Early Recognition and Effective Intervention in Peripheral Vascular Trauma
Samantha Redden Chirinos1, Miguel Eduardo Rodriguez1, Gioacchino De Sario Velasquez1, Jesus Alejandro Cordova Guilarte1, Coralvia Yaroslangna Villanueva Perez2, Yeisson Rivero-Moreno1, Carolina Michelle Mejia Alaniz3, Andreina Rojas Marron1, Uche Brigid Smith4, Sruthi Siddada5, Victor Bolivar1, Maria Isabel Gomez-Coral6*
1Universidad de Oriente, Venezuela
2Universidad Nacional Experimental Francisco de Miranda, Venezuela
3Universidad Americana, Nicaragua
4Richmond Gabriel University, Saint Vincent, and the Grenadines
5Ramaiah Medical College, India
6Universidad del Valle de México, México, USA
Submission: September 13, 2023;; Published: September 25, 2023
*Corresponding author: Shreya Jayaram, Kasturba Medical College, Manipal, India, Email ID: shreyaj125@gmail.com
How to cite this article: Samantha Redden Chirinos1, Miguel Eduardo Rodriguez1, Gioacchino De Sario Velasquez1, Jesus Alejandro Cordova Guilarte1, Coralvia Yaroslangna Villanueva Perez, et al. Early Recognition and Effective Intervention in Peripheral Vascular Trauma. Open Access J Surg. 2023; 14(5): 555898. DOI: 10.19080/OAJS.2023.14.555898.
Abstract
The history of vascular trauma repair dates back to the 1700s when Dr. Hallowell introduced a significant paradigm shift. Dr. Hallowell advocated for repairing arterial injuries while maintaining the integrity of the blood vessel lumen. This change in approach emerged from the recognition of the high rates of morbidity and mortality associated with arterial ligation. It sparked optimism for improved patient outcomes through more straightforward repair techniques. Penetrating extremity traumas account for 5-15% of all traumatic injuries, with vascular injuries making up 1% of these cases. These injuries can result from various mechanisms, including blunt trauma, penetrating wounds, or both. Often, soft signs, such as a history of bleeding, are the primary symptoms observed. It’s worth noting that hard signs typically signal the need for surgical intervention. However, it’s essential to acknowledge that the incidence of arterial injuries in patients presenting with soft signs can vary widely, ranging from 3% to 25%. Therefore, while soft and hard signs remain valuable for guiding injury management, diagnostic tools like duplex ultrasound have become increasingly indispensable for confirming diagnoses. A comprehensive assessment, facilitated by a multidisciplinary approach, plays a pivotal role in making informed treatment decisions and ultimately improving patient outcomes. As we integrate modern diagnostic capabilities and maintain a high level of clinical suspicion, managing vascular extremity trauma continues to evolve, offering promising prospects for enhanced patient care.
Keywords: Peripheral Vascular Trauma; Compartment Syndrome; Penetrating Trauma; Vascular Injuries
Abbreviations: PVT: Peripheral Vascular Trauma; CTA: Computed Tomography Angiography; MRA: Magnetic Resonance Angiography; MRI: Magnetic Resonance Imaging; ATLS: Advanced Trauma Life Support; DSA: Digital Subtraction Angiography; ABC: Airway, Breathing, Circulation; AVI: Ankle-Brachial Index; HIT: Heparin-Induced Thrombocytopenia; ICU: Intensive Care Unit; PE: Pulmonary Embolism; DVT: Deep Vein Thrombosis; PACU: Post-Anesthesia Care Unit; PAD: Peripheral Arterial Disease; SIRS: Systemic Inflammatory Response Syndrome; DIC: Disseminated Intravascular Coagulation; PTA: Percutaneous Transluminal Angioplasty; PTFE: Polytetrafluoroethylene; ACS: Acute Compartment Syndrome; MAP: Mean Arterial Pressure; ICP: Intercompartmental Pressure; LMA: Laryngeal Mask Airway; ESR: Erythrocyte Sedimentation Rate; CRP: C-Reactive Protein; RBC: Red Blood Cell; FDP: Fibrin Degradation Product; PMN: Polymorphonuclear Leukocytes
Introduction
Peripheral vascular trauma refers to injuries sustained by blood vessels, encompassing both arteries and veins, with a diameter exceeding 4 mm [1]. Statistics indicate that approximately 1.5% of civilian trauma patients in the United States experience vascular injuries. Yet, the gravity of these injuries is evidenced by their contribution to over 20% of all trauma-related fatalities [2,3]. This classification is further categorized based on the mechanism of injury—blunt, penetrating, or a combination thereof—as well as the anatomical location, specifically the upper or lower extremity. Penetrating trauma can result from projectiles like bullets, blast fragments, or sharp objects like knives, coat hangers, and keys. In contrast, blunt trauma arises secondary to fractures or dislocations [3]. The predominant clinical manifestations of vascular trauma include hemorrhage and tissue and organ ischemia. Clinical presentations are intricately tied to the mechanism of injury. Significant damage to major vessels, including the brachiocephalic trunk artery, can trigger substantial bleeding, resulting in hypotension and shock [3,4].
Physical examination plays a pivotal role in confirming vascular injuries and subsequently guiding the decision for surgical intervention. Signs and symptoms of limb vascular injuries can be categorized as “hard” or “soft,” delineating the urgency of intervention. For diagnosis, methods such as the ankle-brachial index assessment, Doppler ultrasound, and angiography prove invaluable [3,4]. Swift and accurate diagnosis is pivotal in averting complications and expediting necessary interventions. Central to effective management is the rapid control of bleeding and the restoration of blood flow. In cases where timely revascularization cannot be achieved, amputation may become a necessary recourse. Consequently, immediate surgical intervention facilitates functional recuperation and limb preservation [3,4]. Considering these critical considerations, the principal objective of this article is to offer a comprehensive overview of early recognition and intervention in cases of peripheral vascular trauma. By shedding light on the multifaceted aspects of this topic, we aim to enhance medical understanding and promote effective clinical management.
Epidemiology
In urban trauma centers in the United States, the majority (75-80%) of peripheral vascular injuries stem from penetrating trauma, as reported by studies [5,6]. Roughly half of these penetrating injuries result from low-velocity handgun projectiles with minimal kinetic energy, typically around 1,000 ft lbs. In contrast, stab wounds contribute to 30% of such injuries in the U.S., but they become a more prevalent cause in regions with stricter firearm access [6]. Shotgun injuries, on the other hand, account for only 5% of peripheral vascular injuries [5,6]. Furthermore, peripheral vascular injuries resulting from blunt trauma to the extremities, including fractures, dislocations, crush injuries, and traction-related incidents, constitute a smaller portion, ranging from 5% to 25% of cases being treated [7].
Physiopathology
Understanding the physiopathology of peripheral vascular trauma is essential for effective diagnosis and management. It involves a complex interplay of vascular injury, hemostasis, inflammation, and tissue repair. A comprehensive understanding of these processes is essential to provide optimal care and minimize the potential long-term consequences. Peripheral vascular trauma can result from various mechanisms, including blunt or penetrating trauma, crush injuries, and fractures, and it often leads to life-threatening consequences if not promptly addressed.
In peripheral vascular trauma, the initial pathophysiological response involves injury to the vessel wall. Both arteries and veins can be affected, with arteries being more susceptible due to their higher pressure. Damage to the endothelial lining can lead to the exposure of subendothelial collagen, initiating platelet aggregation and the formation of a primary hemostatic plug [8-10]. This temporary plug helps minimize bleeding initially. Simultaneously, vasoconstriction occurs in response to releasing vasoactive substances, such as endothelin, from the damaged endothelium. This vasoconstriction helps reduce blood loss by narrowing the vessel lumen. However, these initial mechanisms may not be sufficient to control significant bleeding, especially in cases of severe vascular injury.
The next phase of physiopathology involves the activation of the coagulation cascade. Tissue factor and exposed collagen trigger the intrinsic and extrinsic pathways, forming fibrin strands and a stable blood clot. While this clot formation is necessary for wound healing, it can also cause complications such as thrombosis if it occludes the vessel entirely [8,11]. Inflammation plays a crucial role in the subsequent stages of peripheral vascular trauma. The damaged tissue releases proinflammatory cytokines, attracting neutrophils and macrophages to the injury site. This inflammatory response can exacerbate tissue damage and contribute to compartment syndrome, which occurs when increased pressure within a closed fascial compartment impairs blood flow and can lead to tissue necrosis [10,12].
The final phase of peripheral vascular trauma physiopathology involves tissue repair and remodeling. Fibroblasts produce collagen and other extracellular matrix components, leading to scar formation and the restoration of tissue integrity. However, complications such as aneurysm formation, stenosis, or chronic limb ischemia may occur if the repair process is disrupted or inadequate [9,13]. Timely diagnosis and intervention are crucial to prevent complications such as hemorrhage, ischemia, and limb loss. Early surgical repair or endovascular procedures may be necessary to restore vascular continuity and maintain adequate blood flow to the affected extremity.
Clinical Presentation
The clinical presentation of peripheral vascular trauma depends on different factors such as trauma mechanism, severity, time, and location. It can be represented by several signs and symptoms, usually classified as soft and hard signs, and this classification facilitates accurate and prompt diagnosis. Although some presentations are apparent, others are entirely masked, so this entity requires high suspicion and timely action [14]. The most frequently present symptoms are the soft signs, represented by a history of hemorrhage, among the most commonly encountered in peripheral vascular trauma setting at the time of injury. This may manifest as the history of oozing or spurting of blood from the wound site. While external bleeding alone may not confirm a vascular injury, it should raise suspicion, especially following penetrating trauma1. Also, developing a stable hematoma near the trauma site suggests vascular injury. This type of hematoma exhibits a non-pulsatile and non-expansive nature with non-lifethreatening features [14,15].
Pulse abnormalities, such as asymmetry and diminished peripheral pulse in the affected extremity compared to the contralateral limb. This could be suggestive of compromised blood flow. However, the association with other soft signs increases vascular trauma’s likelihood. These could be unexplained hypotension, a decreased mean arterial blood pressure without significant explanation, or a neurologic deficit like paresthesia, numbness, or tingling, which should heighten suspicion and require further tests and investigation. However, the total pulse absence suggests a hard sign and must advance to immediate action [16]. The hard signs involve more obvious, accurate, specific, and guided characteristics that expedite diagnosis and typically demand immediate action to prevent further morbidities and complications. These signs are more severe and acute in the trauma or injury setting, such as active hemorrhage, which is typically rapid, pulsatile, and life-threatening within minutes. Immediate intervention is imperative to control bleeding and restore perfusion [14].
Also is the presence of a rapidly expanding pulsatile hematoma. The palpable pulsation arises from blood escaping the artery with each heartbeat [15]. This situation can be associated with a bruit/thrill over the site of injury, and both signs represent classic signs of vascular trauma with continuous hemorrhage. In the case of the absence of pulse, especially when compared to the unaffected limb, this indicates a significant reduction or cessation of blood flow and distal limb ischemia, with evidence of paralysis, poikilothermic, severe pain, and hypothermia. The existence of one or more of these signs demands immediate surgical evaluation and intervention [14,16].
Peripheral vascular injuries can be categorized into three distinct groups. Category 1, often referred to as “Hard Signs,” encompasses indicators like pain, pallor, pulselessness, parasthesias, paralysis, pulsatile bleeding, and the presence of large or expanding hematomas. Patients displaying these signs have a greater than 90% likelihood of vascular injury. In Category 2, known as “Soft Signs,” patients exhibit relatively diminished yet palpable pulses, non expanding hematomas, and peripheral nerve injuries, with 30-35% of these cases resulting in vascular injury. Lastly, Category 3, or “Asymptomatic high risk,” includes individuals with penetrating wounds located within 1 cm of major neurovascular bundle areas (e.g., axillary, femoral, and carotid regions), as well as knee dislocations and severely displaced long bone fractures. In this group, up to 15-20% of patients may harbor vascular injuries [14-16].
Diagnosis
Diagnosing peripheral vascular trauma involves a comprehensive evaluation of the patient’s clinical presentation and often relies on a combination of clinical assessment and various imaging studies. These assessments aim to identify the location and severity of vascular injuries, guiding appropriate treatment decisions. Clinical evaluation is fundamental in diagnosing peripheral vascular trauma [17,18]. This involves a thorough physical examination, focusing on assessing vital signs, perfusion status, and visible injuries, such as wounds or ecchymosis. A detailed medical history, including the mechanism of injury, is also crucial in understanding the context of the trauma [19].
Imaging studies are essential for confirming the diagnosis and characterizing the extent of vascular injuries. Common imaging modalities include computed tomography angiography (CTA), duplex ultrasonography, magnetic resonance angiography (MRA), and conventional angiography [19,20]. CTA and MRA provide detailed visualization of the vascular anatomy and can identify the presence of arterial or venous injuries, pseudoaneurysms, or vascular occlusions. Duplex ultrasonography helps assess blood flow and detect hematomas or vessel dissections. Additionally, conventional angiography, although less commonly used in recent years, remains a valuable diagnostic tool for precisely identifying the location and severity of vascular injuries and often guides endovascular or surgical interventions [20,21].
Laboratory tests, such as complete blood counts and coagulation profiles, are also routinely performed to assess the patient’s overall health status, identify potential coagulopathies, and monitor for ongoing bleeding. Clinical correlation of the findings from these assessments and input from vascular surgeons, interventional radiologists, and other specialists is essential for making a definitive diagnosis and determining the appropriate treatment approach [18,22]. Accordingly, diagnosing peripheral vascular trauma involves a multidisciplinary approach, combining clinical evaluation with various imaging studies to accurately identify and characterize vascular injuries. This comprehensive assessment helps guide treatment decisions and improve patient outcomes.
Imaging studies
Diagnosing peripheral vascular trauma requires a thorough evaluation using various imaging studies to identify and characterize vascular injuries accurately. These imaging modalities are critical in guiding treatment decisions and improving patient outcomes. Computed Tomography Angiography (CTA) is one of the primary imaging modalities used to diagnose peripheral vascular trauma. CTA provides detailed cross-sectional images of blood vessels, allowing visualization of the vascular anatomy, identification of arterial or venous injuries, and assessment of pseudoaneurysms or vascular occlusions. It is a non-invasive and widely available technique, making it a valuable tool in trauma settings [23]. Duplex Ultrasonography is another essential imaging study. This real-time, non-invasive technique combines conventional ultrasound with Doppler technology to assess blood flow within the vessels. Duplex ultrasonography can detect hematomas, vessel dissections, and vascular injuries, particularly in cases of blunt trauma or suspected deep vein thrombosis [24].
Magnetic Resonance Angiography (MRA) is a non-invasive imaging modality that uses magnetic resonance imaging (MRI) techniques to create detailed images of blood vessels. MRA is particularly useful for evaluating peripheral vascular injuries in patients with contraindications to iodinated contrast agents or when detailed soft tissue characterization is required [25]. Although less commonly used today, conventional angiography remains a valuable diagnostic tool in peripheral vascular trauma. It involves the injection of contrast directly into the blood vessels and real-time X-ray imaging to visualize the vascular system. Conventional angiography provides high spatial resolution and can precisely identify the location and severity of vascular injuries, often guiding endovascular or surgical interventions [26].
Digital Subtraction Angiography (DSA) is a variation of conventional angiography that enhances the visualization of blood vessels by subtracting the surrounding structures, resulting in a clearer image of the vasculature. DSA is particularly useful in identifying vascular abnormalities and guiding therapeutic interventions [5]. Lastly, Magnetic Resonance Imaging (MRI) can provide additional information in cases of suspected vascular trauma, particularly when MRA is contraindicated or unavailable. While not primarily used for vascular assessment, MRI can help evaluate soft tissue injuries and potential complications related to vascular trauma [26-28].
Treatment Strategies
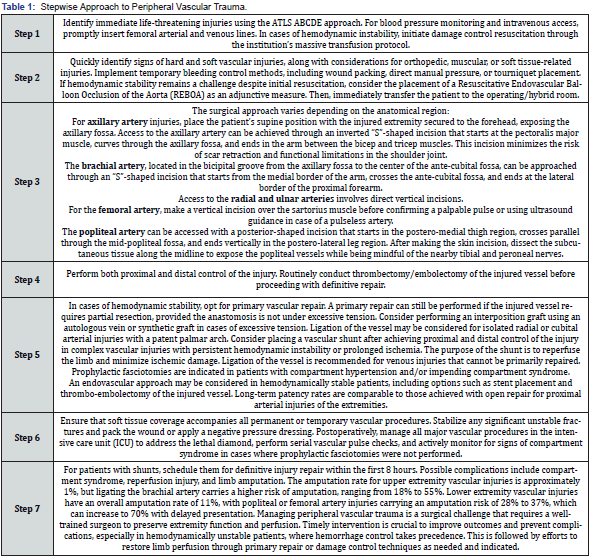
Treatment options for peripheral vascular trauma are tailored to the specific nature and severity of the injury. Management involves a systematic approach that encompasses initial stabilization, surgical intervention tailored to the anatomical location of the injury, achieving vascular control, and selecting repair techniques based on hemodynamic status. Complex cases may require vascular shunts, and an endovascular approach is suitable for stable patients. Timely and appropriate management is crucial to preserve limb function and prevent complications [29-31]. A stepwise management approach is shown in Table 1.
In hemodynamically unstable patients, immediate attention is given to addressing life-threatening injuries using the ABCDE approach of Advanced Trauma Life Support (ATLS) (American College of Surgeons, 2018) [29]. This includes securing airways, breathing, and circulation while initiating damage control resuscitation through the institution’s massive transfusion protocol to restore blood volume and prevent hypovolemic shock. Once the patient is stabilized, the focus shifts to identifying and managing the vascular injury. Surgical intervention becomes essential, and the choice of approach depends on the anatomical region affected. This may involve accessing the injured vessel through various incision techniques, including “S”-shaped incisions for axillary and popliteal arteries, vertical incisions for radial and ulnar arteries, and a vertical incision over the sartorius muscle for the femoral artery [32,33].
The next step is to achieve proximal and distal control of the injured vessel to prevent further hemorrhage. Thrombectomy or embolectomy of the injured vessel is performed routinely before proceeding with definitive repair. The choice of repair technique depends on the patient’s hemodynamic stability. Hemodynamically stable patients may undergo primary vascular repair, while partial resection may be considered if necessary, provided the anastomosis is not under excessive tension. Excessive tension may necessitate an interposition graft with an autologous vein or synthetic graft. Ligating the injured vessel may be appropriate in specific cases, such as isolated radial or cubital arterial injuries with a patent palmar arch [31,33].
Complex vascular injuries, especially those resulting in prolonged ischemia or persistent hemodynamic instability, may require the placement of a vascular shunt after achieving proximal and distal control. The purpose of the shunt is to reperfuse the limb and minimize ischemic damage [33]. In cases where venous injuries cannot be primarily repaired, vessel ligation may be necessary. Prophylactic fasciotomies are indicated in patients with compartment hypertension or impending compartment syndrome to prevent complications. An endovascular approach may be considered for hemodynamically stable patients, involving options such as stent placement and thrombo-embolectomy of the injured vessel. Long-term patency rates are comparable to open repair for proximal arterial injuries of the extremities [32,34].
Complications
Compartment Syndrome
Despite advancements in diagnostic technologies, diagnosing compartment syndrome, especially in high-risk injuries, remains a challenge without a clear consensus [35]. While measuring intracompartmental pressure is considered the gold standard when clinical signs are evident, there is a growing trend towards continuous pressure monitoring rather than relying solely on isolated pressure readings. This shift aims to provide a more comprehensive understanding of the evolving pressure dynamics within the affected compartment, which can be especially valuable in high-risk cases where early detection is critical.
Ongoing research efforts are directed toward refining diagnostic techniques and treatment strategies for compartment syndrome. Non-surgical or minimally invasive interventions, such as intermittent pressure pumps, tissue ultrafiltration, hyperbaric oxygen therapy, and targeted pharmacological approaches, are being explored to mitigate tissue damage and reduce the risk of irreversible consequences [36]. These innovative approaches promise to improve patient outcomes and preserve limb function, particularly in cases where rapid surgical intervention may be challenging or less effective.
In conclusion, despite the challenges in diagnosing compartment syndrome, the medical community actively seeks ways to enhance diagnostic accuracy and treatment efficacy. Continuous pressure monitoring and exploring non-surgical interventions represent promising avenues for addressing this complex condition [37,38].
Conclusion
This article provides a comprehensive overview of peripheral vascular trauma, encompassing its epidemiology, physiopathology, clinical presentation, diagnosis, treatment strategies, and potential complications. Peripheral vascular injuries, although relatively rare, contribute significantly to trauma-related fatalities. Most cases arise from penetrating trauma, with gunshot wounds and stabbings being prominent causes. Blunt trauma, while less common, also presents its own challenges. Understanding the physiopathology of vascular trauma is essential to grasp the complexities of diagnosis and management. Vascular injuries trigger events, including vessel wall damage, platelet aggregation, clot formation, inflammation, and tissue repair. These processes underscore the importance of timely intervention and effective treatment strategies. Clinical presentation plays a pivotal role in diagnosing peripheral vascular trauma, with soft and hard signs guiding the urgency of intervention. Early recognition and swift action are crucial, as delayed treatment can lead to severe complications, including limb loss. Diagnosis relies on clinical evaluation and various imaging studies, such as CTA, duplex ultrasonography, and MRA, to accurately identify and characterize vascular injuries. A multidisciplinary approach involving vascular surgeons and interventional radiologists is often necessary to determine the appropriate treatment approach. Treatment strategies vary depending on the nature and severity of the injury, with a focus on achieving vascular control and restoring blood flow. Complex cases may require vascular shunts or endovascular approaches. Prophylactic fasciotomies may also be necessary to prevent compartment syndrome.
Despite advancements in diagnostic technologies, the diagnosis of compartment syndrome remains a challenge, emphasizing the need for continuous pressure monitoring and exploration of non-surgical interventions to improve patient outcomes. In conclusion, this article aims to enhance medical understanding and promote effective clinical management of peripheral vascular trauma, emphasizing the critical importance of early recognition and intervention to preserve limb function and prevent life-threatening complications.
References
- Lisseth López-Narváez, Andrea Salazar-Trujillo, Juan F Cáceres-Sepúlveda, Cristian Rincón-Guio, José Daniel Charry-Cuellar (2019) Peripheral vascular trauma. A review of the literature. Cir Gen 41(3): 184-190.
- Mirdamadi N, Bakhtiari M, Baratloo A, Fattahi MR, Farshidmehr P (2022) An Epidemiologic Overview of Traumatic Vascular Injures in Emergency Department; a Retrospective Cross-Sectional Study. Arch Acad Emerg Med 10(1): e59.
- Huber GH, Manna B (20223) Vascular Extremity Trauma. In: StatPearls [Internet]. TIn urban trauma centers in the United States, peripheral vascular injuries are most reasure Island (FL): StatPearls.
- Liu JL, Li JY, Jiang P, Jia W, Tian X, et al. (2020) Literature review of peripheral vascular trauma: Is the era of intervention coming? Chin J Traumatol 23(1): 5-9.
- Frykberg ER, Schinco MA (2008) Peripheral vascular injury. In: Feliciano DV, Mattox KL, Moore EE, eds. Trauma. 6th edn. New York, NY: McGrawHill 941-971.
- Robbs JV, Baker LW (1988) Cardiovascular trauma. Curr Prob Surg. 1988 21:1-87.
- Cooper C, Rodriguez A, Omert L (1996) Blunt vascular trauma. Curr Prob Surg 29: 281-357.
- Rozycki GS, Tremblay LN, Feliciano DV, McClelland WB (2003) Blunt vascular trauma in the extremity: diagnosis, management, and outcome. J Trauma 55: 814-824.
- Feliciano DV (2016) Peripheral Vascular Injuries. In: Mattox KL, Moore EE, Feliciano DV, editors. Trauma, 8th edition. McGraw-Hill Education.
- Biffl WL, Smith WR, Moore EE, R J Gonzalez, S J Morgan et al. (2001) Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Ann Surg 233(6): 843-850.
- Inaba K, Demetriades D (2017) Management of Vascular Injuries. Surg Clin North Am97(5): 1085-1099.
- Fox CJ, Gillespie DL, O'Donnell SD, Rasmussen TE, James M Goff et al. (2005) The Contemporary Management of War-Related Vascular Trauma. J Vasc Surg 41(4): 638-644.
- Asensio JA, Trunkey DD (2001) Vascular Trauma. Surg Clin North Am 81(6): 1271-1295.
- Feliciano DV, Mattox KL, Moore EE. Trauma, 9th McGraw-Hill Education.
- FDV (2019) Management of peripheral arterial injuries. In: Feliciano DV, Mattox KL, Moore EE, editors. Trauma, 8th ed. McGraw-Hill Education.
- Fox N, Rajani RR, Bokhari F, William C Chiu, Andrew Kerwin et al. (2015) Evaluation and management of penetrating lower extremity arterial trauma: An Eastern Association for the Surgery of Trauma practice management guideline. Journal of Trauma and Acute Care Surgery, 78(4), 815-824.
- DuBose JJ, Savage SA, Fabian TC, Jay Menaker, Thomas Scalea, et al. (2012) The American Association for the Surgery of Trauma PRO spective Observational Vascular Injury Treatment (PROOVIT) registry: Multicenter data on modern vascular injury diagnosis, management, and outcomes. Journal of Trauma and Acute Care Surgery 73(3): 641-647.
- Asensio JA, Trunkey DD (2001) Management of Vascular Injuries. Surg Clin North Am 81(6): 1271-1295.
- Trunkey DD, Feliciano DV (2016) Peripheral Vascular Injuries. In: Mattox KL, Moore EE, Feliciano DV, editors. Trauma, 8th edition. McGraw-Hill Education.
- Biffl WL, Smith WR, Moore EE, Ricardo J. Gonzalez, Steven J. Morgan, et al. (2001) Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Ann Surg 233(6): 843-850.
- Fox CJ, Gillespie DL, O'Donnell SD, Rasmussen TE (2005) The Contemporary Management of War-Related Vascular Trauma. J Vasc Surg 41(4): 638-644.
- Inaba K, Demetriades D (2017) Management of Vascular Injuries. Surg Clin North Am 97(5): 1085-1099.
- Mattox KL, Moore EE (2021) Trauma, 9th edition. McGraw-Hill Education.
- Michael Rieger 1, Ammar Mallouhi, Thomas Tauscher, Martin Lutz, Werner R Jaschke (2011) Acute Arterial Injuries in Extremity Trauma: Diagnosis with 64-MDCT Angiography. AJR Am J Roentgenol 197(6): W931-937.
- Ricci MA, Trevisani GT, Pilcher DB, et al. (1991) Duplex sonography in penetrating extremity arterial trauma: a prospective study. J Vasc Surg 14(3): 350-358.
- Edelman RR, Hesselink JR, Zlatkin MB, Crues JV (2005) Clinical Magnetic Resonance Imaging.
- Feliciano DV, Mattox KL, Moore EE (2021) Trauma, 9th edition. McGraw-Hill Education.
- Goldberg HI, Gross E (1985) Digital Subtraction Angiography: Principles and Applications. Futura Publishing Company.
- El-Khoury GY, Eikelboom BC, Monteleone P (1988) Magnetic Resonance Imaging of the Musculoskeletal System.
- Cohen M J, (2018) American College of Surgeons. Advanced Trauma Life Support (ATLS) Student Course Manual (10th edn.).
- Khan M A, Raja A S, Cohen M J, Como J J, Cotton B A, et al. (2008) Damage control resuscitation in patients with severe traumatic hemorrhage: A practice management guideline from the Eastern Association for the Surgery of Trauma. Journal of Trauma and Acute Care Surgery 74(6): 1584-1595.
- Frykbergn E R, Crump J M, Vines F S (2001) Prognostic factors for the outcome of selective nonoperative management of blunt injury to the liver. Journal of Trauma and Acute Care Surgery, 51(6): 1015-1022.
- Moore E E, Mattox K L, Brunicardi F C (2018) Trauma (8th ed.). McGraw-Hill Education.
- Rajani R R, Bokhari F, Chiu W C, Kerwin A, Seamon M J, et al. (2004) Evaluation and management of penetrating lower extremity arterial trauma: An Eastern Association for the Surgery of Trauma practice management guideline. Journal of Trauma and Acute Care Surgery 56(4): 815-824.
- Healey MA, Dente C J (2017) Lower extremity vascular trauma. In R R, Bollinger K BMoore, W L Clancy (Eds.), Surgery: Basic Science and Clinical Evidence 3rd edn, 1045-1059.
- Ng J, Makaram N, Mitchell S (2019) Lessons learned in the challenging case of evolving compartment syndrome with atypical presentation. BMJ Case Rep 12(11): e231116.
- Novak M, Penhaker M, Raska P, Pleva L, Schmidt M (2022) Extremity compartment syndrome: A review with a focus on non-invasive methods of diagnosis. Front Bioeng Biotechnol 10: 801586.
- McMillan TE, Gardner WT, Schmidt AH, Johnstone AJ (2019) Diagnosing acute compartment syndrome-where have we got to? Int Orthop 43(11): 2429-2435.






























