Laparoscopic Bilio-Digestive Derivations, a Potentially Life-Saving Procedure-Case Report
Razvan Calin Tiutiuca1, Alina Ioana Nastase Puscasu2*, Nicoleta Stoenescu3, Mihaela Moscalu4, Vacarasu Andrei Bogdan5, Bondoc Irina6, Mardare Mara7, Bradea Costel8, Ginghina Octav9 and Lupascu Cristian10
1Senior surgeon, Doctor of Medical Sciences, Iasi Military Hospital, University of Medicine and Pharmacy "Grigore T. Popa" Iasi, Romania
2General Surgery Specialist Doctor, PhD student University of Medicine and Pharmacy "Grigore T. Popa" Iasi, Romania
3Psychologist, PhD student, University "Alexandru Ioan Cuza" Iasi, Romania
4Associate Professor, University of Medicine and Pharmacy "Grigore T. Popa", Iasi, Romania
5Senior Resident, Bucharest Oncological Institute, Romania
6Senior Resident, Bucharest Oncological Institute, Romania
7Senior Resident, Bucharest Oncological Institute, Romania
8Associate Professor, University of Medicine and Pharmacy "Grigore T. Popa" Iasi, Romania
9Professor, University of Medicine and Pharmacy "Carol Davila" Bucharest, Romania
10Professor, University of Medicine and Pharmacy "Grigore T. Popa" Iasi, Romania
Submission: March 18, 2024; Published: March 28, 2024
*Corresponding author: Alina Ioana Nastase Puscasu, General Surgery Specialist Doctor, PhD student University of Medicine and Pharmacy “Grigore T. Popa” Iasi, Romania.
How to cite this article: NRazvan Calin T, Alina Ioana Nastase P, Nicoleta S, Mihaela M, Vacarasu Andrei B, et al. Laparoscopic Bilio-Digestive Derivations, a Potentially Life-Saving Procedure-Case Report. Open Access J Surg. 2024; 15(3): 555911. DOI: 10.19080/OAJS.2024.15.555911.
Abstract
Mechanical jaundice is a therapeutic challenge in particular situations represented by cases where papillo-sphincterotomy is contraindicated or fails to clear the bile duct or where percutaneous drainage techniques are ineffective. he primary responsibility of the radiologist is to distinguish between particular anatomical and pathological situations that adequately direct the therapeutic strategy, especially in serious clinical cases, for the fastest possible adoption of the appropriate treatment technique to save the patient's life. It is now possible to diagnose obstructive jaundice early and precisely without causing any patient discomfort thanks to the availability of non-invasive imaging techniques like computed tomography and magnetic resonance imaging (MRI).
The advancement of medical technology has led to the development of numerous therapeutic methods intended to improve the patient's prognosis. The use of ERCP and the placement of biliary stents to aid biliary drainage have changed the conventional surgical approach to treating patients with obstructive jaundice. The decision to use surgical techniques as a life-saving treatment should consider the unique characteristics of the patient, the stone, the surgeon's experience, and the resources at hand. For the best results, a multidisciplinary strategy combining gastroenterologists, radiologists, and surgeons is necessary.
Keywords: Hepato-biliopancreatic imagistic; Endoscopic retrograde; Surgical management; Bile duct stone; Pancreatic cancer
Abbreviations: MRI: Magnetic Resonance Imaging; ERCP: Endoscopic Retrograde Cholangiopancreatography; MRCP: Magnetic Resonance Cholangiopancreatography; EBD: Endoscopic Biliary Drainage; PTBD: Percutaneous Transhepatic Biliary Drainage; ENBD: Endoscopic Nasobiliary Drainage; GI: Gastrointestinal; CDD: Choledochoduodenostomy; CBD: Common Bile Duct; MR: Magnetic Resonance; FOV: Field of View
Introduction
Obstructive jaundice is a complex syndrome with both benign (choledocholithiasis, hydatid cyst, chronic pancreatitis) and malignant (pancreatic cancer, cholangiocarcinoma, and gallbladder cancer) etiologies, and it has a special place in biliopancreatic pathology. It is of the utmost importance due to changes in local and general status of the organism, difficult etiologic diagnostic problems for the clinician and whose solution requires teamwork, which involves both the surgeon, gastroenterologist, anesthesiologist. The development of laparoscopic and robotic surgery and upper gastrointestinal endoscopy for the treatment of biliary duct disease opened up the possibility of treating obstructive jaunice using endoscopic retrograde cholangiopancreatography, greatly limiting the use of traditional surgical procedures.
However, in some particular situations, the specifics of the patients' diseases have occasionally imposed a special treatment approach, and sometimes decision-making requires a multidisciplinary team. When viewed on a CT scan, biliary calculi can appear in a variety of ways, from highly calcified, lamellated radio dense calculi to low-density calculi because of the presence of cholesterol. Depending on its HU value, an air bubble can be clearly distinguished from calculi on CT. Stone- or cholangitis-related local irritation may result in wall thickening, mucosal augmentation, and periductal fat stranding. However, the likelihood of malignancy should be considered when there is mural enhancement [1].
CT is an essential tool for assessing liver morphology because it gives precise details on the size, texture, and existence of localized lesions in the liver. CT can help in identifying characteristics linked to increased intra-abdominal fluid when analyzing liver morphology to anticipate ascites formation. Magnetic resonance cholangiopancreatography can identify stones as tiny as 2 mm in size, which are shown as filling defects surrounded by T2 hyperintense bile, making it superior to CT and USG for the identification of choledocholithiasis. Regular T1 and T2 weighted sequences, on which pigmented stones look hyperintense on T1 as opposed to cholesterol stones, which seem hypointense, are required for further characterization of calculi. Although, they can be mistaken for stones due to their smooth, rounded shape and propensity to group and rise to the nondependent surface, air bubbles are typically distinguishable from them [2]. Benign and malignant structures can be distinguished by specific characteristics. More characteristics that are suggestive of benign stricture are wall thickness less than 1.5 mm, stricture length less than 9 mm, and upstream bile duct dilatation of 17 mm. A dilated bile duct with abrupt, smooth tapering on MRCP is indicative of post-operative biliary stricture. Additionally, the anatomical level and duration of the structure can be accurately depicted by MRCP, which aids in its operational management [3]. A CT scan can reveal stricture-related problems such cholangitis and an accompanying abscess [2].
Multi-detector CT is still useful for determining the extent of bile duct obstruction and local invasion, but MRI offers better tissue characterization for a small subset of cancers, such as lymphoproliferative diseases, which exhibit diffusion restriction. Obstruction causing PD, common bile duct, or both, to enlarge is the typical imaging finding on MRCP. The double-duct indication is caused by dilatation of both ducts. The unequal narrowing of the pancreatic and bile duct in the area of the pancreatic head is another evidence that points to a malignant etiology [2]. Endoscopic Retrograde Cholangiopancreatography (ERCP) was for a long time the gold standard for diagnosing patients with obstructive jaundice. It does, however, have an intrinsic complication rate of 3-9% and a mortality rate of 0.2-0.5% due to the fact that it is an intrusive treatment [2]. Cross-sectional imaging has significantly improved, especially with the introduction of magnetic resonance cholangiopancreatography (MRCP), so that ERCP now mainly serves therapeutic purposes.
Several therapeutic techniques aimed at enhancing the patient's prognosis have been developed because of medical technology's progress. The traditional surgical strategy for treating patients with obstructive jaundice has been transformed by the use of ERCP and the implantation of biliary stents in helping biliary drainage. Endoscopic biliary drainage (EBD) and percutaneous transhepatic biliary drainage (PTBD) are two different types of biliary drainage. Endoscopic nasobiliary drainage (ENBD), which is external drainage, and stent insertion, which is internal drainage, are the two forms of EBD. Because there are fewer complications, endoscopic drainage is preferable to percutaneous drainage [4-6].
Obstructive jaundice is a typical condition that can be caused by either benign or malignant diseases. Prior to the invention of endoscopic biliary stenting in the early 1980s, surgery was the standard of care for biliary obstruction. According to the underlying problem, surgical options for obstructive jaundice included the Whipple surgery with hepaticojejunostomy, cholecystojejunostomy, choledochojejunostomy, or other techniques. Biliary stents are tubes composed of plastic or metal that are used to cure biliary leaks or reduce obstruction in the biliary tree [6-8]. Surgery has a higher morbidity than endoscopic biliary stenting when used for palliation of malignant biliary blockage.
However, physicians who care for patients with jaundice ought to be aware of stenting as a therapy option and life-saving procedure. The need for removal and replacement due to stenosis of stents remains despite advancements in stent manufacturing [9-12].
There are several contraindications for Endoscopic Retrograde Cholangiopancreatography (ERCP). Some of these include having had gastrointestinal (GI) surgery that has blocked the ducts of the biliary tree, having pouches in your esophagus (esophageal diverticula) or other abnormal anatomy that makes the test difficult to perform, and having barium within the intestines from a recent barium procedure since it may interfere with an ERCP. Contraindications to ERCP are relative and may include visceral perforation, suboptimal anesthesia support, and partially or fully anticoagulated patients. Additionally, lack of patient consent is an absolute contraindication to ERCP [13]. The anatomical features of individuals with obstructive jaundice and the contraindications of biliary drainage afforded by the implantation of biliary stents have directed the therapy towards conventional surgery.
The choice of surgical tactics should be based on individual patient characteristics, stone characteristics, surgeon expertise, and available resources. A multidisciplinary approach involving gastroenterologists, radiologists, and surgeons is essential for achieving optimal outcomes. A choledochoduodenostomy (CDD) is a surgical procedure that creates an anastomosis between the common bile duct (CBD) and an alternative portion of the duodenum. It is indicated for the treatment of primary common bile duct stones with a dilated common bile duct as well as benign strictures of the distal bile duct. It may also be favored by some surgeons in place of the transduodenal approach for stones impacted in the ampulla. CDD is also used for benign conditions such as distal bile duct stricture or recurrent choledocholithiasis [14].
Choledochojejunostomy is a surgical procedure that creates an anastomosis between the common bile duct (CBD) and the jejunum. It is performed to relieve symptoms of biliary obstruction and restore continuity to the biliary tract. The main indications for choledochojejunostomy are benign, mainly iatrogenic, biliary strictures and malignant obstruction of the biliary system caused by peri-ampullary tumors. It may also be used in the treatment of selected patients with retained, recurrent, and impacted bile duct stones; strictures of the bile ducts; stenosis of the sphincter of Oddi; pancreatitis associated with biliary disease; choledochal cysts; fistulas of the bile duct; and biliary obstruction, either benign or malignant.
Cholecystoenteric anastomosis involves removing one's gallbladder and connecting it to their small intestine. Although this option isn't as commonly used as others, it can help those with specific conditions affecting their gallbladder and/or liver function. Biliodigestive derivations are a life-saving technique that has been used to treat various liver and bile duct ailments for many years. As with any medical procedure, there are pros and cons associated with biliodigestive anastomosis. On the one hand, the primary advantage of these procedures is their ability to help alleviate symptoms associated with malignant diseases such as biliary obstruction, jaundice, or cholangitis. Additionally, they can be beneficial in treating other conditions like benign strictures or gallstones.
However, there are also some downsides to consider when contemplating this option. One major drawback is that these procedures require significant surgical skill and experience due to their complexity. Moreover, they may not always be suitable for individuals who have underlying comorbidities or severe liver damage.
Additionally, while biliodigestive derivations do provide relief from certain symptoms related to liver disease, they don't necessarily cure it entirely. Patients often need ongoing monitoring and treatment even after undergoing this type of surgery.
The choice of surgical tactics for obstructive jaunice should be individualized based on the patient's condition, preferences and expectations, as well as the availability of resources and expertise. The optimal surgical tactics should aim to achieve biliary drainage, prevent complications, minimize morbidity and mortality, and improve quality of life [15]. Accurate preoperative evaluation is vital for optimal surgical planning in patient with obstructive jaunice. The assessment includes a detailed history, physical examination, laboratory investigations (complete blood count, liver function tests, coagulation profile), and imaging studies such as ultrasound, magnetic resonance cholangiopancreatography (MRCP), or endoscopic retrograde cholangiopancreatography (ERCP). In this article we have chosen to present the cases of two patients who required a biliodigestive anastomosis in the absence of any other therapeutic option available.
Case 1
Malignant biliary blockage may be difficult to drain endoscopically. An endoscopic ultrasound-guided method may be useful for patients in whom traditional wire-guided cannulation or precut procedures have failed. In patients with malignant biliary obstruction from pancreatic cancer, concurrent duodenal strictures happen in 10–20% of cases [16].
Interventions that are guided by endoscopic retrograde cholangiopancreatography (ERCP) are crucial for the detection, management, and palliation of pancreatic cancer. The diagnosis of pancreatic cancer is aided by ERCP-guided biliary tissue sampling, which also allows for therapeutic measures during the same procedure. In advanced pancreatic cancer, biliary or gastric outlet obstruction is sometimes possible. The quality of life is increased, and effective palliation is provided by the implantation of either biliary or enteral stents under ERCP guidance [17].
We discuss a 73-year-old female patient diagnosed with breast cancer (matrix producing metaplastic carcinoma) in Octomber 2022 who presented to the emergency unit with tegumentary jaundice, asthenia, fatigue, and very altered general condition. Biological findings identified a high level of bilirubin (25 mg/dl), cholestasis syndrome and coagulation disorders. The patient is cholecystectomysed by classical surgery in history. To assess the cause of jaunice, further imagistic investigations were performed.
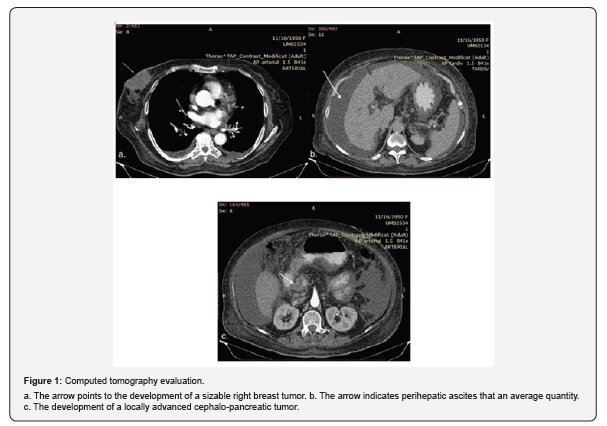
Computer tomography of the chest and abdomen revealed absence of suggestive nodular pulmonary parenchymal lesions for secondary determinations. Absence of mediastino-hilar adenopathies. Absence of pleuro-pericardial fluid overflow. The right mammary node, at the junction of the lower quadrants, iodophil, inhomogeneous structure, with internal necrosis, irregular contour, with extensions around, without affecting the muscular plane, dimensions of 30/48/ mm (ap/t/cc). Right axillary node of 10/20 mm. Liver with increased dimensions (antero-posterior diameter of the right lobe 175 mm, of the left lobe of 70 mm), shows some bilobar microcalcifications, and at the border of segments II-IV a 31/34 mm nodule with contrast uptake in arterial time and wash-out in late time, outlining a pseudo capsule (Figure 1). Nodular thickening of the duodenal wall with dimension of 25/30 mm, at the level of the lower knee (limit of segments D2-D3), in contact with the cephalic pancreas (without a defined limit). Perilesional adenopathy of 10/12 mm. No free intraperitoneal fluid was identified. Absence of bone lesions suspicious of malignancy. We concluded several diagnoses: Right mammary tumoral mass, hepatic nodular lesion that requires an MRI examination with a dedicated protocol and duodenal parietal thickening for which we recommend endoscopy with biopsy.
We chose to perform a magnetic resonance imaging (IRM). In addition to being non-invasive, magnetic resonance imaging (MR) offers the benefits of a large field of view (FOV), great patient tolerance, and the ability to present cholangio-pancreatico visually three-dimensional (3D) data sets.
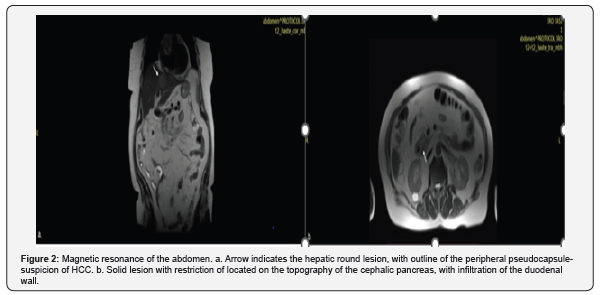
Magnetic resonance of the abdomen hightlighting homogeneous hepatomegaly (LDH 170 mm diam A-P), presents bilobar lesions with the following characteristics: in the anterior subcapsular segment II, round lesion, with outline of the peripheral pseudocapsule, moderately hypersignal on the seventh DW, with moderate and inhomogeneous contrast uptake, diameter 33 /40mm- suspicion of HCC (late scans do not provide diagnostic information due to the absence of biliary excretion) (Figure 2a). Multiple other lesions in T2 hypersignal with Dw restriction, are marked bilobar with sizes between 6 and 12 mm suspicious of MTS. Solid lesion with restriction of Dw located on the topography of the cephalic pancreas, with infiltration of the duodenal wall, with dimensions of 29/26 mm (Figure 2b). CBP 13mm, apparently free. Non-dilated CBIH. Portal vein of 14mm. Absence of retroperitoneal adenopathies. No free intraperitoneal fluid. The IRM scan revealed: Macronodular liver segment II lesion suspected of hepatocarcinoma - biopsy is recommended. Cephalopancreatic lesion suspected of malignancy - echoendoscopy and biopsy are recommended. Bilobar sub centimeter hepatic lesions with secondary appearance.
We scheduled an upper digestive endoscopy and we discovered at the level of the DII/DIII junction, a hemi circumferential tumor, with an ulcerated infiltrative character (malignant macroscopic characteristic). The multiple biopsies performed, revealed two fragments of duodenal mucosa, one of which is viable to evaluate, having an area with carcinomatous infiltration with tubular and trabecular architecture, cuboidal tumor cells with moderate and increased cyto-nuclear pleomorphism, together with desmoplastic stroma with moderate inflammatory infiltrate lympho-plasmocytic. Numerous tumor emboli are also identified in the lymphatic vessels. Duodenal epithelium does not show dysplasia. Immunohistochemistry registered: CK7, CK19 - intensely diffusely positive in the tumor area and at the level of lymphatic emboli; CDX2 - weak or moderately positive in frequent tumor cells; HSA, CK 20 - negative in the tumor area and at the level of the epithelial groups in the lymphatic vessels Mammaglobin, GCDFP15, ER - negative in the tumor area and at the level of the lymphatics. The final diagnostic concludes an adenocarcinoma infiltration with a pancreatic-biliary phenotype, the correlation with the imaging data pointing to a pancreatic origin.
A gastroenterology facility with expertise in biliary stents for malignant diseases receives the patient as a referral. The patient is sent to the surgery clinic so that a life-saving biliodigestive anastomosis can be done after the attempt to conduct stenting failed despite several attempts. In this case, after carefully examine the patient, we chose to perform a laparoscopic latero-lateral choledocho-duodenal anastomosis, after a difficult dissection to release adhesions due to previous interventions. On the day following surgery an episode of liver failure is recognized, and a 3500–4000 ml/24-hour increase in ascites flow is observed on the drain tube. Because there were no large parietal incisions (this allowed control of intra-abdominal pressure and reduced the risk of postoperative wound dehiscence), the aggressive and effective intense therapy made the therapeutic approach more manageable. On the 12th postoperative day, the patient underwent discharge in an improved general state. A low-flow ascitic fistula persisted (200-250 ml/day).
After 30 days, the patient was readmitted with ascitic fistula with a flow rate of 15 ml per day, which allowed drainage suppression. The general condition was satisfactory, jaundice with total bilirubin levels of 2 mg/dl with increased direct bilirubin to values of 1.5 mg/dl, without dilation of bile ducts. Intestinal transit present with normally colored stools, digestive tolerance that allows normal nutrition. A good quality of life was assessed accordingly. We referred the case to the oncology institute in order to initiate chemotherapy treatment.
Case 2
Patients with gastrointestinal cancer are increasingly living longer thanks to advancements in surgical methods and postoperative patient care [18,19]. As a result, it is important to pay closer attention to variables that could impact quality of life following surgery. Gallstone development is one such factor. Following stomach resections, biliary stones can show clinically in a variety of ways, from asymptomatic instances to serious consequences such biliary colic, cholecystitis, or pancreatitis [20]. The length of lymph node dissection, style of operation, type of reconstruction, individual surgeon experience, and follow-up procedure are only a few of the local factors that may have an impact on the occurrence of gallstones after gastrectomy.
The vagus nerve is severed during a complete and proximal gastrectomy. In contrast, pylorus-preserving distal gastrectomy preserves the right gastric artery and hepatic branch of the anterior vagus nerve [21]. During a gastrectomy, vagus nerve damage may increase the sphincter of Oddi's tension and lessen the gallbladder's ability to contract. Gallstone development and biliary stasis may follow as a result [22, 23]. After gastric resections, non-surgical and surgical methods can also be used to treat biliary stones. The use of drugs that dissolve stones or stop stone development is one non-surgical strategy. Laparoscopic cholecystectomy is one surgical option, but there are also more complex procedures such endoscopic procedures and lithotripsy.
A concern for therapeutic endoscopists is endoscopic retrograde cholangiopancreatography (ERCP) in post-gastrectomy patients with Billroth II (BII) reconstruction and Roux-en-Y (RY) reconstruction. In this group of people, significant challenges must be overcome, such as intubation to the Vater's ampulla, selective cannulation, and ampullary intervention. Before performing ERCP procedures on post-gastrectomy patients, a thorough understanding of postoperative anatomy and numerous instruments, including endoscopes and accessories, is essential for a satisfactory outcome [24]. We present a case of a 69-year-old male hospitalized in our surgical clinic with obstructive jaundice, cholestasis syndrome, hepatocytolysis syndrome. According to the patient's medical history, he was diagnosed with gastric cancer in 2018 and had distal gastric resection as treatment. We determine that the patient's symptoms started 4 months ago.
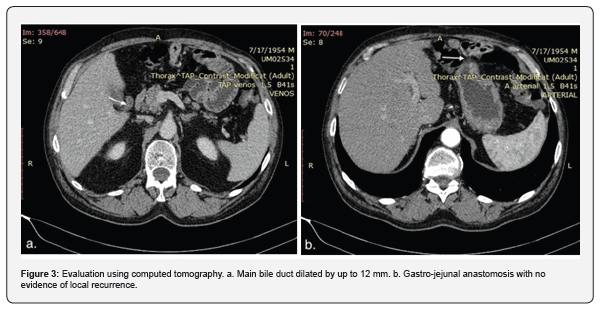
A chest and abdominal tomography was performed and the result encountered no CT-detectable pleuro-pulmonary lesions, except for a calcified nodule, 4 mm, located at the level of the posterior segment of the LSD, subpleural, and an emphysema bubble of 8 mm, at the level of the same segment. Hilar, mediastinal and bilateral axillary adenopathy’s are not detected. Liver with increased dimensions (antero-posterior diameter of LHD 153 mm), homogeneous structure, without focal lesions. Cholecyst with liquid content, apparently without hyperdense stones, wall with normal thickness. The intrahepatic bile ducts undilated. CBP dilated up to 12 mm, it decalibrates progressively at level of the pancreatic head (Figure 3a). Permeable portal vein with normal caliber. Post-subtotal gastrectomy status, with permeable end-to-side gastro-enter anastomosis (Figure 3b). There are no signs of recurrence at the anastomotic level. The diverticulum of approximately 27/15 mm, at the level of the second portion of the duodenum, with liquid and gaseous content. Absence of abdominal, pelvic or groin adenopathy’s. Abdominal aorta with calcified atheromatous plaques. Absence of peritoneal fluid. Half-full bladder, homogeneous liquid content, normal wall. Voluminous prostate, approximately 44 mm in diameter, homogeneous. Abdominal wall without changes. Arthritic changes in the spine included in the scanned volume, without CT elements suggestive of secondary bone lesions. The investigation concluded: Hepatomegaly. Post-subtotal gastrectomy status, apparently without complications. Dilated common bile duct, without an obvious cause, probably secondary to age. Enlarged prostate. Duodenal diverticulum.
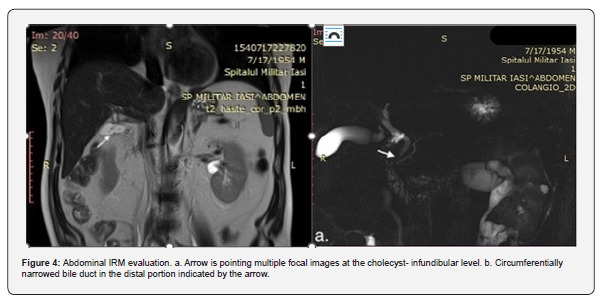
The failure to identify the underlying etiology of obstructive jaundice justified the suggestion of more imagistic research. The patient performs an abdominal IRM. Magnetic resonance imaging concludedliver with increased dimensions (antero-posterior diameter of LDS = 60 mm, respectively of LHD = 155 mm), with homogeneous structure. A distended liquid cholecyst, infundibular, with a wall of normal thickness, presents multiple focal images at the infundibular level, the largest with a maximum diameter of 2.6 mm (Figure 4a). Non-dilated intra-hepatic bile ducts. CBP with a caliber of 7 mm, with the progressive reduction of the caliber up to the level of the head of the pancreas. Circumferentially narrowed bile duct in the distal portion, over a length of approximately 4.5 mm, with a caliber of up to 3.2 mm, with the absence of visualization in the terminal 5 mm (Figure 4b). The right hepatic duct 5.4 mm and left hepatic duct with caliber 5.8 mm. Common hepatic duct with a caliber of 7.6 mm. Pancreas with dimensions of: 26 mm at the cephalic level, 13 mm corporeal and 15 mm at the caudal level. Undilated duct of Wirsung. There are no adenopathies or free intraperitoneal fluid at the abdominal level.
For ampullary access, standard ERCP with a duodenoscope is technically difficult and clinically ineffective. Despite the gastroenterologist's efforts, the ERCP was unsuccessful in this case. Considering the imaging investigations and after carefully evaluating the patient, we concluded the diagnosis of vesicular lithiasis and main biliary tract lithiasis and the surgical intervention is decided. Cholecystectomy, choledodochotomy, lavage of thecommon hepatic duct with calculus extraction and latero-lateral choledoco-duodenoanastomosys is performed laparoscopily. The postoperative evolution is favorable, with the resumption of digestive tolerability immediately after the surgical intervention. The patient is discharged on the 5th day after the operation, without complications. The imaging investigations performed at 3 and 6 months were within normal parameters.
Case 3
The collaborative effort between gastroenterology and general surgery departments facilitated the successful management of gallstones with main biliary tract obstruction in elderly patients. The timely surgical intervention and laparoscopic techniques contributed to a favorable postoperative outcome, highlighting the importance of a multidisciplinary approach in complex cases. We report a case of an 82-year-old female, presented clinically and via imaging with gallstones and evidence of main biliary tract involvement. Initial evaluation was conducted in the gastroenterology department, where an attempt was made to perform an ERCP (endoscopic retrograde cholangiopancreatography) but was unsuccessful. Due to this, the patient was referred to the general surgery department for specialized therapeutic management.
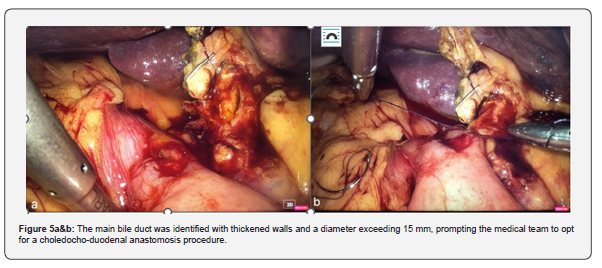
Upon arrival at the general surgery department, the patient presented with good general condition, was afebrile, but exhibited sclerotegumentary jaundice. Laboratory investigations revealed an inflammatory syndrome indicated by elevated C-reactive protein levels, as well as an increase in total bilirubin levels primarily due to direct bilirubin. Based on the clinical and laboratory findings, surgical intervention was deemed necessary. The patient underwent retrograde laparoscopic evaluation, cholecystectomy to address the gallstones and choledochoduodenal anastomosis with intraoperative cholangiography to manage the main biliary tract obstruction (Figure 5a, b).
The patient's postoperative course was favorable, marked by a notable decrease in liver function tests, bilirubin levels, and resolution of the inflammatory syndrome. Due to these positive indicators, the patient was discharged seven days after the surgery.
Conclusion
Endoscopic drainage of a malignant biliary obstruction may be challenging. Biliary or gastric outlet obstruction is sometimes possible in advanced pancreatic cancer. The placement of either biliary or enteral stents under ERCP guidance improves quality of life and offers efficient palliation. Following stomach resections, biliary stone formation is a common complication, and medical practitioners must be careful in identifying and treating it. For patient treatment to be optimized, it is crucial to comprehend the incidence, risk factors, clinical presentation, diagnostic techniques, and management strategies. To lower the burden of biliary stones in patients after stomach resections, future research should concentrate on creating preventive interventions and improving treatment algorithms.
Laparoscopic biliodigestive derivations have proven to be a life-saving technique for patients suffering from malignant and benign diseases causing obstructive jaunice in selected cases. While there are potential risks and drawbacks associated with this procedure, the benefits often outweigh them. Biliodigestive anastomosis has helped improve the quality of life for many individuals and has become an important treatment option in modern medicine. It is important to note that each patient's situation is unique, and therefore their treatment plan should reflect that. It is crucial the significance of early detection, interdisciplinary collaboration, and specialized therapeutic interventions in optimizing outcomes for patients with biliary tract disorders, particularly in elderly populations.
References
- Park MS, Kim TK, Kim KW, Park SW, Lee JK, et al. (2004) Differentiation of extrahepatic bile duct cholangiocarcinoma from benign stricture: findings at MRCP versus ERCP. Radiology 233(1): 234-240.
- Rana SS, Bhasin DK, Sharma V, Rao C, Gupta R, et al. (2013) Role of endoscopic ultrasound in evaluation of unexplained common bile duct dilatation on magnetic resonance cholangiopancreatography. Ann Gastroenterol 26(1): 66-70.
- Govil H, Reddy V, Kluskens L, Treaba D, Massarani-Wafai R, et al. (2002) Brush cytology of the biliary tract: retrospective study of 278 cases with histopathologic correlation. Diagn Cytopathol 26(5): 273-277.
- Zhang X, Wang X, Wang L, Tang R, Dong J (2018) Effect of covered self-expanding metal stents compared with multiple plastic stents on benign biliary stricture: A meta-analysis. Medicine (Baltimore) 97(36): e12039.
- Teoh AYB, Dhir V, Kida M, Yasuda I, Jin ZD, et al. (2018) Consensus guidelines on the optimal management in interventional EUS procedures: results from the Asian EUS group RAND/UCLA expert panel. Gut 67(7): 1209-1228.
- Ahmad J (2018) Metal, magnet or transplant: options in primary sclerosing cholangitis with stricture. Hepatol Int 12(6): 510-519.
- Huespe PE, Oggero S, Santibanes MD, Boldrini G, Agostino DD, et al. (2019) Percutaneous Patency Recovery and Biodegradable Stent Placement in a Totally Occluded Hepaticojejunostomy After Paediatric Living Donor Liver Transplantation. Cardiovasc Intervent Radiol 42(3): 466-470.
- Lee JH, Ahmed O (2019) Endoscopic Management of Pancreatic Cancer. Surg Oncol Clin N Am 28(1): 147-159.
- Teng F, Xian YT, Lin J, Li Y, Wu AL (2019) Comparison of Unilateral with Bilateral Metal Stenting for Malignant Hilar Biliary Obstruction. Surg Laparosc Endosc Percutan Tech 29(1): 43-48.
- Cassani LS, Chouhan J, Chan C, Lanke G, Chen HC, et al. (2019) Biliary Decompression in Perihilar Cholangiocarcinoma Improves Survival: A Single-Center Retrospective Analysis. Dig Dis Sci 64(2): 561-569.
- Zhumatayev DT, Baimakhanov AN, Abdykadyrov MK, Nurmakov DA, Raimkhanov AD, et al. (2020) Simultaneous surgical treatment tactics of acute destructive cholecystitis combined with choledocholithiasis: A case report. Int J Surg Case Rep 70: 230-233.
- Solomon S, Baillie J (2019) Indications for and Contraindications to ERCP. Elsevier sci 1: 54-58.
- Harold VG, Barry AL, Kenneth RS, Bradley A (1982) Frequency and indication for choledochoduodenostomy in benign biliary tract disease: Reassessment of therapeutic application. Am J Surg 144(6): 682-684.
- Parneet (2020) Current Assessment of Choledochoduodenostomy in the Management of Choledocholithiasis. J Med Dent Sci 19(1): 25-30.
- Vogt DP, Hermann RE (1981) Choledochoduodenostomy, choledochojejunostomy or sphincteroplasty for biliary and pancreatic disease. Ann Surg 193(2): 161-168.
- Jeffrey HL, Amanpal S (2012) Difficult endoscopic retrograde cholangiopancreatography in cancer patients. Int J Gastrointest Interv 1(1): 19-24.
- Yousaf MN, Ehsan H, Wahab A, Muneeb A, Chaudhary FS (2020) Endoscopic retrograde cholangiopancreatography guided interventions in the management of pancreatic cancer. World J Gastrointest Endosc 12(10): 323-340.
- Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, et al. (2016) Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat 48(2): 436-450.
- Paik KH, Lee JC, Kim HW, Kang J, Lee YS, et al. (2016) Risk factors for gallstone formation in resected gastric cancer patients. Medicine (Baltimore) 95(15): e3157.
- Seo GH, Lim CS, Chai YJ (2018) Incidence of gallstones after gastric resection for gastric cancer: a nationwide claims-based study. Ann Surg Treat Res 95(2): 87-93.
- Suh YS, Han DS, Kong SH, Kwon S, Shin CI, et al. (2014) Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann Surg 259(3): 485-493.
- Chen XJ, Li N, Huang YD, Ren S, Liu F, et al. (2014) Factors for postoperative gallstone occurrence in patients with gastric cancer: a meta-analysis. Asian Pac J Cancer Prev 15(2): 877-881.
- Hauters P, de Neve de Roden A, Pourbaix A, Aupaix F, Coumans P, et al. (1988) Cholelithiasis: a serious complication after total gastrectomy. Br J Surg 75(9): 899-900.
- Park CH (2016) Endoscopic Retrograde Cholangiopancreatography in Post Gastrectomy Patients. Clin Endosc 49(6): 506-509.






























