxiety level, depression and binge eating disorder. Later, the psychosocial profile of the patient was assessed and compared with the other variables of the study. Two psychometric scales and a questionnaire were applied to the patients (anonymously) who gave their written informed consent.
Pre-Bariatric Surgery Questionnaire of the Program of the Surgical Treatment of Obesity (Porto Hospital) – It is a set of questions elaborated by specialists in the area which focus on the clinical aspects of the patient. It is divided in 5 areas: Personal Information (name, date of birth, sex, age, weight, height, BMI, marital status, education, profession and current professional situation); psychiatric history; family psychiatric background; food behaviour; and personal history. Binge Eating Scale [BES; Gormally, Black, Daston, & Rardin (1982)] - This scale was adjusted and validated into Portuguese by Tapadinhas and Ribeiro (2009). This instrument allows the evaluation of behavioural manifestations, feelings and cognition associated to compulsive binge and qualifies it. BES is formed by 16 items and 62 statements, for example: “I usually eat when I am upset. Nothing seems to help to cease this habit”; and the statements range from the absence of the behaviour to the extreme severity of it. The given value for each item range within the ordinal Likert scale of three points. The sum of the score for each response (total score) shows distinguishing levels of bingeeating severity: a) total score of 17 or less: there is no evidence of binge eating disorder (BED); b) total score ranging from 18 to 26: moderate BED; and c) total score of 27 or higher: severe BED [16].
Hospital Anxiety and Depression Scale (HAD; Zigmond & Snaith, 1983) - This scale was adjusted and validated into Portuguese by M Baltar and J Ribeiro (2007). This scale is used to evaluate, succinctly, the anxiety and depression levels of individuals who are in outpatient treatment. The scale was developed to be used in the hospital settings and it is composed by 14 items divided into two sub-scales: anxiety (7 items) and depression (7 items), which cumulatively produce the final score. The response is classified from zero (low) to three (high), in a Likert scale of four points. The results may have a score that ranges from 0 to 21, where the highest scores correspond to highest levels of anxiety and depression: normal: ranging from 0 to 7; mild: ranging from 8 to 10; moderate: ranging from 11 to 14; and severe: ranging from 15 to 21 [17].
Data was analysed by the IBM-SPSS program, version 22.0, using frequency measures, central tendency and dispersion and inferential analysis. The Student t-test (p<0.05) was used to compare the relationship between the genders and BED, anxiety and depression.
Results
From the 339 patients evaluated, 78.8% were women and 21.2% men, ranging from 18 to 65 years old (average 43.82 years). Most individuals were from the north of Portugal, and more than half of them (54.9%) were from Porto district. Regarding marital status, 56.3% are married, 22.7% single, 9.4% separated or divorced, 9.1% are in cohabitation and 1.8% are widows/widowers. The majority of them (57.5%) has an occupation/job, 29.2% are unemployed, 6.8% are retired, 1.5% are students and 4.7% declared having a different situation. Most individuals have finished secondary school (32.2%), 23% finished primary school (9 years education – 3rd cycle), 19.4% studied four years (1st cycle), 13.6% studied six years (2nd cycle), and 11.2% has a university degree. One patient did not inform his/her profession and two their education level.
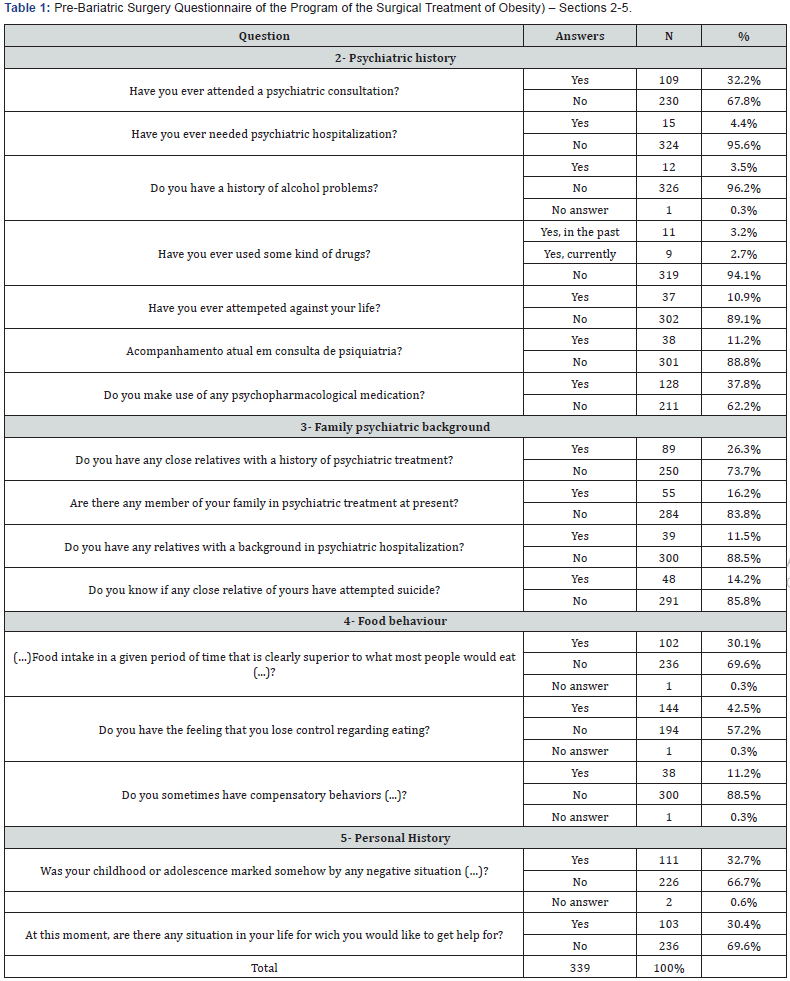
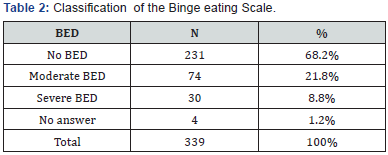
The average value of the Body Mass Index was of 43.04 kg/ m2, and the patients related that overwieight has appeared when they were, on average, 21.7 years old, ranging from 2 to 59 years. Most patients put on weight when they were adults (48.4%), 1.5% in childhood (0-11 years old), and 8.3% in adolescency (12-17 years old) (Table 1). Table 2 shows that more than half of the patients (68.2%) do not present BED. When we look at the patients who suffered of BED (30.6%), we can see that 21.8% suffered from moderate BED and 8.8% from severe BED.
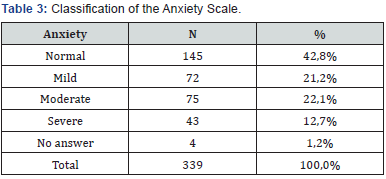
i. Anxiety Sub-scale: Most patients (56%) presented some level of anxiety, being 12.7% considered severely anxious, 22.1% moderately anxious and 21.2% mildly anxious (Table 3).
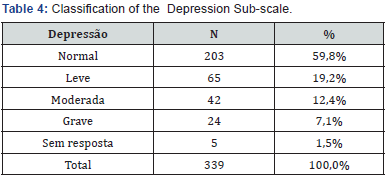
ii. Depression Sub-scale: 59.8% of the patients did not have depression. 19.2% presented mild depression, 12.4% moderate depression and 7.1% severe depression Table 4.
Regarding the differences between genders, and their relationship with BED, anxiety and depression the following results were found:
a. BED: 81.9% of men and 65.4% of women did not have BED.
b. Anxiety: Most men (62.5%)did not present symptoms of anxiety, while 21.7% of women had mild values, 25.1% moderate values and 15.2% severe values; only 38% of women did not present the symptoms. The values of anxiety were significantly different difference
c. Depression: Most men (69.4%) presented normal values for depression, 15.3% of them presented mild values, 8.4% moderate and 6.9% severe. Regarding women, 58.4% showed normal levels for depression, 20.6% presented mild values, 13.7% moderate and 7.3% severe.
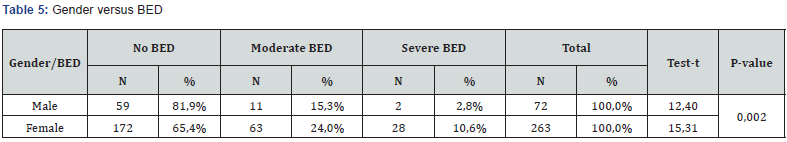
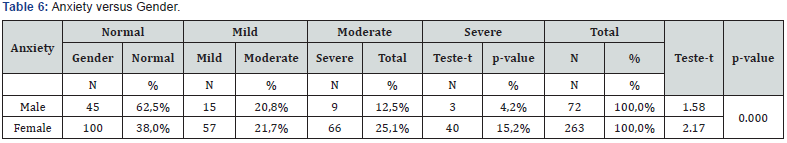
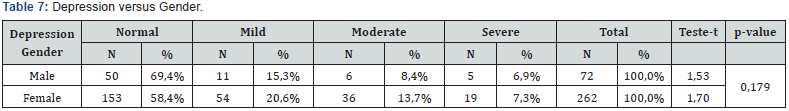
The diferences between men and women were significantly different (p<0.002) for BED (Table 5) and anxiety (Table 6), being women more prone to this disorders. However, the same was not verified for depression (p = 0.179) (Table 7).
Discussion
The present study presented some limitations. Some psychosocial characteristics were not evaluated, such as marital and sexual life, family characteristics, physical activity, social relationships, and the patients’ perception of their quality of life. It was also a transversal descriptive study which questionnaires were filled by the patients themselves, depending on their subjective interpretation of the questions.
The average profile of the patients who were candidates to bariatric surgery was established as: a married 44-yearold woman, who has finished the 2nd or 3rd cycle of primary education and is employed. She has begun to put on significant weight when was 21 years old and has a BMI of 43kg/m2. This woman and the members of her family have also no psychiatric or psychological history and she also do not present symptoms for BED and relevant levels of anxiety and depression; however, anxiety may present some impact. It may also be inferred that only a minority of the candidates to the surgery presented the psychopathologies investigated and there was no domain of one of psychopathologies over the others, being these results corroborated by others in the same area [9,18,19].
Despite the profile above, it is important to highlight that 1/3rd of population was attending psychiatric treatment, made use of psychopathological therapy and had experienced some negative experience in childhood. Also, 40% of the candidates reported losing control over food intake, being BED present in 30.6% of the cases, anxiety in 34.8% and depression in 19.5%. If we compare our results with the prevalence of anxiety (16.5%) and depression (7.9%) [20] in the Portuguese population, it is evident that this population present more than twice the chance of suffering from these pathologies [9,18,21]. Therefore, we may say that the patients who are candidates to the bariatric surgery are more psychopathologic vulnerable than the general population [9].
It is also interesting to observe data regarding the increasing of weight. Another study conducted in this area revealed that 57% of the patients began to put up weight in childhood/ adolescence [22], and not in adulthood, as it was shown in our analysis. This data suggests that young adults may not be receiving the necessary investments in education, and there may be no sociologic conditions and structure to promote a healthy lifestyle, both from the physical and psychological points of view, to prevent such deleterious epidemic.
When comparing both genders, obese women who are candidates to bariatric surgery present levels of anxiety and BED superior to men, but the same results were not found for depression. However, if we compare the results for depression to the general population in Portugal, we may say that women are more prone to depression than men [23]. Furthermore, other studies have also found that the prevalence of obese women suffering from neuroses and depression is higher than in obese men [2,7,24 -27]. Such results may evoke some questions: Can obesity and the behaviours associated to it have a protective component to combat depression in obese women in the north of Portugal? Do obese women wish to be socially accepted and, therefore, fake personal difficulties to obtain the approval of the others and be considered apt to the surgery?
Finally, previous studies conducted in this population have shown that patients present a bias of vulnerability, a risk for self-injurious behaviour and a syndromic recurrence between the 4th and 9th years after surgery [9]. Such characteristics and the results from the present study would reinforce the need of having a group of specialists in mental health throughout the whole pre and post-surgery process.
Conclusion
The present study presented a general characterization of patients from north Portugal who were candidates to undergo bariatric surgery and concluded that the psychosocial construct of obesity, especially for the Portuguese population, needs to be further investigated in its multiple dimensions, bearing in mind that psychological and behavioural conditions affect obesity significantly. We suggest further investigations should prospectively analyse the patients who present more severe psychopathologic indicators; and analyse the post-surgical outcome and, if possible, correlate them with the psychosocial characteristics to create a predictive prognostic model.
Acknowledgement
The authors manifest their acknoledgement to all the individuals and institutions that were fundamental to this study; Unity of Psychiatry and Helath Psychology; Psychiatry and Mental Health Service; Multidisciplinary group to Surgical Treatment of Obesity; and Porto Hospital (Portugal).
References
- World Health Organization. Methodology and summary Country profiles on nutrition, physical activity and obesity in the 53 WHO European Region Member States.
- Lopes A, Telles Correia D (2016) Depressão, Obesidade e Cirurgia Bariá Psicológos. 14(2): 64-75.
- Alosaimi F (2012) Psychosocial aspects of overweight and obesity. European Psychiatry. 27(1): 741.
- Cunningham J, Merrell C, Sarr M (2012) Investigation of Antidepressant Medication Usage after Bariatric Surgery. Obes Surg 22: 530-535.
- Gonçalves S, Silva D, Antunes H (2012) Psychosocial correlates of overweight and obesity in infancy. Journal of Human Growth and Development 22(2): 179-186.
- Almeida SS, Zanatta DP, Rezende FF (2012) Imagem corporal, ansiedade e depressão em pacientes obesos submetidos à cirurgia bariá Estudos de Psicologia 17(1): 153-160.
- Almeida G, Giampietro H, Belarmino L, Moretti L, Marchini J, et al. (2011) Aspectos psicossociais em cirurgia bariátrica: a associação entre variáveis emocionais, trabalho, relacionamentos e peso corporal. ABCD, arq bras cir dig 24 (3): 226-231.
- Faith MS, Butryn M, Wadden TA, Fabricatore A, Nguyen AM, et al. (2011) Evidence for prospective associations among depression and obesity in population based studies. Obes Rev 12: 438-453.
- Herpertz S, Kessler H, Jongen S (2017) Psychosomatic and Psychosocial Questiond regarding Bariatric Surgery: What do we Know, or What do we Think We Know? Z Psychosom Med Psychother 63: 344-367.
- Dobrow IJ, Kamenetz C, Devlin MJ (2002) Aspectos psiquiátricos da obesidade. Revista Brasileira de Psiquiatria 24(3): 63-67.
- Franques ARM, Ascencio RFR (2006) Depressão e obesidade. In: ARM Franques and MSA Loli (Orgs.), Contribuições da psicologia na cirurgia da obesidade, Vetor, São Paulo, Brazil: pp. 125-135.
- Moliner J, Rabuske M (2008) Fatores biopsicossociais envolvidos na decisão de realização da cirurgia bariá Psicologia: Teoria e Prática 10(2): 44-60.
- Paes da Silva M, Jorge Z, Domingues A, Lacerda N, Chambel P, et al. (2006) Obesidade e Qualidade de Vida. Acta Med Port 19: 247-250.
- Sousa P, Bastos AP, Venâncio C, Vaz AR, Brandão I, et al. (2014) Compreender a Sintomatologia Depressiva após a Cirurgia Bariátrica: o Papel do Peso, da Alimentação e da Imagem Corporal. Acta Med Port 27(4): 450-457.
- Direcção Geral de Saúde (2012) Boas práticas na abordagem do doente com obesidade elegível para cirurgia bariá Orientação Nº 028/2012.
- Tapadinhas AR, Pais Ribeiro J (2008) Ingestão Compulsiva e Gestão das Emoções na Obesidade. In: I Leal, J Pais Ribeiro, I Silva, S Marques (Edts.). Actas do 7º congresso nacional de psicologia da saúde, ISPA, Lisboa, Portugal, p.85-88.
- Pais Ribeiro J, Silva I, Ferreira T, Martins A, Meneses R, et al. (2007) Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol Health Med 12(2): 225-235; quiz 235-237.
- Rocha C, Costa E (2012) Aspectos psicológicos na obesidade mórbida: Avaliação dos níveis de ansiedade, depressão e do auto-conceito em obesos que vão ser submetidos à cirurgia bariá Análise Psicológica 4: 451-466.
- Juan A Guisado, Francisco J Vaz, Javier Alarcón, Agustín Béjar, Mariano Casado, et al. (2002) Psicopatologia en pacientes com obesidad mórbida poscirugía gá Revista Cubana de Endocrinologia 13(1): 29-34.
- Direcção Geral de Saúde (2014) Depressão e outras Perturbações Mentais Comuns. Enquadramento Global e Nacional e Referencia de Recurso em Casos Emergentes. Saúde Mental em números, Portugal.
- Vinícius Lins Costa Melo, Paula Januzzi Serra, Cristiane de Freitas Cunha (2010) Childhood obesity – psychosocial impacts. Rev Med Minas Gerais 20(3): 367-370.
- Horta AC (2017) Fatores de início e manutenção da obesidade/excesso de peso: uma comparação entre adultos co binge eating e sem binge eating. Tese de Mestrado. Instituto Universitário de Ciencias Psicologicas, Sociais e da Vida, Portugal.
- Depression and other Common Mental Disorders. (2017) Global Health Estimates, WHO.
- Istvan J, Zavela K, Weidner G (1992) Body weight and psychological distress in NHANES Int J Obes Relat Metab Disord 16: 999-1003.
- Faith MS, Matz PE, Jorge MA (2002) Obesity-depression associations in the population. J Psychosom Res (53): 935-942.
- Carpenter KM, Hasin DS, Allison DB, Faith MS (2000) Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: Results from a general population study. Am J Public Health 90: 251-257.
- Travado L, Pires R, Martins V, Ventura C, Cunha S (2004) Abordagem psicológica da obesidade mórbida: Caracterização e apresentação do protocolo de avaliação psicoló Análise psicológica XXII(3): 533-550.






























