Anterior Dentoalveolar Setback: Anticipated Incisor Inclinations
Ahmed A El Danaf1*, Heba A Eldanaf2, Manal A Mohsen3 and Ahmad A Rabie4
*1Emeritus Professor and Ex-Chief, Department of Plastic and Maxillofacial Surgery, Al Mataria Teaching Hospital, General Organization of Teaching Hospitalsss and Institutes (GOTHI), Cairo, Egypt.
2Lecturer and Researcher, Department of Restorative and Dental Materials, Oral and Dental Research Division, National Research Centre, Cairo, Egypt.
3Emeritus Professor, Department of Child Health, National Research Centre, Cairo, Egypt.
4Lecturer and Researcher, Department of Dermatology & Venereology, Institute of Medical Research and Clinical Studies, National Research Centre, Cairo, Egypt.
Submission: July 05, 2024; Published: August 12, 2024
*Corresponding author: Ahmed A El Danaf, Emeritus Professor and Ex-Chief, Department of Plastic and Maxillofacial surgeon, Al Mataria Teaching Hospital, General Organization of Teaching Hospitals and Institutes (GOTHI), Cairo, Egypt.
How to cite this article: El Danaf AA, Eldanaf HA, Mohsen MA, Rabie AA. Anterior Dentoalveolar Setback: Anticipated Incisor Inclinations. Open 006 Access J Surg. 2024; 15(4): 555920. DOI: 10.19080/OAJS.2024.15.555920.
Abstract
Background: Predicting results is crucial when it comes to planning. Some patients after anterior maxilla-mandible osteotomy may choose not to have postoperative radiographs, however mobilized distances and directions of incisor-canine segment are regularly recorded in operative reports.
Purpose: This retrospective study aimed to predict modifications in incisor orientation induced by the mobilization.
Material and Methods: Out of 33 patients who underwent surgical anterior dentoalveolar setback, eleven did not have a cephalometric study after the operation and one had it 17 years later. Mobilizations of the central incisor tip were marked on the preoperative cephalometric tracings to draw an anticipated postoperative orientation. The predictors included the preoperative incisor inclination, the setback distance and upward mobilized distance of the segment. The main outcome involved geometrically calculated postoperative upper incisor-Frankfurt plane and lower incisor-mandibular plane angles. Paired and one sample t-tests were used to analyse the variables. Multiple regression models were used to create probable ideal equations predicting postoperative incisor inclinations.
Results: Surgical results aesthetically and functionally satisfied patients. There was a highly significant reduction in inclination angles between the preoperative and the drawn postoperative inclination angles (P < 0.01) and the late cephalography of one patient supported the upper incisor aroused formula. The regression model equations were based on the predicted postoperative inclinations which were not significantly different from the normal standards (P > 0.05).
Conclusion: Despite the occasional lack of postoperative cephalometric radiographs, it is still possible to preoperatively anticipate and postoperatively evaluate changes in the incisor inclination.
Key words: Esthetics; Malocclusion; Orthognathic Surgical Procedures; Maxilla Osteotomy; Mandibular osteotomy; Incisor.
Introduction
Mobilization of the incisor-canine segment corrects anterior malocclusion, gummy smile, and facial profile, while the inclination of the incisors influences the beauty of the face. Changes in the orientation of the incisor axis along with mobilization distances are useful for studying stability and relapses after orthognathic surgeries. It is standard surgical care to obtain postoperative radiography to exclude artifacts like missed screws, hooks, and orthodontic brackets. Unfortunately, postoperative radiographs are occasionally missed for a variety of reasons. This study aimed to propose the employment of the segmental mobilization distances and preoperative incisor inclination for predicting the postoperative incisor axial orientation.
Materials and Methods
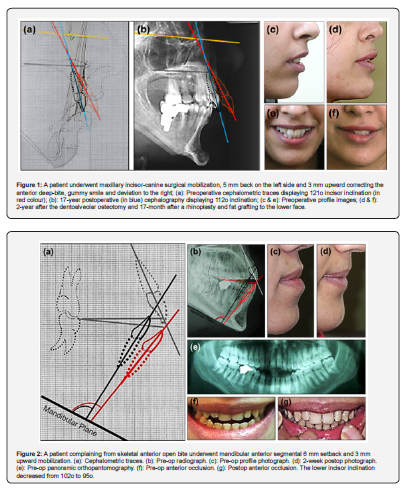
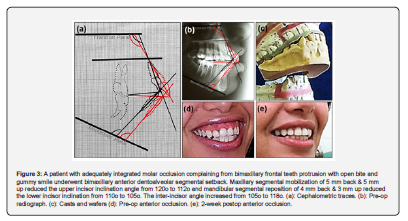
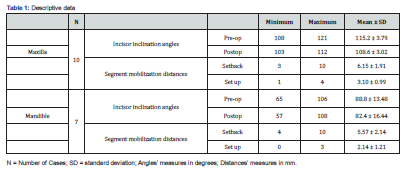
Out of 33 patients who underwent anterior dentoalveolar setback, twelve patients declined to undergo a cephalometric study after the operation, and one of the 12 had a 17-year postoperative cephalography. The sample included eleven female patients, and one male patient, with ages ranging from 18 to 47 years old. The segmental setback procedures, statistically considered as study covariates, were maxillary in ten cases (Figure 1) and mandibular in seven (Figure 2); five patients underwent a bimaxillary procedure (Figures 3). This cohort retrospective study was in accordance with a local Institutional Review Board guidance.
Surgical procedure
Ø Surgery was performed to correct over-projection of the incisor-canine segment and anterior malocclusion. Patients had acceptable functional posterior occlusion; therefore, a Le Fort I osteotomy was not considered the preferred treatment. The mobilization distances were planned in accordance with patient’s cosmetic demands, clinical assessment, amount of deviation from normal Sella-nasion point A and point B angles and mock surgical trials on casts. In maxillary cases, the distance of alveolar setback was largely influenced by the severity of the gummy smile and limited by the lower incisors position to avoid crossbite.
Ø Teeth extraction typically involves the first premolars on both sides to mobilize backward the segment. Two patients with anterior maxillary deviation had only one premolar extracted on the opposite side to simultaneously correct symmetry. In two others with already missing mandibular first premolars, bilateral second premolar extraction was chosen to afford the required space.
Ø In addition to preserving the adherence of the maxillary segment to an intact palatine muco-periosteum, a valuable vascular pedicle was maintained by keeping the attachment of the segment anterior muco-periosteum to the upper lip mucosa. This was achieved by substituting the surgically popular long transverse vestibular approach with three vertical incisions: one above the extracted premolar socket on each side and a smaller one in the midline, enough to perform shortening of the caudal border of the nasal septum giving room for upward mobilization of the segment. The width of the excised bone vertical strip in-line with the extracted teeth sockets did not exceed the planed posterior repositioning distance. Horizontal ostectomies were maid 4 mm away from the teeth apices to prevent dental vascular and neural injuries. Muscular attachments to the posterior surface of the mandibular segment were carefully preserved to maximally conserve its blood supply. Segments were repositioned after being completely freed. Inter-dental wiring temporarily stabilized the segment for adjusting the occlusion, and the final inter-osseous fixation was secured with miniplates and screws. Excised bony pieces were incarcerated as grafts in the residual skeletal gaps to promote rapid consolidation. Absorbable suture ensured watertight mucosal closure. Mouth washing, and hygiene started early after the operation. Inter-maxillary fixation provided comfort during the early postoperative days in bimaxillary cases.
Ø For aesthetic reasons, the segmental osteotomy was combined with osseous genioplasty in five cases, facial fat grafting in two cases, and rhinoplasty in one case. The average duration of the operation was four hours. Orthodontics was regularly advised for all patients.
Postoperative complications included
Ø A premolar crown with caries was constricted by excessive tightening of circum-dental wire. It was promptly cemented, and few weeks later endodontically treated to alleviate persisting sensitivity to cold fluids.
Ø A tracheostomy was indicated after anaesthetist’s recommendation in a patient with severe mandibular retrusion undergoing a combined mandibular anterior segmental setback, BSSO and chin advancements [1].
Ø Undiagnosed choanal atresia in another case prevented trans-nasal tracheal intubation and per-operative occlusion adjustments, forcing a revision surgery started by tracheostomy within 48 hours.
Ø A protruding bony spike in one case was noticed ten days after surgery and promptly removed under local anaesthesia in the clinic.
Sample, Predictors, geometrical tracing, and statistics
Ø The study included patients who underwent front dentoalveolar surgical mobilizations and refused the postoperative radiography. The predictors included the preoperative central incisors inclination angles (upper incisor-Frankfurt plane angle and lower incisor-mandibular plane angle), and the setback, and upwards mobilization distances of the incisor-canine segments. The independent variables were the age and sex of the patients. Segment mobilizations were traced on the preoperative cephalography, and the predicted inclination of the incisor was measured.
Ø Statistical analysis: The SPSS program (Statistical Package for the Social Sciences, Chicago, IL, USA) was utilized to calculate descriptive data including mean, minimum, and maximum. A paired t-test was employed to compare the preoperative and the geometrically drawn postoperative upper incisors' inclination, as well as the pre and postoperative lower incisors' inclination. Also, a one sample t-test was performed to compare the results against the normal standards, with an upper incisor-Frankfurt horizontal plane angle of 109 degrees and a lower incisor-mandibular plane angle of 93 degrees considered ideal. Multiple regression models were preformed to introduce the ideal equation model assessing the postoperative incisor inclinations. A good fit R-squared ranges between 0.50 and 0.99 and an adjusted R-square value from 0.5 to 0.7 were considered acceptable, especially when relations were significant. P- value of less than 0.05 was deemed statistically significant for all tests.
Results
Ø Follow up ranged from a few weeks to 6 years with a mean of 18 months when the patient with 17 years follow-up was excluded. Patients were satisfied with the improved facial profile, improved nice smile, and corrected anterior bite. By marking the backward and upward mobilization distances of the tip point of the central incisor on the preoperative lateral cephalometric tracings, the predicted change in the incisor’s axial orientation was drawn and measured.
Ø On average, a maxillary segment setback of 6 mm and an upward movement of 3 mm improved the axial angle of the upper incisors by approximately 7 degrees. A mandibular segment setback of 5 mm and an upward movement of 2 mm changed the inclination of the lower incisors by 6 degrees (Table 1).
Ø The main outcome variable was the geometrically calculated postoperative central incisor inclination angles. In both maxillary and mandibular anterior segmental osteotomy cases, there was a highly significant reduction in inclination angles between the preoperative and the drawn postoperative measurements (P<0.01). The postoperative inclinations were insignificantly different from the normal standard (P>0.05) that may support the accuracy of the methodology used. (Table 2).
Ø Mobilization distances and incisor inclination changes were further used to perform multiple regression models for finding out postoperative inclination ideal equations (Table 3):
· Postop upper incisor angle = (0.395 X pre-op inclination angle) + (1.370 X upward mobilized distance) - (0.443 X setback mobilized distance) + 61.521
· Postop lower incisor angle = (1.296 X pre-op inclination angle) + (0.409 X setback mobilized distance) - (2.820 X upward mobilized distance) - 28.984

The equation of the predicted upper incisor inclination was checked and mathematically validated after one of the 12 studied patients thankfully accepted to undergoing cephalography 17 years after surgery (Figure 1). Larger sample size studies with available pre and postoperative cephalometric analyses may further support the proposed formulas.
Discussion
Ø Forecasting postoperative axial incisor orientation may preoperatively provide an approximate anticipation of the planned anterior dentoalveolar mobilization results. The main contribution of the study was the assessment of changes in the orientation of anterior teeth when postoperative radiographs were not available. Calculations of the new incisor orientation were based on the distances of segmental mobilization reported during the operation and the preoperative cephalometric angular degrees of incisor inclination. While there may have been a small margin of human error in the drawings and angle readings, the statistical results aligned with common surgical expectations. The very late cephalography in one patient confirmed precision of the upper incisor developed equation. The small sample size of the study may be explained by the infrequency of patients’ refusal to undergo postoperative radiography and by the fact that it was a single-surgeon series. Surgical incisor-canine setback in low socio-economic income communities and private practice is not infrequently performed without an available preoperative cephalography. The described methodology may assist maxillofacial surgeons, orthodontists, and program designers.
Ø In the vast landscape of maxillofacial osteotomies, the challenging maxillary anterior segmental osteotomy was pioneered in the 1920s by G. Cohen-Stock and M. Wassmund, while the mandibular anterior segment osteotomy was reported three decades later by H Kole [2]. Reestablishing balanced symmetric positional and volumetric distribution among the three stages of the face is a common request in plastic and orthognathic surgery centres [3]. The axial position of the maxillary incisors, whether under- or over-jetting, has a significant impact on the smile and facial aesthetics [4]. According to Arnett et al. (1999), the centre of the maxillary first incisor should be vertically aligned with the wet-dry line of the upper lip, approximately in the same vertical plane as the forehead [5]. Recent advancements in three-dimensional cone-beam computed tomography have provided more precise orthognathic planning compared to traditional cephalometric assessments [6]. A multi-disciplinary team consisting of an orthodontist, restorative and operative dentists, along with a maxillofacial surgeon is essential for creating an appropriate plan, performing precise operations, and achieving optimal outcomes in orthognathic treatments [7]. Procedures such as anterior segmental osteotomy, genioplasty, and rhinoplasty play a significant role in harmonizing the facial profile [8]. By addressing cosmetic defects and malocclusion simultaneously, edging the central mandibular segment below the mental foramen along with other orthognathic procedures, can lead to a more aesthetically pleasant result [9,10]. [Image 1]
Author contributions
Author 1: Performed the surgical operations, contributed to conception, design, data acquisition and interpretation, drafted and critically revised the manuscript.
Author 2: Performed most of the dental work, contributed to conception, design, data acquisition and interpretation, drafted and critically revised the manuscript.
Author 3: Performed all statistical analyses, contributed to conception, design, data acquisition and interpretation, drafted, and critically revised the manuscript.
Author 4: Contributed to conception, design, and critically revised the manuscript.
All authors gave their final approval and agreed to be accountable for all aspects of the work.
References
- El Danaf A, Eldanaf H, Rabie A (2024) Mandibular retrusion six-piece contouring by combined anterior subapical setback, BSSO advancement, and two-step genioplasty. Oral Maxill of Surg Cases.
- Kole H (1959) Surgical operations on the alveolar ridge to correct occlusion abnormalities. Oral Surg Oral Med Oral Pathol Ppp: 515-529
- Bell R, Kiyak HA, Joodeph DR, McNeill RW, Wallen TR (1985) Perceptions of facial profile and their influence on the decision to undergo orthognathic surgery. Am J Orthdo 88: 323-332 Cited by: Ghandhi V, Malek F (2018) Orthognath Surg and Facial changes - are view. J Orthod Endod.
- Bou Assi S, Macari A, Hanna A, Tarabay R, Salameh Z (2020) Cephalometric evaluation of maxillary incisors inclination, facial, and growth axes in different vertical and sagittal patters: an original study. J Int Soc Prevent Communit Dent 10(3): 292-299.
- Arnett GW, Jelic JS, Kim J, Cummings DR, Beress A, et al. (1999) Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop 116(3): 239-253.
- Hija A, Allon DM (2022) Comparative assessment of perception about angle inclination of mandibular and maxillary incisors on the cephalometric analysis between skeletal Class 3 and orthognathic cases. Appl Sci 12(2): 6228.
- Cunningham SJ, Johal A (2015) Orthognathic correction of dentofacial discrepancies. Brit Dent J 218(3): 167-175.
- Hoenig J (2007) Sliding osteotomy genioplasty for facial aesthetic balance: 10 years of experience. Aesth Plast Surg 31(4): 384-391.
- Ho CT, Tai WK, Kao CT (2023) Simple treatment for beauty is not always the best: a corrective surgery. J Dent Sci 18(2): 898-900.
- Lee TY-H, Hung C-Y, Cheng JH-C, Fang C-Y (2023) The combination of mandibular Kole procedure and bilateral sagittal splitting in orthognathic surgery has positive effect in esthetics and function for short-throat-length skeletal class III patient. J Dent Sci 18(1): 479-481.






























