Burden of parents with Children Diagnosed with Pervasive Developmental Disorders and Behavioural Disorders [BD]
Bekos Vassilis *
Hellenic University of Patras, Greece, National Organisation Providing Health Services (EOPYY), Greece
Submission: October 02, 2017; Published: October 26, 2017
*Corresponding author: Bekos Vassilis, Hellenic University of Patras, Greece, National Organisation Providing Health Services (EOPYY), Greece, Email: mttheoria3@gmail.com
How to cite this article: Bekos Vassilis. Burden of parents with Children Diagnosed with Pervasive Developmental Disorders and Behavioural Disorders [BD]. Psychol Behav Sci Int J. 2017; 7(2): 555710. DOI: 10.19080/PBSIJ.2017.07.555710
Abstract
Theoretical Background: Research indicates that the presence of one or more children with developmental and behavioral disorders increase the psychological burden of parents
Purpose/Objective: The objective of this study is the investigation of the burden of parents with children with Pervasive Developmental Disorders [PDD] and Behavioural Disorders [BD] who come to Children's Mental Health Centers and Advisory Stations.
Materials and Methods: 104 parents [either mother or father] of children of both sexes suffering from Pervasive Developmental Disorder [PDD] took part in the research, and an additional 25 parents [either mother or father] of children of both sexes with Behavioral Disorders [BD] also participated. The questionnaire was used for the data collection was the Zarit Burden Interview.
Results: More specifically it is statistically borderline evident and important (p=0,057) that mothers on average (11, 74±5, 00) experience the intensity of the care-giving role more profoundly as opposed to the men (9, 93±6, 03). Additionally, it is statistically significantly evident (p=0,007) that mothers on average (8, 41±4, 00) experience the relationship deprivation more profoundly than their male counterparts (6, 39±4, 24). Also, it is statistically significantly evident (p=0,036) have on average (39, 05±16, 54) a higher total care giving coping burden in relation to men (33, 07±18, 84).
Conclusion: Parents with children that suffer either from pervasive developmental disorders or behavioral disorders, experience a psychological burden. Parents with children that suffer either from pervasive developmental disorders have higher psychological burden than parents with children with behavioral disorders. Mainly it is noteworthy that mothers are burdened more than fathers.
Keywords: Psychological Burden, Parents of children with pervasive developmental disorders, Parents of children with behavioral disorders
Introduction
Child care with autism spectrum disorders and behavioral disorders has increased significantly in recent years, with a higher incidence rate in boys (85.9%) Chakrabarti [1]. This increase is probably due to the fact that it is possible to diagnose, develop and make available services, to raise public awareness, but not to exclude other factors Elsabbagh et al. [2], Fombonne [3]. These children's speech problems White [4], which increases the difficulty of communicating with the social environment, and their desire for communication, results in provocative behavior Chiang [5]. Due to their lack of social skills, they are more likely to experience symptoms of depression, anger, suicidal ideation, provocative behavior Green et al. [6], low self-esteem and anxiety, making their adaptation difficult Lake et al. [7]; Kim et al. [8]. At the same time, according to the National Collaborating Center for Mental Health (UK) (2013), behavioral disorders seen in childhood and adolescence at the global level are now seen as the most common mental health disorders in children and adolescents.
Most common cause of referral to similar mental health services as s early as 1987, Kazdin identifies anti-social behavior in children as a predominant and serious clinical problem. Many children have symptoms of social isolation Bauminger et al. [9], reduced academic performance and progress at school, attention deficit disorder, hyperactivity, which in adolescence are manifested with symptoms of delinquency and antisocial behavior Reid et al. [10], McGilloway [11] On the other hand, research shows that the presence of one or more children with disorders is psychologically burdened by parents Taylor- Richardson [12], Myers [13] report that the autistic child's parents experience the constant anxiety and the burden of uninterrupted care and supervision together with provocative behaviors, social isolation, struggle for school and lack of respite, resulting in the calm of the family is disturbed. According to Weiss [14], the family's internal capabilities, members' needs, external resources and subjective assessments often lead to a crisis. At the same time, Gona [15] note that the challenges that parents face, regardless of their cultural or religious background, are stigma, financial burden, lack of proper treatment, and especially the burden of care, which affects them their mental wellbeing.
Moreover, the psychological burden of parents whose children experience emotional and behavioral disorders, anxiety about their child's condition, fatigue, depression, as well as the burden of their physical health adversely affect their social interactions, relationships with Meltzer [16] and their efficiency in their work Rosenzweig [17,18] This burden can often come from either the occurring incidents, such as inconvenience to peers and neighbors, police intervention, interruption of employment, financial pressure, disturbed family relationships, or emotions they feel like anger, stigma, guilt, sadness, entrapment and anxiety [19]. In this research study, an effort is being made to investigate the burden of parents of children with diffuse developmental disturbances (DRFs) and behavioral disturbances (ADs) coming to Centers and Counseling Centers of Child and Mental Hygiene, as well as exploring the social and demographic characteristics of parents and children.
Materials and Methods
The survey was conducted at a Child Psychotherapeutic Center, at a Child Psychiatric Center and at a Day Center, which serve as centers for prevention, diagnosis, treatment, counseling support aimed at rehabilitating disorders of children and adolescents and their psychosocial support and who receive incidents from all over the country West Greece. In the survey, 104 parents (either mother or father), children of both sexes with Pervasive Developmental Disorder (PDD) and 25 parents (either mother or father), children of both sexes with Behavioral Disorders Counseling and Child Psychiatric Centers in their quest to tackle the problem. Completion of the questionnaire was carried out with the help of a professional while the parents were in the waiting room and the specialist was alone with the child.
The data collection process took place over a period of 7 months, from October 2016 to April 2017. For the collection of data, the Zarit Burden Interview Zarit [20] was used. The Zarit Burden Interview measurement scale 1987 was designed to assess the burden of American caregivers of dementia patients. According to Zarit [20], the burden of carers refers to their physical health, psychological well-being, economic factors, their social life and their relationship with the family member they take care of. It was translated into Greek and weighed to Greek Cypriot caregivers with dementia by [21] and according to the results of their study constitutes a valid and reliable tool for anyone who would like to use it in the Greek population. According to the questions (a total of 22) the dimensions of the burden of care are: personal tension, the intensity of the role, the deprivation of relationships and the care of the care. During the completion of the questionnaire, clarifications were requested from the parents where they were given. The time to complete the questionnaire given to the parents was about 5-10 minutes
Results and Demographics
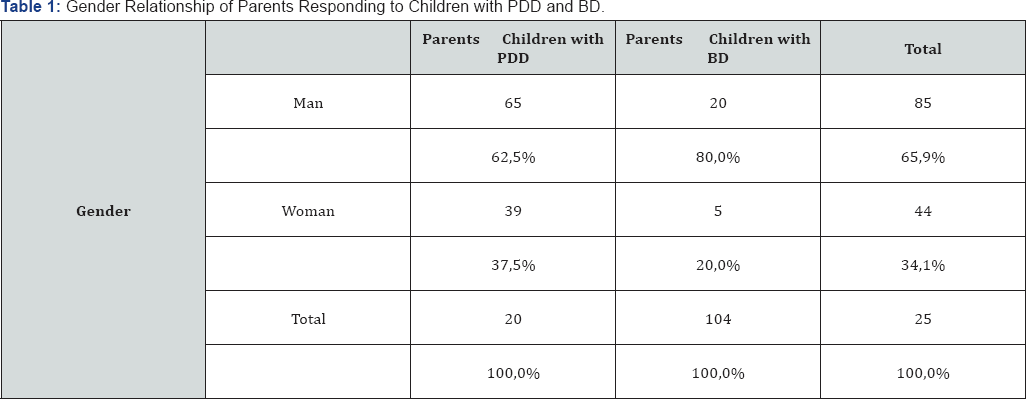
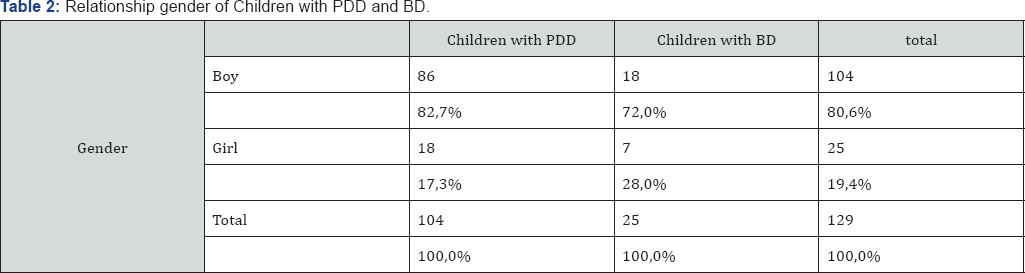
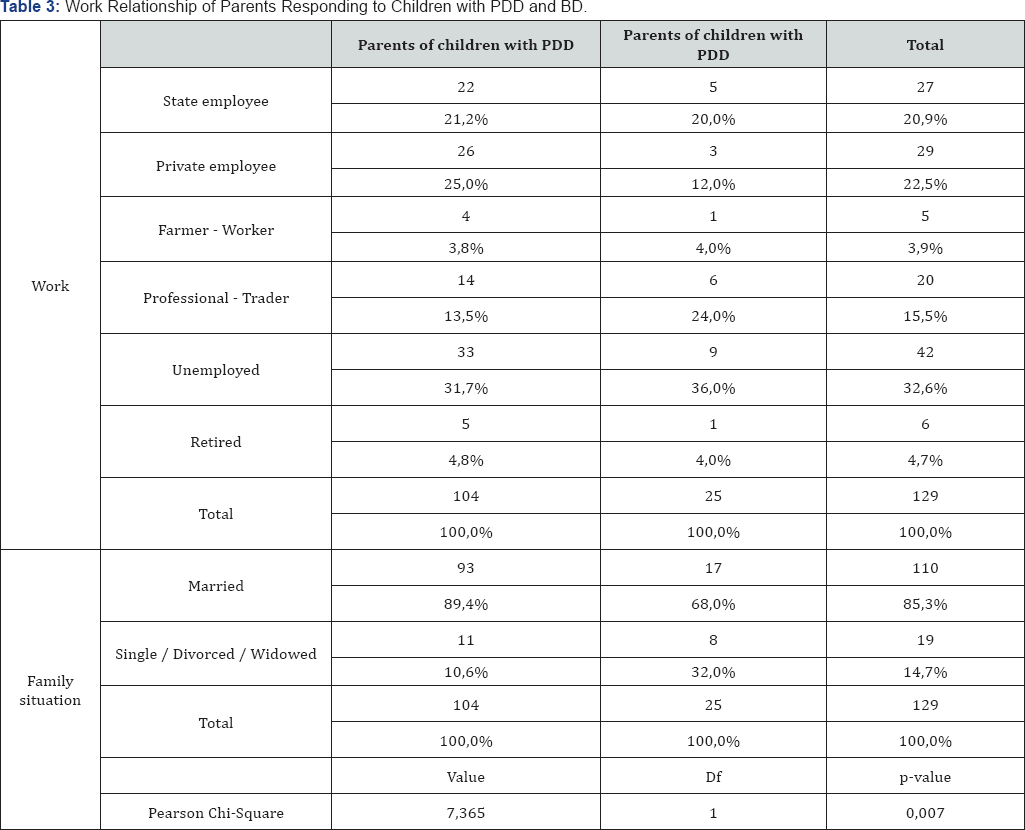
A higher percentage (62.5%) of both fathers of children with PDD compared to mothers and fathers (80.0%) of children with BD compared to mothers participated in our research (Table 1). Of the children in the study, PDD boys were in a higher percentage (82.7%) than girls with PDD and boys with a higher percentage (72.0%) than boys with AD (Table 2). Parents of children with PDD 89.4% declare married to parents of children with BD who declare married to 68.9%. The difference observed is statistically significant (x2 = 7.365; p = 0.007) (Table 3).
Results of burden Interview of Parents
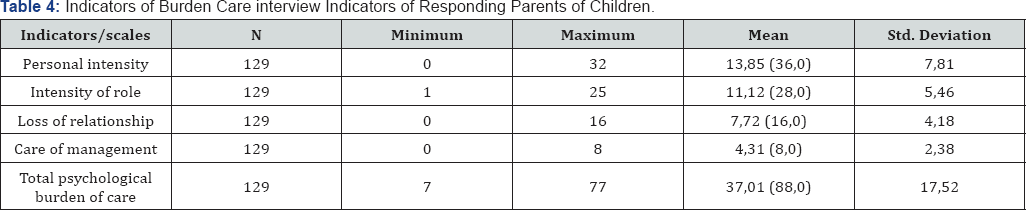
The personal intensity of the interviewed parents in total ranged from 0 to 32 with an average of 13.85 ± 7.81 showing a minimal to moderate burden (see the corresponding tables with the price levels of all the indicators) (Table 4). The intensity of the role of the interviewed parents overall ranged from 1 to 25 with an average of 11.12 ± 5.46 showing a modest burden (Table 4). The deprivation of the interviewed parents' relationships in total ranged from 0 to 16 with an average of 7.72 ± 4.18 showing a moderate to severe burden (Table 4). The management of the care of the interviewed parents overall ranged from 0 to 8 with an average of 4.31 ± 2.38, which also shows a moderate to severe burden (Table 4). Finally, the total psychological burden of care for respondents in parentheses ranged from 7 to 77, averaging 37.01 ± 17.52, showing a modest burden (Table 4).
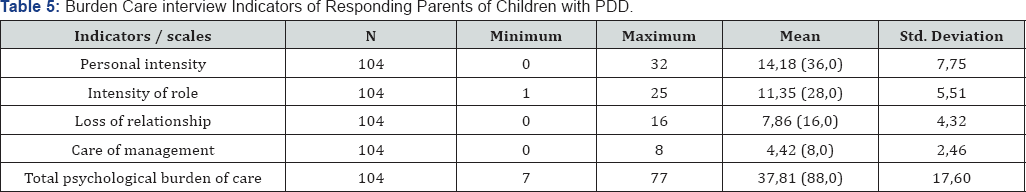

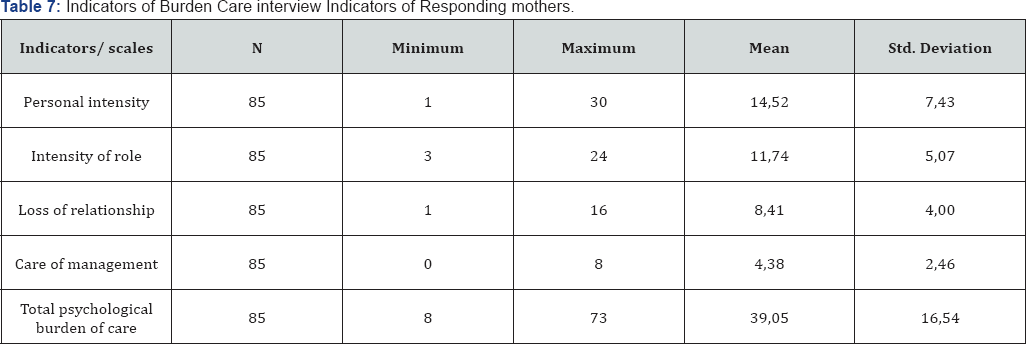
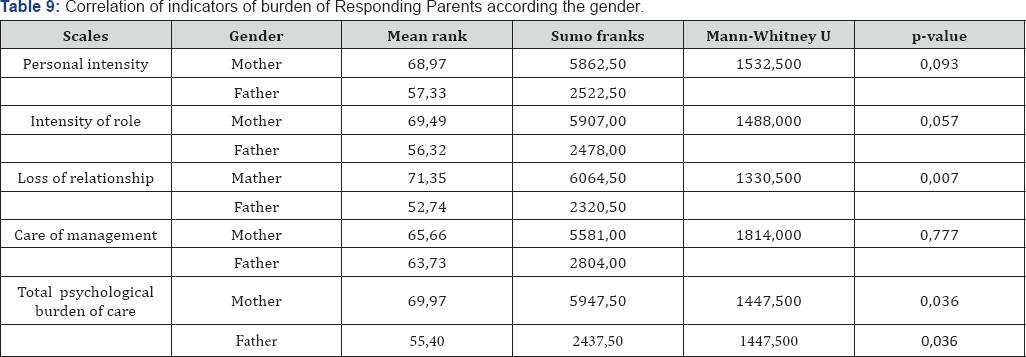
In Tables 5 & 6 it is obviously that all the indicators- dimensions of burden of parents of children with BDD are higher than that of the parents interviewed of children with BD. By checking the indicators of the gender-based Parental Care Questionnaire for parents of parents, we found that: The personal intensity of the mothers interviewed was 14.52 ± 7.43 (Table 7), higher than that of the fathers interviewed, which was 12.57 ± 8.43 (Table 8) without the difference being observed statistically significant (U = 1532, 500; p = 0,093) (Table 9). Similarly, the management of the care of the mothers interviewed was 4.38 ± 2.46 (Table 7), higher than the same indicator of the fathers interviewed, which was 4.18 ± 2.24 (Table 8) without the difference being observed statistically significant (U = 1814, 000; p = 0.777) (Table 9). In contrast, the intensity of the role of the mothers interviewed was 11.74 ± 5.00 (Table 7), higher than the intensity of the interviewed fathers, which was 9.93 ± 6.03 (Table 8). The difference observed is marginal statistically significant (U = 1488, 000; p = 0.057) (Table 9). The deprivation of mothers' relationships was 8.41 ± 4.00 (Table 7), much higher than the same index of fathers interviewed, which was 6.39 ± 4.24 (Table 8). The difference observed is statistically very significant (U = 1330, 500; p = 0,007) (Table 9). Finally, the total maternal care burden was 39.05 ± 16.54 (Table 7), much higher than the same index of fathers interviewed, which was 33.07 ± 18.84 (Table 8). The difference observed here is statistically significant (U = 1447, 500; p = 0,036) (Table 9).

Discussion
This study involved 129 parents (father or mother) of children with Diffuse Developmental Disorders and Behavioral Disorders. Of the 104 parents of children with PDD, 65 were fathers and 39 were mothers. Of the 25 parents with children with a BD, 20 were fathers and 4 mothers. It is characteristic that the child was accompanied by the father (65.9%) to the Child Psychotherapy-Hygiene Center, compared with the mother (34%) of the total. Regarding professional employment, it is characteristic that 32.6% of the total are unemployed, with a higher percentage of 36.0% being the parents of children with Behavioral Disorders. A study by Costello [22] states that children from very poor families were more at risk of developing comorbidities of emotional and behavioral disorders. Typically, Gatsa [23] report on the child's aggressive schooling and psychological well-being that the father's unemployment was of particular significance on the part of the victim. In a similar study, children of long-term unemployed parents, along with Christoffersen [24] are isolated at school, their psychosomatic balance is disturbed, they have low self-esteem and school performance, or they may even fall victim to intimidation. It is a fact that there is a burden on families with socio-economic problems. At the same time, similar study findings indicate that child behavioral disorders (difficulty of adaptation, aggression, substance use) are also observed in families with financial comfort and social background Luthar, Ansary [25] Luthar, Latendresse [26] due to limited bibliography.
Of course, it is worth noting that only 4.7% of the parents were farmers or workers, which deserves to be explored more in terms of accessibility from rural areas to similar diagnostic, support and treatment centers. At the same time, in Table 2 it appears that among the children involved in the study, the PDD boys were in a higher percentage (82.7%) than the girls with PDD Chakrabarti [1], as boys with a higher percentage (72.0%) against boys with BD. On the other hand, as regards the marital status, the difference is observed statistically significant (x2 = 7,365; p = 0,007), where 89,4 parents of children with PDD were married compared to parents of children with BD declared married only 68,9%. Possible behavioral disorders when there are no developmental disorders, which are necessarily inherent, are related to the particular marital status divorce, single parent family Magpantay [27]; Van Roy [28] reports that relationships in the family are an important factor in children's problem behaviors. Relevant studies have shown that ongoing conflicts and disputes between spouses as well as divorce as a fact affect children's behaviors Krishna kumar [29], resulting in difficulties in adapting, substance abuse behavioral problems and performance at school, but and behavioral and emotional disorders Amato and Cheadle [30].
With regard to the total psychological burden of care for respondents, the total number ranged from 7 to 77, with an average of 37.01 ± 17.52 showing a modest burden (Table 4). Of course, the deprivation of relationships and the management of the care of the interviewed parents overall ranged from 0 to 16 with an average of 7.72 ± 4.18 and from 0 to 8 with an average of 4.31 ± 2.38 respectively, showing a moderate to severe burden Ankri [31] (Table 4). Regarding the total psychological burden of care of the respondents parents of children with PDD was 37, 81 ± 17, 60 (Table 5), higher than the same index of respondents parents of children with BD that was 33, 68 ± 17, 15 (Table 6) Cadman 1996. More specifically, the findings of this research show that, in general, all indicators of burden care are higher in mothers than in fathers. In particular, it seems marginal statistically significant (p=0.057) that mothers on average (11.74 ± 5.00) experience the role of the role higher than fathers (9.93 ± 6.03). Also, it is statistically very important (p = 0.007) that mothers on average (8.41 ± 4.00) experience the deprivation of relationships also higher than men (6.39 ± 4.24). In addition, it is particularly statistically significant (p = 0.036) that mothers have a higher average (39.05 ± 16.54) total psychological care over men (33.07 ± 18.84) (Table 8).
The results ofthis study show a continuity with corresponding studies Fombonne [3], Robinson [32], Herring [33], Karst Van Hecke [34], Meirsschaut [35] demonstrating the mental burden that parents feel confronted with the challenges of caring for their children with pervasive developmental disorders and behavioral disorders. In a relevant research, Stuart, McGrew [36] report that the severity of the symptoms of the disorder Meltzer [16], the accumulation of additional requirements to deal with the condition Gallacher [37] and passive management strategies increase parents' load. Regarding the mental burden of mothers in this study, which was found to be higher than fathers, according to the dimensions of the psychological burden of Zarit [20] it appears that the mothers surveyed feel mainly pressure, anger, Gray [38], Joosten [39]concern that they are locked up, that they do not have personal time for themselves, that they are lagging behind in their work, in their relationships with other family members Meirsschaut [36] and their friends, feel blocked and generally overburdened emotionally due to care.
Conclusion
To a lesser degree they feel depression, weakness, fatigue, despair, negative feelings or guilt because they feel they are not offering what they should be to their child Woodgate [40]; Meirsschaut [36]; Ludlow [21]. In a similar study, Allik [41] reported that the burden of maternal health was greater than that of fathers, especially when behavioral and hyperactivity problems coexisted. Due to the increased care, Dumas [42] found that mothers, compared to fathers, children with autism and behavioral disorders felt more discomfort and depression Davis [43]. In addition, Little [44] found that mothers were more likely to experience high psychosomatic fatigue, had more stress, were pessimistic, had antidepressant treatment and visited specialists. Regarding the dimension of the derailment of relationships that the mothers of the study show higher, Ooi [45], Myers [13] report that mothers of autistic children, in order to take care of the child, were forced to leave work Meirsschaut [36] due to the particularities of their child's inability to work, and to abandon any career opportunities, have limited their job capacity, or have significantly modified their hours. They feel weak and trapped in controlling the behavior of their «normal child» in the social and family environment, feel anger, sadness and frustration and mistrust [46-48].
References
- Chakrabarti S, Fombonne E (2005) Pervasive developmental disorders in preschool children: Confirmation of high prevalence. The American journal of psychiatry 162(6): 1133-1141.
- Elsabbagh M, Divan G, Koh YJ, Kim Y S, Kauchali S, et al. (2012) Global Prevalence of Autism and Other Pervasive Developmental Disorders. Autism Research 5(3):160-179.
- Fombonne E (2008) Epidemiology of Pervasive Developmental Disorders. Pediatric Research 65(6): 591-598.
- Zarit S, Zarit JM (1987) The memory and behavior problems checklist and the burden interview (technical report). University Park, Pennsylvania State University.
- Chiang H (2008) Expressive communication of children with autism: The use of challenging behaviour. Journal of Intellectual Disability Research 52(11): 966-972.
- Green J, Gilchrist A, Burton D, Cox A (2000) Social and psychiatric functioning in adolescents with Asperger syndrome compared with conduct disorder. Journal of autism and developmental disorders 30(4): 279-293.
- Lake KJ, Perry A Lunsky Y (2014) Mental Health Services for Individuals with High Functioning Autism Spectrum Disorder. Autism Research and Treatment 502420: 9
- Kim JA, Szatmari P, Bryson S E, Streiner DL, Wilson F J (2000) The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism 4(2): 117-132.
- Brannan AM Heflinger CA (2006) Caregiver, child, family, and service system contributors to caregiver strain in two child mental health service systems. The journal of behavioral health services & research 33(4): 408-422.
- Reid R, Gonzalez JE, Nordness, PD Trout, Epstein M H (2004) A meta-analysis of the academic status of students with emotional/behavioral disturbance. Journal of Special Education 38(3): 130 -143.
- Mc Gilloway S, Mhaille GN, Bywater T, Furlong M, Leckey Y, et al. (2012) A parenting intervention for childhood behavioural problems: A randomized controlled trial in disadvantaged community-based settings. Journal of Consulting and Clinical Psychology 80(1): 116-127.
- Taylor-Richardson KD, Heflinger CA, Brown TN (2006) Experience of strain among types of caregivers responsible for children with serious emotional and behavioral disorders. Journal of Emotional and Behavioral Disorders 14(3): 157-168.
- Myers BJ, Mackintosh VH, Goin-Kochel RP (2008) My greatest joy and my greatest heart ache: Parents' own words on how having a child in the autism spectrum has affected their lives and their families' lives. Research in Autism Spectrum Disorders 3(3): 670-684.
- Wilson TD, Schooler JW (1991) �x00AB;Thinking too much: Introspection can reduce the quality of preferences and decisions*. Journal of Personality and Social Psychology 60(2): 181-192.
- Gigerenzer G, Todd P, ABC Group (1999) Simple Heuristics that make us smart. Oxford University Press, New York, USA.
- Menger C (1963) Investigations into the method of the social sciences with Special Reference to Economics. New York University Press, New York, USA.
- Rosenzweig JM, Brennan EM, Ogilvie AM (2002) Work-family fit: Voices of parents of children with emotional and behavioral disorders. Social Work 47(4): 415-424.
- Bauminger N (2003) Peer interaction and loneliness in high-functioning children with autism. Journal of Autism and Developmental Disorders 33(5): 489-507.
- Herring S, Gray K, Taffe J, Tonge B, Sweeney D, et al. (2006) Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: associations with parental mental health and family functioning. Journal of intellectual disability research 50(12) 874-882.
- Zarit S, Zarit JM (1987) The memory and behavior problems checklist and the burden interview (technical report). University Park, Pennsylvania State University.
- Ludlow A, Skelly C Rohleder P (2012) Challenges faced by parents of children diagnosed with autism spectrum disorder. Journal of health psychology 17(5): 702-711.
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, et al. (1996) The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of general psychiatry 53(12): 1129-1136.
- Gatsas T, Maglaras K, Bellos S, Damigos D, Maureas B, et al. (2015) Socio-demographic correlations of school aggression and effects on the psychosocial health of adolescent pupils Archives. Hellenic Medicine 32 (2): 182-193.
- Christoffersen NM (2000) Growing up with unemployment: a study of parental unemployment and children's risk of abuse and neglect based on national longitudinal 1973 birth cohorts in Denmark. Childhood 7(4): 421-438.
- Luthar SS, Ansary NS (2005) Dimensions of adolescent rebellion: Risks for academic failure among high- and low-income youth. Development and Psychopathology 17(1): 231-250.
- Luthar SS, Latendresse SJ (2005) Children of the Affluent: Challenges to Well-Being. Current Directions in Psychological Science 14(1): 4953.
- Magpantay MJ, Malabrigo P, Malijan RJ, Mazarin MG (2014) Behavioral Problems and Coping Strategies of Selected Adolescents Belonging to a Broken Family. CAM Research Journal 2(1): 112-135.
- Van Roy B, Groholt B, Heyerdahl S, Clench-Aas J (2010) Understanding discrepancies in parent-child reporting of emotional and behavioural problems: Effects of relational and socio-demographic factors. Psychiatry 10: 56.
- Krishnakumar A, Cheryl B (2000) Interparental Conflict and Parenting Behaviors: A Meta-Analytic Review. Family Relations 49(1): 25-44.
- Amato RP, Cheadle EJ (2008) Parental Divorce, Marital Conflict and Children's behavior Problems: A Comparison of Adopted and Biological Children. Social Forces 86 (3): 1139-1161.
- Ankri J, Andrieu S, Beaufils B, Grand A, Henrard JC (2005) Beyond the global score of the Zarit Burden Interview: useful dimensions for clinicians. International journal of geriatric psychiatry 20(3): 254260.
- Robinson S, Weiss JA, Lunsky Y, Ouellette-Kuntz H (2016) Informal Support and Burden among Parents of Adults with Intellectual and/or Developmental Disabilities. Journal of Applied Research in Intellectual Disabilities 29(4): 356-365.
- Herring S, Gray K, Taffe J, Tonge B, Sweeney D, et al. (2006) Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: associations with parental mental health and family functioning. Journal of intellectual disability research 50(12) 874-882.
- Karst SJ, Van Hecke AV (2012) Parent and Family impact of Autism Spectrum Disorders: A Review and Proposed Model for Intervention Evaluation. Clinical Child and Family Psychology Review 15(3):247- 277.
- Meirsschaut M, Roeyers H, Warreyn P (2010) Parenting in families with a child with autism spectrum disorder and a typically developing child: mothers' experiences and cognitions. Research in Autism Spectrum Disorders 4(4): 661-669.
- StuartM, McGrew HJ (2009) Caregiver burden after receiving a diagnosis of an autism spectrum disorder. Research in Autism Spectrum Disorders 3(1): 86-97.
- Gallagher S, Phillips AC, Carroll D (2010) Parental stress is associated with poor sleep quality in parents caring for children with developmental disabilities. Journal of pediatric psychology 35(7): 728-37.
- Gray DE (2003) Gender and coping: The parents of children with high functioning autism. Social Science and Medicine 56(3) 631-642.
- Joosten AV, Safe AP (2014) Management strategies of mothers of school-age children with autism: implications for practice. Australian occupational therapy journal 61(4): 249-258.
- Woodgate RL, Ateah C, Secco L (2008) Living in a world of our own: the experience of parents who have a child with autism. Qualitative health research 18(8): 1075-1083.
- Allik H, Larson JO Smedje H (2006) Health-related quality of life of parents of school-age children with Asperger syndrome or high functioning autism. Health & Quality of Life Outcomes 4(1): 1-8.
- Dumas EJ, Wolf CL Fisman NS, Culligan A (1991) Parenting stress, child behavior problems, and dysphoria in parents of children with autism, down syndrome, behavior disorders, and normal development. Exceptionality 2(2): 97-110.
- Davis NO, Carter AS (2008) Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: associations with child characteristics. Journal of autism and developmental disorders 38(7): 1278-1291.
- Little L (2002) Differences in stress and coping for mothers and fathers of children with Asperger's syndrome and nonverbal learning disorders. Pediatric nursing, 28(6): 565-570.
- Ooi KL, Ong YS, Jacob SA, Khan TM (2016) A meta-synthesis on parenting a child with autism. Neuropsychiatric Disease and Treatment 12:745-762.
- Brennan EM, Rosenzweig JM, Ogilvie AM, Wuest, Shindo AA, et al. (2007) Employed parents of children with mental health disorders: Achieving work-family fit, flexibility, and role quality. Families in Society 88(1): 115-123.
- Fombonne E, Simmons H, Ford, T, Meltzer H, Goodman R (2001) Prevalence of pervasive developmental disorders in the British nationwide survey of child mental health. Journal of the American Academy of Child and Adolescent Psychiatry 40(7): 820-827.
- Gona JK, Newton CR, Rimba KK, Mapenzi R, Kihara M, et al. (2016) Challenges and coping strategies of parents of children with autism on the Kenyan coast. Rural and remote health journal 16(2): 3517.






























