Long Term Paired Outcomes of Index and Redo Per Oral Endoscopic Myotomy
Lucie F Calderon1, Hima Veeramachaneni1, Natalie Roppolo2, Brittany Kile2, Hailey Canezaro2, Victoria Andrus2, Elizabeth Armstrong2, David Okuampa2, Ross Dies2, Ashely Deville2, Lena Kawji2, Julia Massaad1, Steve D Keilin1 and Qiang Cai1,2*
1Division of Digestive Diseases, Emory University School of Medicine, Atlanta, GA, USA
2Division of Gastroenterology and Hepatology, Louisiana State University Health Science Center at Shreveport, Shreveport, LA, USA
Submission: April 17, 2024; Published: May 01, 2024
*Corresponding author: Qiang Cai, Professor and Director, Division of Gastroenterology and Hepatology, Louisiana State University School of Medicine, Shreveport, LA, USA. Email: qiang.cai@lsuhs.edu
How to cite this article: Lucie F Calderon, Hima Veeramachaneni, Natalie Roppolo, Brittany Kile, Hailey Canezaro, Victoria Andrus, Elizabeth Armstrong, David Okuampa, Ross Dies, Ashely Deville, Lena Kawji, Julia Massaad1, Steve D Keilin and Qiang Cai*. Study of Efficacy and Early Post-Procedure Complications of Rubber Band Ligation for Controlling Bleeding in Second Degree Hemorrhoid at National Referral Hospital. Open Access J Surg. 2024; 15(3): 555912. DOI: 10.19080/OAJS.2024.15.555912.
Abstract
Introduction
Per-Oral Endoscopic Myotomy (POEM) is a specialized procedure designed to improve symptoms by minimizing lower esophageal sphincter pressure in patients with achalasia. Despite excellent reported success rates, about 10% of patients have persistent or recurrent symptoms after procedure. There are limited studies looking at the efficacy of redo POEMS for these patients. In particular, there is no published data on comparing the paired effect of index POEM and redo POEM individually. We aimed to compare paired data of index and redo POEMs and provide election criteria for redo POEM.
Methods
We conducted a retrospective observational study of all patients who underwent both index and redo POEM between August 2014 and January 2020 at Emory University. All patients underwent standard POEM protocol. We defined clinical success by an Eckardt score ≤3 post procedure. Results were analyzed with t tests, Chi squared tests where appropriate, or were otherwise reported as means with corresponding ranges.
Results
15 patients underwent redo POEM (ages 25-79, 53% female). One was lost to long-term follow up. There was no significant difference noted between index and redo POEM in procedure time (61.9 minutes vs. 62.2 minutes) (p=0.96), myotomy length (6.9 cm vs.6.1 cm) (p=0.13). 10 out of 15 patients (67%) achieved clinical success post-procedure with an Eckhardt score <3,
Conclusion
Redo POEM procedure can be safely performed even on the same side of index POEM. Patients with previous interventions, those who clinically failed index POEM (never-responders), and those who initial responded (recurred) all can benefit from and should be offered redo POEM procedure. However, patients with severely diffusely dilated esophagus may not benefit from redo POEM and warrant surgical consultation for esophagectomy, if necessary.
Keywords: POEM; Redo; outcome; Achalasia
Abbreviations: POEM: Per-Oral Endoscopic Myotomy; LES: Lower Esophageal Sphincter; FLIP: Functional Lumen Imagine Probe; NPO: Nil Per os; EGJ: Esophagogastric Junction; LOS: Length of Hospital Stay
Introduction
Achalasia is a rare esophageal motility disorder that is characterized by absent or defective peristalsis and poor relaxation of the lower esophageal sphincter (LES). Patients’ symptom burden lies mostly in their failure to swallow normally, often leading to gradually worsening dysphagia, regurgitation, chest pain, and eventually weight loss from the inability to eat. The loss of innervation of the inhibitory neurons in the LES creates unopposed cholinergic excitation and insufficient relaxation of the LES [1].
Treatment for achalasia aims to reduce LES pressure and better allow the passage of boluses of swallowed liquid and food. Therapeutic options include pneumatic dilatation and laparoscopic Heller myotomy. However, over the last decade, per-oral endoscopic myotomy (POEM) has emerged as a first line therapeutic motility, achieving the same effectiveness as Heller myotomy and even shown to have improved benefit in type III achalasia over traditional Heller myotomy due to the ability to extend the myotomy length [2-4]. Despite increasing popularity and published short- and mid-term clinical success of POEM, there is a small subset of patients who have persistent symptoms or develop recurrent symptoms after the procedure. A recent study reported that 9.8% of 441 patients who underwent POEM never experienced symptomatic relief [5]. This group of patients was then offered several salvage options, including pneumatic dilatation, Heller myotomy, and redo POEM, with the largest resolution of symptoms (63%) occurring in the group that underwent redo POEM compared to 20% and 45% with pneumatic dilatation and Heller myotomy, respectively [5].
Overall, limited studies have explored therapeutic options after failure of initial POEM. Select case series have commented on the feasibility and safety of redo POEM, but there is not yet enough evidence to establish repeat POEM as standard of practice [6,7]. The aim of this study is to evaluate the efficacy and safety of redo POEM as a salvage therapy in patients who have failed index POEM. Moreover, we aimed to observe the long term outcome of redo POEM and to compare index and redo POEM in each patient in order to identify which subsets of patients would likely receive the most benefit based on their presenting symptoms and their response to initial POEM. To our knowledge, this is the first report of paired comparisons of long term outcomes of index and redo POEM in each patient.
Methods
Study design, definitions, and statistical analysis
We conducted a retrospective observational study of patients with achalasia who underwent POEM at Emory University Hospital between August 2014 and January 2020. These patients were diagnosed with achalasia by high-resolution manometry as per Chicago Classification (v3), or in the case of inconclusive manometry, based on barium swallow and functional lumen imagine probe (EndoFLIP) with visualization of clinical features. Patients who met the following criteria were offered redo POEM: 1. Patients who had no response to index POEM; 2. Patients with symptoms recurred after index poem with Eckardt score >6. The medical records were reviewed for patient demographics, symptom scores, intraoperative techniques, and complications. The study was conducted with approval by the institutional review board, and patients’ consent was obtained prior to each procedure.
POEM protocol
The protocol for index and redo POEM were similar. All POEM procedures were performed at Emory University Hospital by advanced endoscopists (SK and QC) with participation of an advanced endoscopy fellow while under general anesthesia. All patients were instructed to be on a clear liquid diet for two days and nil per os (NPO) after midnight on the planned procedure day. Each patient was given prophylactic antibiotics during the procedure. Posterior myotomy at the 6 o’clock orientation was performed while patients were in supine position for all patients in their index POEM. For redo POEM, after an initial diagnostic upper endoscopy and identification of prior mucosotomy scar, redo mucosotomy was performed at the side of the scar if possible. The POEM procedure was started with a clear cap attached to the tip of the endoscope. Similar to index POEM, the new mucosotomy site was selected in mid esophagus approximately 10 cm proximal to the esophagogastric junction (EGJ). Using an I-type hybrid knife (ERBE USA Inc. Marietta, GA, USA), a mucosal incision and a submucosal bleb was created by injection of a solution of mixed normal saline with methylene blue and epinephrine. This was followed by a 1.5 cm mucosotomy. Then a submucosal tunnel was established by repeated injection and submucosal dissection. After creating an adequate tunnel and extending about 2 cm distal to EGJ, a selective myotomy of the circular muscle layer started distally beginning at about 1-2 cm distal to the EGJ and extending proximally to mid esophagus, approximately 2-3 cm distal to the mucosotomy site. The length of myotomy was dependent on the type of achalasia and the degree of difficulty of the procedure. Finally, the incision site was closed using endoscopic clips. Patients were observed in the hospital overnight and were discharged after tolerating a liquid diet.
Outcome measurements
The primary outcome was the clinical success of redo POEM in each patient. Clinical success was defined as a decrease of Eckardt score to less than or equal to 3. The Eckardt score is the sum of the symptom scores for dysphagia, regurgitation, and chest pain (0, absent; 1, occasional; 2, daily; and 3, each meal) and weight loss (0, no weight loss; 1,<5kg; 2,5–10kg; and 3,>10kg). Secondary outcomes included the paired comparisons of index and redo POEM through sub-analyses, including duration of symptom relief, those with previous interventions prior to index POEM, and initial vs never-responders (defined as patients who never achieved an Eckardt <3 after initial POEM). Safety outcomes were defined by the occurrence of peri-operative adverse events.
Statistical analysis
Continuous variables were reported as means ± standard deviation. Categorical variables were reported as percentages and paired t-test. Statistical analyses were performed using the t-test for quantitative variables and the Chi square test for categorical variables (or Fisher’s exact test where appropriate). A two tailed P-value of <0.05 was considered statistically significant.
Results
Subjects
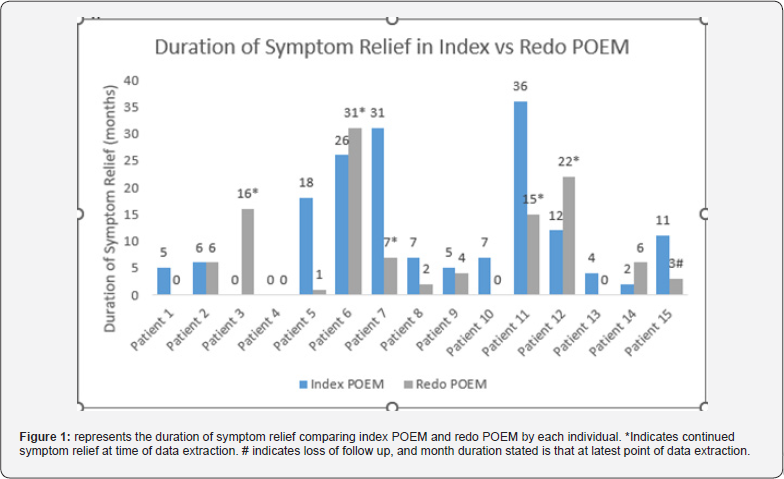
A total of 15 patients (mean age 49.4, range 25-79) met the selection criteria and underwent redo POEM between August 2014 and January 2020. All patients were followed up to 5 years after index POEM, with a minimum of 6 month follow up after redo POEM. (Table 1) summarizes demographic and clinical data of included patients in the study. (Table 3) also includes patients by type of achalasia, where “not specified” refers to those whose type of achalasia was not stated in the manometry or FLIP report. The median (range) interval after initial POEM was 13 months (1-55 months) prior to performing redo POEM. Following redo POEM, subjects were followed for a median (range) of 6 months (6-31 months). Four of the 15 (27%) patients had previously undergone alternative procedures for symptom relief prior to index POEM.


Procedure-related data
Technical success of redo POEM was achieved in all 15 patients (100%). As to the site of myotomy, 11 redo procedures were performed at the same orientation (posterior) from the middle esophagus to the GE junction, while four were performed at opposite sides. (Table 2) outlines procedure-related data from index and redo POEM. There was no difference between the index POEM and redo POEM groups in terms of procedure duration (61.9±21.1minutes vs 62.2±14.4 minutes, , p=0.98), number of clips used to close mucosotomy site (3.4 clips range 3-4 vs 3.6 clips range 3-8, p=0.07), myotomy length (6.9±1.1 cm vs 6.1± 1.6 cm, p=0.12), or length of hospital stay (LOS) (3.1±5.09 days vs 1.5±0.83 days, p=0.19). The myotomy length distal to the EGJ was shorter in the redo POEM compared to index POEM (1.1cm±1.2 vs 2cm±1, p=0.02).
Clinical Success and Long-term Follow up
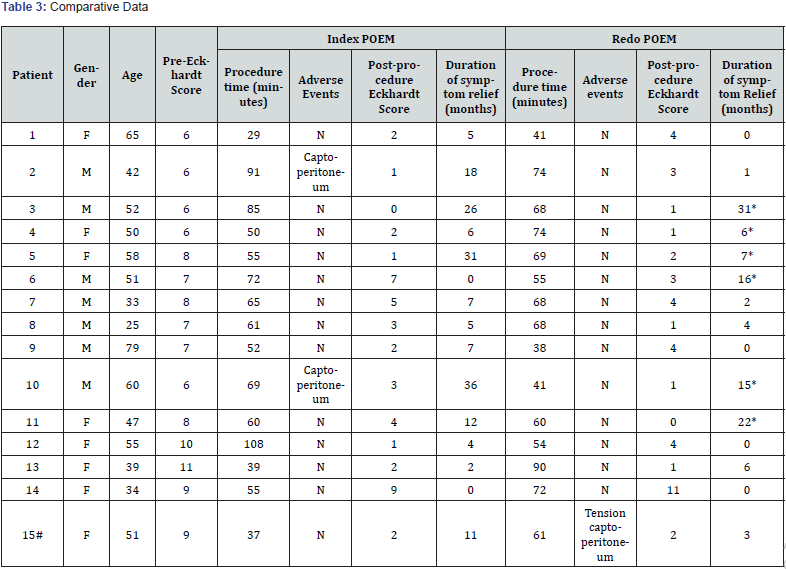
10 out of 15 patients (67%) achieved clinical success postredo procedure with an Eckardt score ≤3. One patient (7%) had no improvement at all post redo POEM, while four additional patients (27%) had improvement of their Eckardt score without meeting criteria for clinical success. (Figure 1) describes the duration of symptom relief after index and redo POEM. Patients with clinical success at initial follow up were followed for assessment of longterm symptom relief at 6 months or greater following their redo- POEM, except for 1 patient who was lost to follow up. Of the 10 patients with clinical success, two (20%) had limited duration of symptom relief, achieving less than 6 months of therapeutic effect from their redo POEM (one and four months respectively). Seven patients (70%) reported long-term relief as reported by an Eckardt score ≤3 at 6 months or greater, with five patients reporting continued symptom relief at time of data extraction (range 7+ to 31+ months, median 16 months). The patient who was lost to follow up but had continued symptom relief at her last point of contact, which was 3 months post redo procedure.
Comparative Outcomes
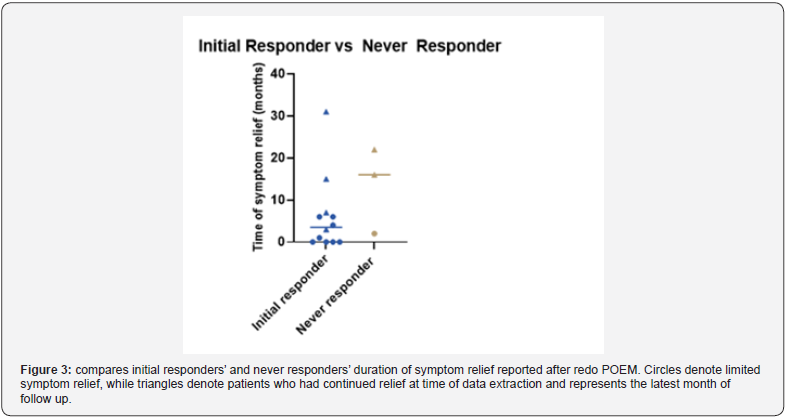
There was no significant difference in comparing those who had prior interventions before index POEM with those who didn’t in observing short-term outcomes of redo POEM (p = 0.99, OR 1.5, 95% CI: 0.17, 12.42). Two of the 7 patients with long-term clinical relief (28.6%) had prior interventions done before index POEM procedure, including Heller myotomy and bolutin toxin injections, while two of the 7 patients who did not achieve longterm clinical relief (28.6%) also had prior interventions, including pneumatic dilatations (Figure 2). Additionally, there was no difference between never-responders and initial responders for index POEM regarding the long-term duration of symptom relief after redo POEM (p = 0.99, OR 1.7, 95% CI: 0.15, 28.44). Two of the 7 patients with long-term clinical relief after redo POEM (28.6%) did not report clinical success after initial POEM. Meanwhile, one of the 7 patients (14.3%) who had limited or no relief from their redo POEM also initially failed their index POEM (Figure 3). Among the five patients who failed the redo POEM, one also had no response at the index POEM. This patient had severe diffusely dilated esophagus with an esophageal diameter of at least 5cm or greater [8].
Adverse events
Two patients in the index POEM had abdominal pain with x-ray confirmed captoperitoneum and recovered without intervention. One patient in the redo POEM had tension captoperitoneum during the procedure which resolved shortly after needle decompression.

Discussion
While POEM has been studied as a salvage therapy for patients who have previously failed other interventions, it has not been universally adapted as a revision therapy for patients who develop a recurrence of symptoms after initial POEM [9]. This is likely multifactorial, including not only limited data being available regarding long-term symptom relief but also concern regarding the safety in repeating myotomy. However, a recent meta-analysis including a total of 46 patients demonstrated 100% technical success and 85% clinical success10, which is in line with the results from our study which were 100% and 67% respectively. Adverse events from the above study were limited to 17% of patients experiencing peri-procedural bleeding [10]. In our study, there was only one reported peri-procedural adverse event during our redo POEMs, which suggests that there is minimal increased risk of major adverse events in repeating myotomy. Additionally, those patients who had captoperitoneums during index POEM did not experience any adverse events during their revision POEM, which is reassuring from a safety perspective when recommending revision procedures in patients with previous procedural events.
Our study is the first to document same-orientation (posterior) myotomies for both the index and redo POEM, with 11 of the 15 procedures performed as same-orientation myotomies [11,12]. These were typically performed at the posterior orientation of the esophagus. Those that were not performed at same-orientation were due to endoscopist preference, poor positioning, or reasons otherwise not stated. Even in recently published studies of redo POEM, there is still some concern surrounding the safety of same orientation myotomy due to speculation of increased fibrosis at the site of initial myotomy [9]. However, there is additional evidence of the feasibility of same-side myotomies from previous studies observing no difference in post-operative Eckardt scores or procedural time in patients who had previous endoscopic intervention and those that were treatment naïve prior to POEM [13]. This supports previous publications that have demonstrated similarly favorable outcomes for patients who had prior pneumatic dilation, botulinum toxin injections, and Heller myotomies [14,15,16]. Our study demonstrated similar clinical success rates to other published studies, as described previously [10], and boasts no significant difference in procedural times between index and redo POEM. Parallel observations in surgical myotomies have speculated that aside from fibrosis and scarring, treatment failure could arise from insufficient length of myotomy [17]. While there was no difference in length between index and redo POEM in our study, the myotomy length distal to the GEJ in subjects’ redo POEM was less than our index POEM. Despite this, most patients had improvement in their Eckardt score after intervention, which suggests fibrosis and scarring may be the main reason for recurrence in our patients.
Our study is the first to expand length of time of analysis beyond short-term outcomes of redo-POEMs, following 14 of the 15 patients beyond 6 months, with one of the patients being lost to after 3 month follow up. Despite 10 patients who achieved clinical success at initial follow up after redo POEM, only seven patients had six months or greater of symptom relief. The return of dysphagia and regurgitation symptoms is not uncommon and has been studied long-term in patients with POEM procedure. A recent study published the results of 32 patients’ post-POEM over the course of 7 years, demonstrating that 30% of the patients who achieved initial documented clinical success had increases in their Eckhardt score over time [18]. While the current offered treatments aim at reducing symptom burden, it is important to remember that the underlying pathophysiology of achalasia remains, and no matter the intervention or clinical outcome, all patients are recommended to follow modified diets, such as avoiding triggering foods and staying upright peri-prandially, to avoid exacerbation of symptoms. From our observations, it does seem that early recurrence after initial POEM predicts limited or no relief from redo POEM. Nevertheless, our study offers enlightening information regarding outcomes of redo POEMs after six months, suggesting that even patients who have recurrent symptoms following initial POEM can benefit from a redo POEM. One patient who clinically failed both index and redo POEM had severe dilation throughout the esophagus, suggesting that patients with diffusely dilated anatomy may not benefit from POEM.
There are several limitations to this study. This is a retrospective study and selection bias may have occurred. As these were done at a referral site, it was difficult to collect follow up esophagrams as well as manometry after both initial and redo POEMs, and therefore we were unable to include LES pressures in our analysis. This limits our analysis to subjective interpretation from patient-reported symptom scores rather than improvement in swallowing function on esophagram or reduced LES from manometry. Additionally, due to the rarity of the clinical condition and even more infrequent need for revision POEM, our sample size is small and makes it difficult to make definitive conclusions regarding redo POEM efficacy in patients with achalasia. Additionally, patients were not objectively tested for gastroesophageal reflux disease (GERD) through pH-catheter off PPI, so the prevalence of GERD in these patients post redo POEM is unknown. However, when analyzed in conjunction with existing studies, our study not only confirms the safety of redo POEM, but it also proposes potential benefit in patients with previous interventions and never-responders. Furthermore, it introduces potential long-term duration of symptom relief from redo POEM and makes it an attractive option for salvage therapy in patients who have previously failed POEM intervention. Our observations indicate that we should offer redo POEM for both patients with no response to index POEM and patients with recurrent symptoms after index POEM, except patients who have severe diffusely dilated esophagus with an esophageal diameter greater than 5cm.
*Denotes continued symptom relief at time of data extraction #lost to follow up, denotes time of reported symptom relief at last point of contact
References
- Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT (2020) ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol 115(9): 1393-1411.
- Zou BC, Zhang L, Qin B, Wang SH, Cheng Y, et al. (2020) Effects of Peroral Endoscopic Myotomy on Esophageal Function in the Treatment of Achalasia. Surg Innov 27(4): 333-341.
- Werner YB, Hakanson B, Martinek J, Repici A, bredenoord AJ, et al. (2019) Endoscopic or Surgical Myotomy in Patients with Idiopathic Achalasia. N Engl J Med 381(23): 2219-2229.
- Kumbhari V, Tieu AH, Onimaru M, El Zein MH, Teitelbaum EN, et al. (2015) Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of Type III achalasia in 75 patients: a multicenter comparative study. Endosc Int Open 3(3): E195-201.
- van Hoeij FB, Ponds FA, Werner Y, Sternbach JM, Fockens P, et al. (2018) Management of recurrent symptoms after per-oral endoscopic myotomy in achalasia. Gastrointest Endosc 87(1): 95-101.
- Kumbhari V, Tieu AH, Azola A (2015) Double peroral endoscopic myotomy for achalasia. Gastrointest Endosc 82: 953.
- Wehbeh AN, Mekaroonkamol P, Cai Q (2016) Same site submucosal tunneling for a repeat per oral endoscopic myotomy: A safe and feasible option. World J Gastrointest Endosc 8(18): 669-673.
- Gockel I, Junginger T (2007) The value of scoring achalasia: a comparison of current systems and the impact on treatment--the surgeon's viewpoint. Am Surg 73(4): 327-31.
- Tan S, Zhong C, Ren Y, Luo X, Xu J, et al. (2021) Efficacy and Safety of Peroral Endoscopic Myotomy in Achalasia Patients with Failed Previous Intervention: A Systematic Review and Meta-Analysis. Gut Liver 15(2): 153-167.
- Tyberg A, Seewald S, Sharaiha RZ, Martinez G, Desai AP, et al. (2017) A multicenter international registry of redo per-oral endoscopic myotomy (POEM) after failed POEM. Gastrointest Endosc 85(6): 1208-1211.
- Li QL, Yao LQ, Xu XY, Zhu JY, Xu MD, et al. (2016) Repeat peroral endoscopic myotomy: a salvage option for persistent/recurrent symptoms. Endoscopy 48(2): 134-40.
- Werner YB, Costamagna G, Swanstrom LL, Renteln DV, Familiari P, et al. (2016) Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut 65(6): 899-906.
- Sharata A, Kurian AA, Dunst CM, Bhayani NH, Reavis KM, et al. (2013) Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg 17(7): 1188-92.
- Orenstein SB, Raigani S, Wu YV, Pauli EM, Phillips MS, et al. (2015) Peroral endoscopic myotomy (POEM) leads to similar results in patients with and without prior endoscopic or surgical therapy. Surg Endosc 29(5): 1064-70.
- Vigneswaran Y, Yetasook AK, Zhao JC, Denham W, Linn JG, et al. (2014) Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg 18(6): 1071-6.
- Ling T, Guo H, Zou X (2014) Effect of peroral endoscopic myotomy in achalasia patients with failure of prior pneumatic dilation: a prospective case-control study. J Gastroenterol Hepatol 29(8): 1609-13.
- Gockel I, Timm S, Sgourakis GG, Musholt TJ, Rink AD, et al. (2010) Achalasia--if surgical treatment fails: analysis of remedial surgery. J Gastrointest Surg 14 Suppl 1: S46-57.
- Zhang WG, Chai NL, Zhai YQ, Linghu EQ, Li HK (2020) Long-term outcomes of peroral endoscopic myotomy in achalasia patients with a minimum follow-up of 7 years. Chin Med J (Engl) 133(8): 996-998.






























