Hyperbaric Oxygen Therapy for Traumatic Brain Injury in an Iraq War Veteran
Sohail R Daulat1*, Nikhil Dholaria2, Raymond H Cralle3, Joseph Maroon1, Jeffrey M Gran4, Charles Scherer5, Sheldon F Gottlieb6, Tom Fox7 and William S Maxfield8
1 Department of Neurosurgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA
2 University of Arizona College of Medicine - Phoenix, Phoenix, Arizona, USA
3 Oxygen Rescue Care Centers of America, Delray Beach, Florida, USA
4 Private Practice Neuropsychology, Broward County, Florida, USA
5 Delray Medical Center, Delray Beach, FL, USA
6 Consulting Firm, Boynton Beach, Florida, USA
7 Private Practice, Pincourt, Quebec, Canada
8 Private Radiology Consultant, Odessa, FL, USA
Submission:August 06, 2025;Published: August 12, 2025
*Corresponding author: Sohail R Daulat, Department of Neurosurgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA
How to cite this article: Hassan Abuali, Ibrahim Fagiri, Jasmijn de Grebber and Anil Reddy.Atypical Testicular Mass: An Uncommon Manifestation of 005 Gastrointestinal Neuroendocrine Tumor. Open Access J Surg. 2025; 16(4): 555945. DOI: 10.19080/OAJS.2025.16.555945.
How to cite this article: Hassan Abuali, Ibrahim Fagiri, Jasmijn de Grebber and Anil Reddy.Atypical Testicular Mass: An Uncommon Manifestation of 005 Gastrointestinal Neuroendocrine Tumor. Open Access J Surg. 2025; 16(4): 555945.DOI: 10.19080/OAJS.2025.16.555945.
Abstract
Traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD) caused by repeated blast injuries are prevalent conditions affecting veterans of the Iraq and Afghanistan conflicts. While hyperbaric oxygen therapy (HBOT) has shown promise in alleviating symptoms of TBI/PTSD, few studies have evaluated its long-term effects using both neuroimaging and cognitive assessments. This case study documents what occurred to one veteran diagnosed with post-traumatic stress disorder (PTSD) after multiple blast exposures. The patient had attempted suicide and was receiving treatment with psychotropic medications. After 40 hyperbaric oxygen therapy treatments (HBOT) and comprehensive physical therapy, the comparison of pre- and post-treatment neuropsychological tests and single-emission photon computed tomography (SPECT) brain scans demonstrated significant improvement in neurocognitive function, motor skills, mental state and quality of life. In this patient, HBOT was successful in alleviating TBI/PTSD symptoms by repairing brain damage sustained from blast injury without any adverse effects. SPECT brain imaging documented brain abnormalities prior to HBOT and objectively confirmed the response to HBOT and physical therapy. HBOT may benefit TBI/PTSD patients by reducing or eliminating the confusion and side effects associated with complex pharmacologic regimens.
Keywords: Blast exposure, Hyperbaric Treatment, Post Traumatic Stress Disorder, Traumatic Brain Injury, Military
Abbreviations: TBI: Traumatic Brain Injury; PTSD: Post-Traumatic Stress Disorder; HBOT: Hyperbaric Oxygen Therapy; SPECT: Single-Emission Photon Computed Tomography; IED: Improvised Explosive Device; ATA: Atmospheres Absolute; CT: Computed Tomography; EEG: Electroencephalography; MRI: Magnetic Resonance Imaging; NAB: Neuropsychological Assessment Battery; PRBT: Potentially Recoverable Brain Tissue; IN: Idling Neurons
Background
Many servicemen returning from Afghanistan and Iraq experienced a traumatic brain injury (TBI) during deployment. By 2008, approximately 300,000 of the 1.64 million troops deployed to Iraq or Afghanistan were suffering from mild TBI/post-traumatic stress disorder (PTSD) or depression [1]. Furthermore, 88% of military personnel treated at an echelon II medical unit in Iraq had been injured by an improvised explosive device (IED) or mortar, with 47% of injuries involving head trauma [2]. Some of the resulting neuropsychological problems caused by blast exposure are now categorized as PTSD, the symptoms of which mimic those of TBI [3]. These complex and co-occurring injuries contribute to a rising mental health burden and may partially explain the alarming increase in suicide rates observed among U.S. veterans [4,5].
Neurologic symptoms associated with TBI vary in severity, appear randomly, and may be triggered by events years after the initial injury [6]. In the case of blast-related injuries, the effects can be profound even without direct head trauma. As shown in animal studies, isolated torso exposure to IED blasts can still result in significant brain injury [7]. Explosive blasts can cause TBI by the barotrauma of the blast or through coup/contrecoup injuries, causing diffuse axonal damage in individual neural cells [8-11]. Due to the complexity and often delayed presentation of blast-induced brain injury, further investigation needs to be conducted on therapeutic approaches that go beyond symptomatic relief and directly target the underlying pathophysiology [12-14].
Hyperbaric oxygen therapy (HBOT), which delivers 100% oxygen in a pressurized environment, is increasingly being explored as an intervention for physical and neurological conditions. Multiple case series, randomized trials, and individual case reports describe improvements in headache frequency, cognitive function, mood disturbances, and post-traumatic stress disorder (PTSD) symptoms following HBOT, with treatment protocols often involving 30-40 sessions at 1.5-2 atmospheres absolute (ATA) [15-17]. Some studies have also used techniques such as SPECT or MRI to document neurobiological changes in brain perfusion and metabolism before and after HBOT [17,18] However, limited studies have investigated longitudinal, multimodal evaluations, such as combining SPECT neuroimaging and neurocognitive testing. This case report tracks sustained functional recovery across cognitive, emotional, and physiological domains, while offering visual and psychometric evidence of brain tissue reactivation. The patient has lasting improvements in cognitive function, emotional well-being, and physical health, supported by both neuroimaging and standardized testing.
Case Description
History and presentation
A 22-year-old male army veteran who served in Operation Iraqi Freedom between August 2006 and July 2007, with daily duties of route clearance as part of a Quick Reaction Force team, experienced approximately 40 IED blasts. He presented with daily headaches and seizures during the last 2 or 3 IED blast exposures and was medically evacuated to Landstuhl Regional Medical Center, Germany in August 2007 for further examination. On admission, he experienced 2 additional seizures. There was no family history of epilepsy and computed tomography (CT) of the brain was negative for bleeding, shift, and fracture. Electroencephalography (EEG) and magnetic resonance imaging (MRI) results were within normal limits and further evaluation revealed major depressive disorder, PTSD, pseudoseizure disorder, conversion disorder, and tinnitus. The final suspected diagnosis was mild TBI, and additional follow-up with neurology and behavioral health practitioners was recommended.The patient’s VA records documented 9 pseudoseizures within one month of returning to the United States. In September 2007, he experienced auditory hallucinations and headaches that started at the back center of his head and radiated to the right to left frontal lobes. One practitioner opined that the daily headaches were likely caused by prior analgesic misuse. The patient’s records also indicated that he had memory problems, photophobia, phonophobia, osmophobia, and irritability. He did not receive a follow-up MRI, EEG, or CT. The patient subsequently saw a psychiatrist, attended therapy sessions, and was prescribed various combinations of medications, including a period in which he received 7 drugs simultaneously. Medications included trazodone, venlafaxine, risperidone, quetiapine, sertraline, citalopram, eszopiclone, zolpidem, clonazepam, fluoxetine, amitriptyline, lorazepam, prazosin, propranolol, and promethazine.
In October 2007, he spent 12 days in a psychiatric hospital for extremely violent behavior after experiencing auditory hallucinations, homicidal ideation, and blackouts. In December 2007, he was institutionalized for 7 days after attempting suicide by ingesting 60 mg of trazodone and 8 mg of risperidone. He was subsequently diagnosed with conversion disorder, convulsions, and alcohol abuse. In 2008, he experienced 2 to 5 pseudoseizures per week, headaches, anxiety, and upper body spasms. In February 2009, the patient was medically discharged with a 70% disability rating. He began drinking heavily and joined a voluntary alcohol rehabilitation program. When first seen at our facility in October 2009, the patient had PTSD, depression, post-traumatic nightmares 4 times per week, memory problems, high levels of frustration, painful, frequent headaches, and balance difficulties. His medications were venlafaxine, risperidone, mirtazapine, and topiramate. Neuropsychological evaluations included the Medical Symptom Validity Test, State-Trait Anxiety Inventory, Beck Depression Inventory-II, PTSD Checklist-Civilian Version, Neuropsychological Assessment Battery (NAB) Form 2 (attention, language, spatial, memory, and executive modules), and Personality Assessment Inventory. Initial testing with the NAB showed average or better range scores for all modules, whereas his other test scores indicated impaired psychological functioning.
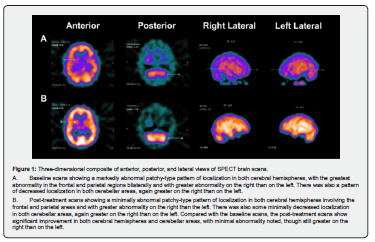
Technetium-99m single-photon emission computed tomography (SPECT) brain scans (29.4 mCi) were obtained to document perfusion and metabolism brain abnormalities. The patient had abnormal SPECT brain scans at his initial evaluation (Figure 1A). The scans showed marked abnormalities in the frontal and parietal regions and in cerebellar areas, with greater abnormalities on the right side, in areas responsible for the visual-spatial abilities that allow individuals to navigate through both familiar and unfamiliar environments. Basal ganglia showed significantly decreased localization, and all areas of abnormal localization had peri-ischemic penumbra. Mild ventriculomegaly was also noted. Abnormal SPECT images correlated with the patient’s decreased functional capacity measured in the psychiatric and physical evaluations.
Treatment
Treatment consisted of 40 sessions of hyperbaric oxygen exposure at 1.75 to 2 atmospheres absolute (ATA), delivered for 90-minutes, twice a day, 5 times per week, with 3 to 4 hours between exposures. Aggressive physical therapy, including vestibular stimulation for balance disorders and electrical stimulation and manual therapy for muscle and joint pain, was provided. No additional medications were prescribed.

Post-treatment evaluation and follow-up
Compared with baseline test results, neuropsychological evaluation at completion of treatment demonstrated significant improvements in depression, anxiety, and PTSD symptoms, including absence of nightmares and increased memory function (Tables 1 & 2). Significant improvements were also found in language function. Attention, spatial, and executive functioning were roughly equivalent to baseline.
Post-treatment SPECT brain scans revealed improvement in the cerebral cortex and cerebellar areas (Figure 1B). Areas of abnormality in the frontal and parietal regions were again greater on the right than the left. There was minimal decreased localization in the cerebellar area, again, with abnormalities greater on the right. Basal ganglia showed minimal abnormality with minimal-to-moderately decreased localization. All areas of abnormal localization continued to show peri-ischemic penumbra. The SPECT scans also suggested that although the ischemic penumbra was diminished, there were some areas of potentially recoverable brain tissue (PRBT), which were defined as viable but metabolically lethargic and electrically non-functional.
The patient reported feeling less depressed, more energetic, and had an improved appetite with fewer and less painful headaches. The patient’s mother noted significant improvements in mood, sleeping patterns, conversational skills, memory function, and level of alertness. Within 2 months of treatment completion, he enrolled in a local college. By the end of the semester, he had earned a 3.6 G.P.A. He had also stopped taking any prescription medications. The patient’s post-treatment scores relative to pre-treatment scores were significantly better for measures of depression, PTSD, anxiety, attention, language and memory. At the 10-month follow-up, he scored significantly better relative to post-treatment scores for measures of depression, PTSD, anxiety, and spatial function (Tables 1 and 2). His 10-month NAB Language module score was equivalent to baseline and post-treatment scores, and while the decrease in the NAB Memory module score was not significantly different, it was significantly better than at baseline Figure 1.
Discussion
Only a few studies have investigated HBOT’s effects in patients with neuropsychiatric complexity and functional impairment. This case report combined quantitative neurocognitive testing, reported outcomes, and pre/post-treatment SPECT imaging, which displayed cerebral perfusion improvements and their alignment with cognitive, emotional, and behavioral gains. Moreover, the stopping of all psychotropic medications, return to academic function, and restoration of daily life activities reflect clinical recovery and true reintegration. Successful treatment of TBI is complicated by compromised cognitive abilities. If a patient can neither focus on physical or mental tasks during therapy nor retain information and remember to take prescribed medications, progress toward wellness can be extremely challenging. Traditional treatment approaches to TBI address each symptom separately: various medications are used to treat sleep disorders, depression, emotional issues, and pain [19-21] Psychotherapy is used to address emotional problems, and physical therapy is applied to recover motor skills. In addition to enduring associated adverse effects, patients must follow complicated and usually ineffective regimens and can become increasingly frustrated.
The pathophysiology of TBI-induced brain injury involves the volume of the infarct (umbra) in the region of brain injury and a variable volume of peri-infarcted tissue of diminished blood flow (ischemic penumbra) where a differential sensitivity of brain tissue function exists based on oxygen availability [8,10,11,22,23]. In hypoxia, the critical oxygen tension (PC O2) is the partial pressure of oxygen (PO2) at which oxygen consumption (VO2) is below the normoxic control. In penumbral areas where the blood flow is below 10-15 mL/100 g brain tissue, neurons and possibly glial cells enter an idling state [22,24] “Idling neurons” (IN) in the ischemic penumbra are viable but show decreased metabolism and no electrical activity [24]. IN are difficult to detect by standard neurological techniques because they behave as if they are non-viable, yet they represent PRBT, or areas that can be reactivated by increased oxygen availability [24] Comparison of pre- and post-HBOT SPECT scans provide tangible evidence of PRBT and can be used to follow the course of therapy and help identify end points of therapy [24-27]. The patient’s SPECT scans were consistent with the presence of PRBT, its diminution with HBOT, and its positive correlation with psychological, cognitive and physical improvements after therapy. The post-treatment scans also showed residual PRBT and thus the potential for further recovery with continued treatment.
Unlike symptom-focused treatment strategies for TBI, which may not address the underlying pathological processes of cerebral neuronal and glial injury, HBOT offers a myriad of physiological, cellular, and biochemical effects, and targets the source of the impairment by facilitating the reactivation and repair of neurons and glia through improved oxygenation and blood flow in the brain [24-26,28]. This case emphasizes the potential for HBOT as a method of recovery for patients who have TBI and PTSD but have not seen beneficial results in standard psychiatric and neurologic interventions. These findings reveal the potential usage of HBOT earlier in the treatment course for patients with TBI and PTSD. Future research should prioritize analyzing integrative methodologies to optimize patient selection and therapeutic monitoring.
References
- Costin Simona, Dumitrascu Dan (2008) The neuroendocrine tumors of the ileum. Open Medicine 3(2): 135-140.
- Heimann David (2015) Primary Neuroendocrine Tumor (Carcinoid Tumor) of the Testis: A Case Report with Review of Literature. American Journal of Case Reports 16: 328-332
- Cai Wen, Tan Yinuo, Ge Weiting, Ding Kefeng, Hu Hanguang (2018) Pattern and risk factors for distant metastases in gastrointestinal neuroendocrine neoplasms: a population‐based study. Cancer Medicine 7(6): 2699-2709.
- Ahmed Monjur (2020) Gastrointestinal neuroendocrine tumors in 2020. World Journal of Gastrointestinal Oncology 12(8): 791-807.
- Amine Mseddi M, Mohamed Bouzguenda, Mourad Hadjslimane, Majed Hamza, Slim Charfi, et al. (2017) Neuroendocrine Testicular Tumors: A Systematic Review and Meta-Analysis. Current Urology 10(1): 15-25.
- Juhlin Carl Christofer, Zedenius Jan, Höög Anders (2020) Clinical Routine Application of the Second-generation Neuroendocrine Markers ISL1, INSM1, and Secretagogin in Neuroendocrine Neoplasia: Staining Outcomes and Potential Clues for Determining Tumor Origin. Endocrine Pathology 31(4): 401-410.
- Uri Inbal, Grozinsky-Glasberg Simona (2018) Current treatment strategies for patients with advanced gastroenteropancreatic neuroendocrine tumors (GEP-NETs). Clinical Diabetes and Endocrinology 4(1): 16.
- Chan Doris T, Luk Andrea OY, So WY, Kong Alice PS, Chow Francis CC, et al. (2016) Natural history and outcome in chinese patients with gastroenteropancreatic neuroendocrine tumours: - a 17-year retrospective analysis. BMC Endocrine Disorders 16(1): 12.
- Singh Simron, Moody Lesley, Chan, David L, Metz David C, Strosberg Jonathan, et al. (2018) Follow-up Recommendations for Completely Resected Gastroenteropancreatic Neuroendocrine Tumors. JAMA Oncology 4(11): 1597-1604.






























