Atypical Testicular Mass: An Uncommon Manifestation of Gastrointestinal Neuroendocrine Tumor
Hassan Abuali*, Ibrahim Fagiri, Jasmijn de Grebber and Anil Reddy
Department of Colrectal surgery, James Cook University Hospital, Middlebrough, UK
Submission:June 18, 2025;Published:June 26, 2025
*Corresponding author: Hassan Abuali, Department of Colrectal surgery, James Cook University Hospital, Middlebrough, UK.
How to cite this article: Hassan Abuali, Ibrahim Fagiri, Jasmijn de Grebber and Anil Reddy.Atypical Testicular Mass: An Uncommon Manifestation of 005 Gastrointestinal Neuroendocrine Tumor. Open Access J Surg. 2025; 16(4): 555944. DOI: 10.19080/OAJS.2025.16.555944.
Abstract
Neuroendocrine tumors (NETs) are rare neoplasms that most commonly originate in the gastrointestinal (GI) tract, with the liver, lymph nodes, bone, and lung as frequent metastatic sites. Testicular metastasis from a GI NET is exceptionally uncommon, accounting for less than 1% of all testicular cancers and only 6.82% of testicular NETs. Here, we present a case of a 68-year-old male with a painful testicular mass, normal tumor markers, and eventual diagnosis of a well-differentiated NET with primary involvement of the terminal ileum, plus liver and testicular metastases. This case emphasizes the importance of considering metastatic NETs in atypical testicular masses and highlights the critical role of imaging, histopathology, and multidisciplinary management.
Neuroendocrine Tumor; Colonoscopy; Laparoscopic; Gastrointestinal Surgery; Hemicolectomy; Testicular Cancer
Abbreviations: NETs: Neuroendocrine Tumors; GI: Gastrointestinal; AFP: Alpha-Fetoprotein; β-HCG: Beta-Human Chorionic Gonadotropin; CT: Computed Tomography; MDT: Multidisciplinary Team
Background
Neuroendocrine tumors (NETs) are rare neoplasms arising from the diffuse neuroendocrine system, most commonly affecting the gastrointestinal tract. Metastasis to the testis is exceptionally rare, presenting unique diagnostic and management challenges. NETs most frequently originate in the gastrointestinal tract (74%) and less commonly in the bronchopulmonary system (25%). They can occur in various sites including the ovary, gallbladder, extrahepatic bile ducts, thymus, testis, liver, cervix, spleen, and breast [1,2]. Gastrointestinal neuroendocrine tumors (GI NETs) most commonly metastasize to the liver, which accounts for the majority of secondary sites, followed by lymph nodes, bone, lung, and brain Metastasis to the testis is extremely rare, with few reported cases in the literature, highlighting its unusual presentation compared to common sites. This case report examines a rare case of a small bowel NET with metastasis to the testicle and liver, initially presenting as a testicular lesion, thereby underscoring the critical importance of comprehensive diagnostic evaluation [3,4].
Case Presentation
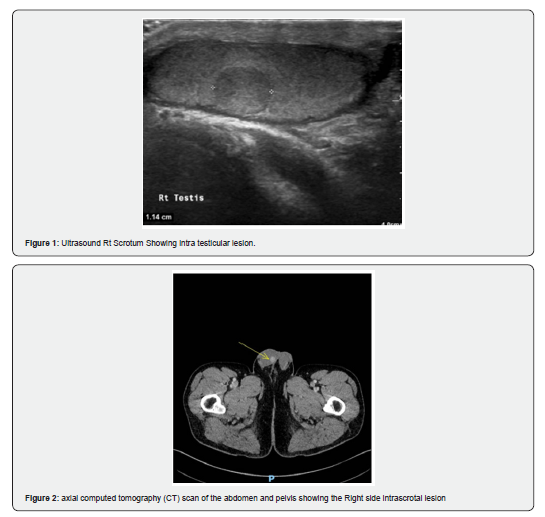
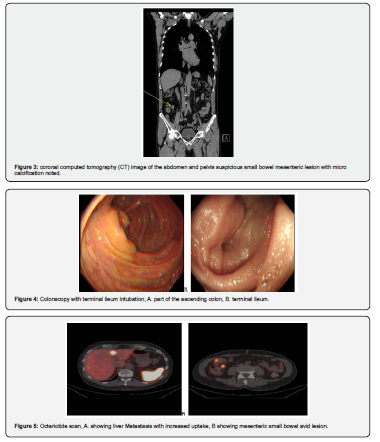
This case involves a 68-year-old Caucasian male who presented with a one-month history of a painful right testicular lump to his general practitioner. The absence of recent trauma or past genitourinary pathology, combined with a negative family history, made the clinical scenario particularly challenging. Initial diagnostic assessment included scrotal ultrasound, which identified a focal intratesticular lesion highly suspicious for malignancy. Despite these imaging findings, tumor markers-specifically alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (β-HCG)-were within normal limits. This discordance between imaging and biochemistry prompted a staging CT, which unexpectedly revealed a suspicious small bowel mesenteric lesion and a solitary liver lesion, raising the possibility of a neuroendocrine tumor (NET) with metastatic disease [5,6] (Figure 1-3).
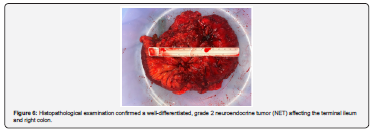
Subsequent histopathological analysis, following a right inguinal orchiectomy, demonstrated a well-differentiated neuroendocrine tumor, indicating testicular metastasis rather than a primary testicular neoplasm. Advanced diagnostic modalities were employed to localize the primary tumor. Colonoscopy, which included intubation of the terminal ileum up to 10 cm, revealed congested mucosa without a distinct mass, and tissue biopsies were ultimately non-diagnostic. An octreotide scan provided further clarity, demonstrating an avid lesion in the terminal ileum as well as mesenteric and hepatic metastatic involvement. Chromogranin A, a recognized biochemical marker of NETs, was notably elevated at 284 µg/L, while other blood tests remained unremarkable [7,8] (Figure 4-6).
The patient’s management was guided through a colorectal multidisciplinary team (MDT) meeting, where it was determined that surgical resection of the primary tumor was the most appropriate intervention. Accordingly, the patient underwent a laparoscopic right hemicolectomy with ileocolic anastomosis one week after the MDT’s recommendation. His postoperative course was without complications, leading to discharge on the fourth postoperative day. Five hepatic metastases were identified based on CT AP and octreotide scan, but these were considered unresectable within the MDT discussion. As a result, the patient was referred to oncology for commencement of somatostatin analogue therapy as part of ongoing systemic management [9].
Discussion
Gastrointestinal neuroendocrine tumors (GI NETs) are uncommon neoplasms that may initially present with nonspecific symptoms, making diagnosis especially complex in cases of atypical metastatic spread. The liver is by far the most frequent site of metastasis for these tumors, followed by lymph nodes, bone, lung, and, much more rarely, the testis. The incidence of secondary testicular neuroendocrine tumors (TNETs) arising from gastrointestinal (GI) organs is very low. In a comprehensive review incorporating published cases and case series spanning several decades, a total of 132 cases of testicular neuroendocrine tumors were identified. Of these, secondary TNETs-meaning tumors that originated elsewhere and subsequently metastasized to the testis-accounted for only 9 out of 132 cases, representing 6.82% of all TNETs. Significantly, the GI tract was the most common primary site among secondary TNETs: out of the nine secondary cases, eight (88.89%) originated from gastrointestinal neuroendocrine tumors, such as those located in the ileum or cecum.
To put this into perspective, TNETs account for less than 1% of all testicular neoplasms or testicular cancers, the vast majority (76.52%) of TNETs were primary and pure, and another 16.67% were associated with teratomas rather than representing true secondary involvement from a distant organ. Therefore, the likelihood of a testicular neuroendocrine tumor being secondary and originating from a GI tract tumor is quite rare in both absolute and relative terms. In this case, the lack of elevation of conventional testicular tumor markers (AFP, β-HCG) helped prompt further investigation, and advanced imaging modalities-such as staging CT and octreotide scintigraphy-proved essential for accurate localization and characterization of the primary and metastatic lesions. Histopathological examination remains crucial for establishing the diagnosis, with immunohistochemical positivity for neuroendocrine markers such as chromogranin A being standard diagnostic criteria¹⁰.The markedly elevated chromogranin A level in this patient was a key biochemical clue consistent with known NET presentations.
The testicular involvement in this patient's disease process underscores the importance of considering metastatic NETs in the differential diagnosis of testicular masses, particularly in older patients or when standard germ cell tumor markers are not supportive of a primary gonadal neoplasm. The literature notes that testicular metastasis may signal widespread disease, given these tumors' tendency to follow vascular and lymphatic dissemination pathways. The management of GI NETs is inherently multidisciplinary. Surgical resection remains the cornerstone of therapy for localized tumors and in select patients with limited metastatic burden, as supported by this patient’s successful right hemicolectomy and orchiectomy. However, for unresectable metastatic disease, as seen with the liver metastases in this patient, systemic therapy with somatostatin analogues such as octreotide or lanreotide is recommended to control symptoms and possibly slow tumor progression.
It is notable that the natural course and prognosis of NETs are influenced not only by the site of origin but also by tumor grade and proliferation index, as evidenced by the well-differentiated, grade 2 histology here. Long-term follow-up is mandated given the risk for delayed recurrences; the literature documents NET metastases developing many years after initial therapy. The favorable postoperative course and good short-term prognosis of this patient highlight the benefits of tailored, stage- and grade-appropriate management, while ongoing surveillance and systemic therapy are required due to residual metastatic disease.
In conclusion, this case underscores the rarity of testicular metastases from GI NETs, the necessity of thorough diagnostic evaluation for atypical testicular lesions, and the importance of a collaborative, multidisciplinary approach for optimal treatment and follow-up.
References
- Costin Simona, Dumitrascu Dan (2008) The neuroendocrine tumors of the ileum. Open Medicine 3(2): 135-140.
- Heimann David (2015) Primary Neuroendocrine Tumor (Carcinoid Tumor) of the Testis: A Case Report with Review of Literature. American Journal of Case Reports 16: 328-332
- Cai Wen, Tan Yinuo, Ge Weiting, Ding Kefeng, Hu Hanguang (2018) Pattern and risk factors for distant metastases in gastrointestinal neuroendocrine neoplasms: a population‐based study. Cancer Medicine 7(6): 2699-2709.
- Ahmed Monjur (2020) Gastrointestinal neuroendocrine tumors in 2020. World Journal of Gastrointestinal Oncology 12(8): 791-807.
- Amine Mseddi M, Mohamed Bouzguenda, Mourad Hadjslimane, Majed Hamza, Slim Charfi, et al. (2017) Neuroendocrine Testicular Tumors: A Systematic Review and Meta-Analysis. Current Urology 10(1): 15-25.
- Juhlin Carl Christofer, Zedenius Jan, Höög Anders (2020) Clinical Routine Application of the Second-generation Neuroendocrine Markers ISL1, INSM1, and Secretagogin in Neuroendocrine Neoplasia: Staining Outcomes and Potential Clues for Determining Tumor Origin. Endocrine Pathology 31(4): 401-410.
- Uri Inbal, Grozinsky-Glasberg Simona (2018) Current treatment strategies for patients with advanced gastroenteropancreatic neuroendocrine tumors (GEP-NETs). Clinical Diabetes and Endocrinology 4(1): 16.
- Chan Doris T, Luk Andrea OY, So WY, Kong Alice PS, Chow Francis CC, et al. (2016) Natural history and outcome in chinese patients with gastroenteropancreatic neuroendocrine tumours: - a 17-year retrospective analysis. BMC Endocrine Disorders 16(1): 12.
- Singh Simron, Moody Lesley, Chan, David L, Metz David C, Strosberg Jonathan, et al. (2018) Follow-up Recommendations for Completely Resected Gastroenteropancreatic Neuroendocrine Tumors. JAMA Oncology 4(11): 1597-1604.






























