Use of a Tourniquet in Lower Limb Amputations: Evaluating Blood Loss in Peripheral Arterial Disease Patients -A Systematic Review
Omar Eldurssi1*, Christo Kloppers2 and Wilbert Sibanda3
1Department of Surgery, Faculty of Health Science, University of Cape Town, South Africa
2Department of ACS, Groote Schuur Hospital, University of Cape Town, South Africa
3Nelson Mandela University, South Africa
Submission:November 20, 2022; Published:December 05, 2022
*Corresponding author: Omar Eldurssi, MMed (General surgery),FCS SA, Division of General Surgery, Faculty of Health Science, University of Cape Town Cape Town, South Africa
How to cite this article: Omar E, Christo K, Wilbert S. Use of a Tourniquet in Lower Limb Amputations: Evaluating Blood Loss in Peripheral Arterial Disease Patients -A Systematic Review. Open Access J Surg. 2022; 14(1): 555878 DOI: 10.19080/OAJS.2022.14.555878.
Abstract
Background: Tourniquets have become an inseparable part of many different types of intricate and major surgeries, including amputation. Tourniquets create a bloodless environment, which is thought to facilitate surgery and reduce time, potential errors and subsequent complications.
Objectives: To investigate the effectiveness of using a pneumatic tourniquet as an adjunct in lower limbs amputation in peripheral arterial disease to reduce blood loss and requirement for blood transfusions. Stump revision rate, complication and mortality will be assessed as secondary objectives.
Method: For this systematic review, a search was performed using the keywords phrases, “peripheral arterial disease”, “lower limb amputation” and “tourniquet” in PubMed, Medline, Embase and Google scholar, this work has been reported in line with PRISMA and AMSTAR guidelines.
Results: Based on univariate analysis, to determine the relationship between risk factors and blood loss, the study demonstrated the use of tourniquet significantly reduces the amount of blood loss during lower limb amputation (LLA), F (21.01), P=0.044. An independent t -test demonstrated that there was a statistically significant difference in mean blood loss between tourniquet and non-tourniquet studies, (T=-2.588, P=0.049). In this review the mean blood loss was 251.67±2.89 and 462.5±137.69ml for tourniquet and non-tourniquet studies respectively.
Conclusion: Using a tourniquet is a technically feasible approach to LLA, and effectively reduces the amount of blood loss and requirements of blood transfusion. No change in revision rates were noted.
Keywords: Tourniquet; Blood loss; Revision; Amputation; Lower limb; Pain
Abbreviations: PRISMA-P: Preferred Reporting Items for Systematic Reviews and Meta- analysis for Protocol; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; AMSTAR: Assessing the Methodological Quality of Systematic Reviews; RCTs: Randomized Controlled Trials; PAD: Peripheral Arterial Disease; DM: Diabetes Mellitus; LLA: Lower Limb Amputation
Background and Aim
Major limb amputation is a common surgical operation for patients with diabetic foot sepsis and critical limb ischemia who failed or are not candidates for revascularization. These patients often have significant co morbidities and outcomes are generally guarded. Post-operative hemorrhage is a common complication that can occur after any surgical procedure. A tourniquet is a device that prevents blood flow in the limbs and has the advantage of improving the surgical field and decreasing the blood loss Its usage is universal, but many controversies remain about it and with passage of time some principles have changed. In general, there are two types of tourniquets, namely surgical and emergency. Surgical tourniquets are used in orthopedic and plastic surgeries for creation of a bloodless field, greater safety, better precision, and convenience for the surgeon. Another use of the tourniquet is as an adjunct for regional anesthetic. Emergency tourniquets are used out of hospital to control traumatic bleeding in limbs. A tourniquet can be either pneumatic or elastic (Esmarch). In recent times, most tourniquets are of the pneumatic design. Currently the use of a tourniquet during amputation is not universally practiced, mostly due to surgical anecdote. With this review we aim to evaluate the current literature on the use of a tourniquet to prevent blood loss during amputation.
Methods
Protocol and Registration
The study is reported according to the Preferred Reporting Items for Systematic Reviews and Meta- analysis for Protocol (PRISMA-P) [1]. The work has been reported in line with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta- Analyses) with Registration number: CRD42021231657 and AMSTAR (Assessing the Methodological Quality of Systematic Reviews) Guidelines.
Statement of Human Rights and Ethics
This is a systematic review and does not involve patients directly. The protocol has been approved by the local institutional ethic committee (HREC/ REF/512/2020).
Eligibility Criteria
Randomized controlled trials (RCTs) and retrospective studies comparing tourniquet with non-tourniquet amputations of the lower limb, for patients aged 18 and above, with peripheral arterial disease (PAD), with the following risk factors, diabetes mellitus (DM), HPT, smoking, hyperlipidemia, and HIV.
Information Sources
Two review authors searched the PubMed, Cochrane, Google Scholar Library and EmBase databases for all results.
Search
A simple, but exhaustive keyword search was performed using the keyword “tourniquet” in EmBase and as a MeSH term in PubMed. Other keywords used were amputations with tourniquet, peripheral arterial disease (PAD), blood loss, Amputation.
Study Selection Criteria
The search results were captured on an online data repository. Two review authors independently reviewed all results, based on the study inclusion and exclusion criteria. Any discrepancies for each step were resolved before proceeding to the next step. Extracted articles were first evaluated for the title, abstract and the complete manuscript to assess eligibility as per PRISMA flow diagram. Non-English articles were excluded.
Data Collection Process
All data collected will be put on a separate sheet under the last name of the first author, year, size of population, median age, country, and type of operation. One author developed the data capture repository, while the other author extracted the relevant data.
Data Items
Primary data extraction concerned only patients with peripheral arterial disease (PAD), who underwent lower limb amputation (LLA), with tourniquet. Secondary data extraction concerned lower limb amputation outcomes such as blood loss, revision rate, operative time, complication, and mortality. Other variables collected were country of study, study design, number of participants and characteristics of study participants (age, sex, fracture type and length of stay in hospital) and operation characteristics (data on the use of a tourniquet and surgery duration).
Summary Measures
Primary outcomes, blood loss, revision rate, operative time, number of complications and mortality were reported across the studies. A p-value < 0.05 was considered statistically significant. Statistical analysis was performed using the SPSS version 26 software.
Study Selection
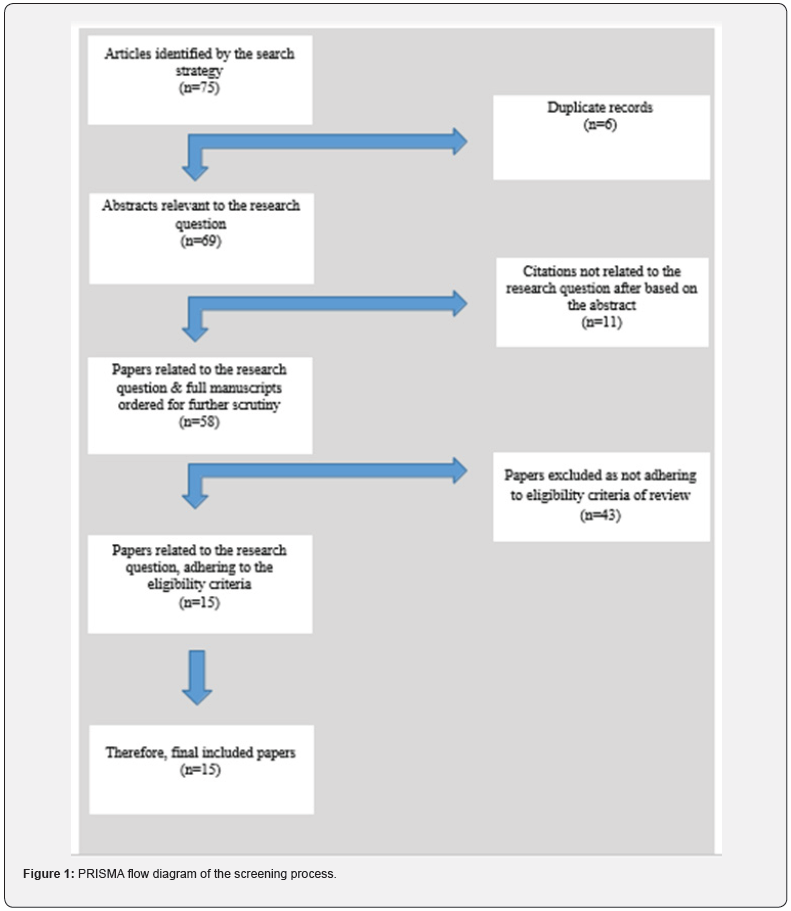
The study selection process is outlined in the Preferred Reporting Items for Systematic Reviews (PRISMA) diagram (Figure 1). A total of 75 articles were identified during the initial search. After removal of six duplicate records remaining with 69. A further review of the 69 abstracts resulted in the removal of 11 citations that were not related to the research, giving 58 full manuscripts that were related to the research question. Screening the remaining 58 manuscripts based on the minimum eligibility criteria excluded 43 articles that did not meet the minimum eligibility criteria. A total of 15 full manuscripts met the minimum eligibility criteria.
Results Synthesis
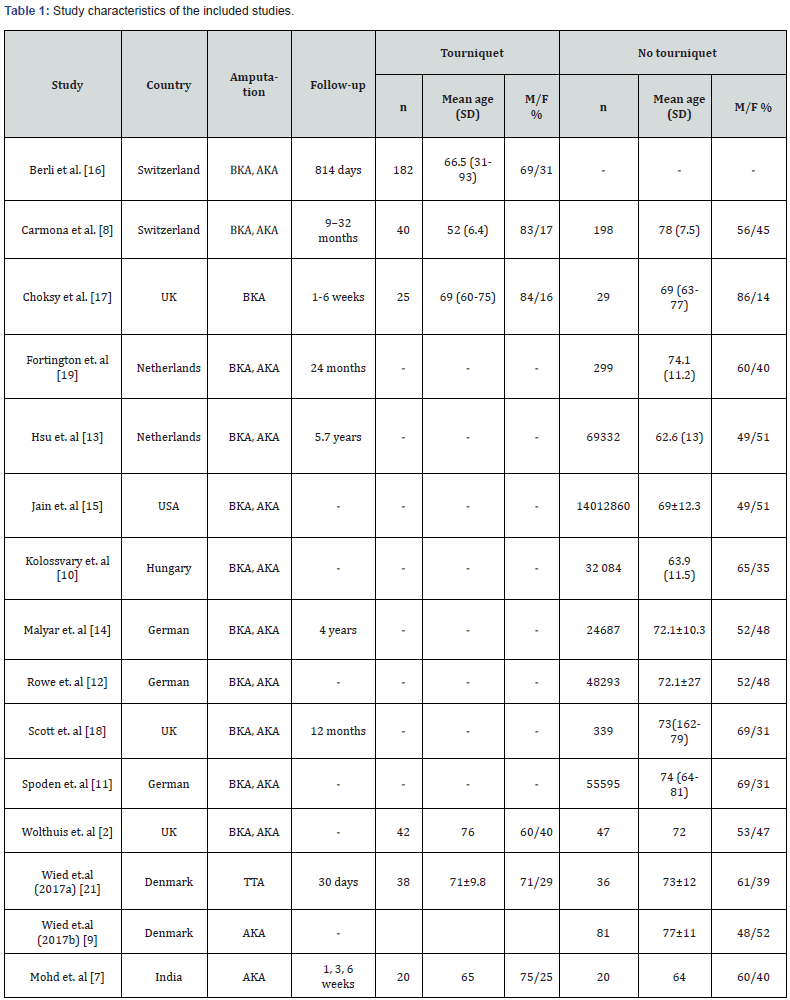
Fifteen studies met the minimum inclusion criteria and were included in this systematic review as shown in Table 1. The number of participants ranged from 42 to 138 and except for one study [2] there was a surplus of males included. Amputations among men were higher compared to women, 11 studies showed (92%) amputations among men were above 50% and five studies (42%) amputations were above 60% compared to women. Prevalence of DM varied between 35% and 58% for the 15 studies.
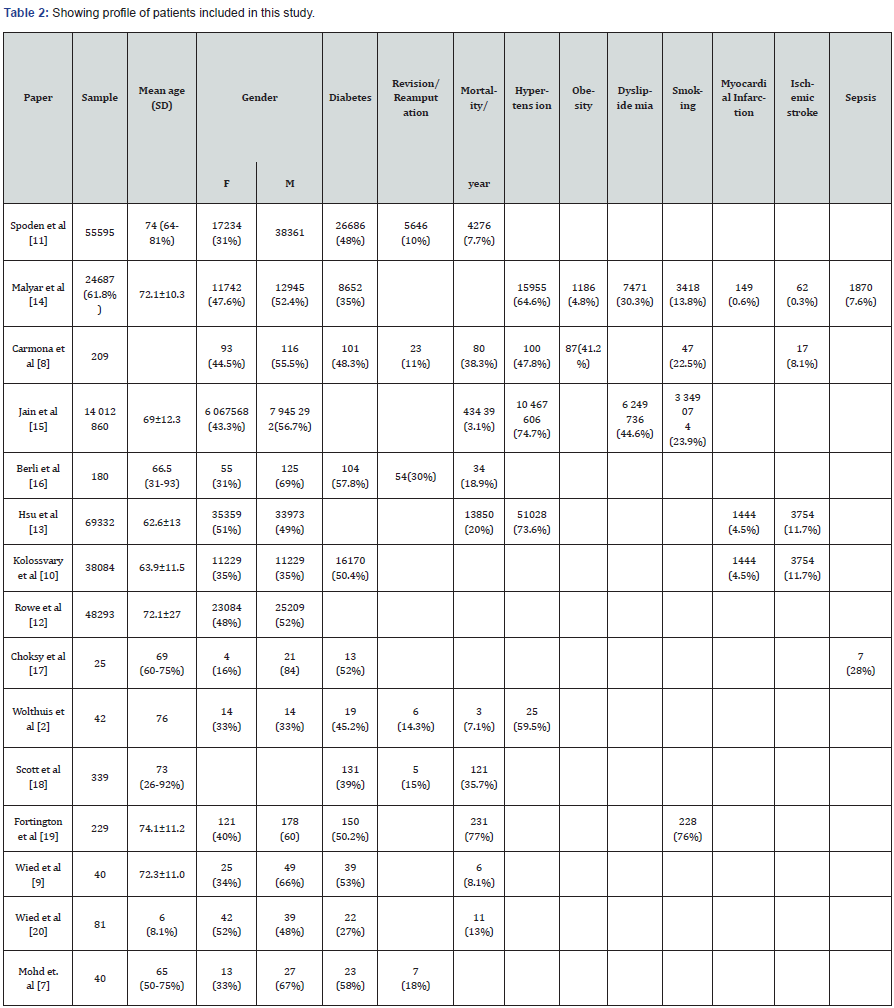
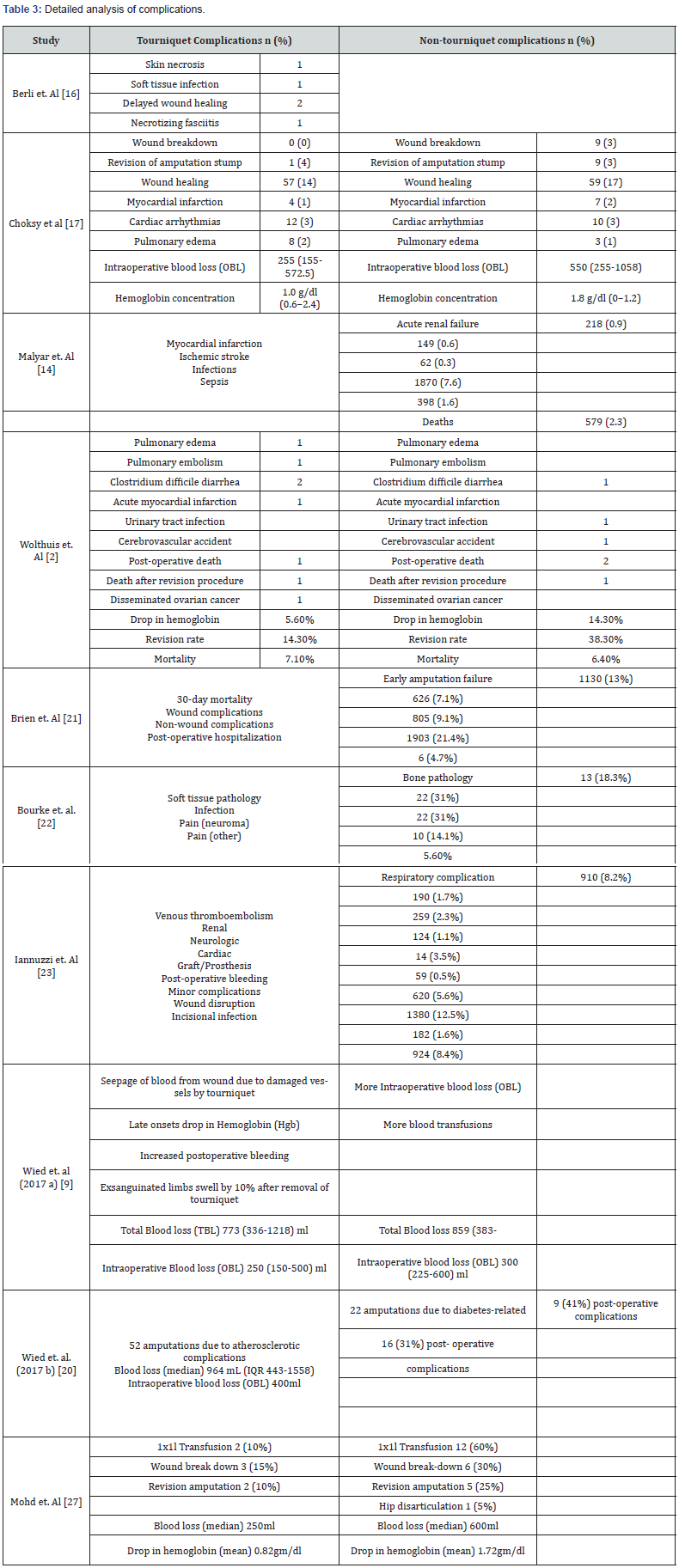
In this systematic review, one article reported on re-operation after lower limb amputation in PAD patients [1], three articles [3-5] on the role of diabetes in increasing the risk of LLA in PAD patients, two articles on application of tourniquets to reduce blood loss in LLA in PAD patients [6,7], two articles on mortality rate after LLA for PAD patients [8,9] and three articles on trends in LLA for PAD patients [2,10,11]. A detailed analysis of profile of patients in the studies and complications associated with LLA surgery is given in Table 2 & Table 3 respectively. By using univariate analysis to determine the relationship between risk factors and blood loss, the study demonstrated the use of a tourniquet significantly reduces the amount of blood loss during lower limb amputation, F = 21.01, P = 0.044 (Table 4). An independent t -test, demonstrated that there was a statistically significant difference in mean blood loss between tourniquet and non-tourniquet studies, (T= -2.588, P= 0.049). The mean blood loss was 251.67±2.89 and 462.5±137.69 milliliter for tourniquet and non-tourniquet studies respectively.

Discussion
In this systematic review, there were studies suggesting that PAD stage was not predictive of the need for revision surgery [1]. In a study by Carmona in Geneva between the year 1990 and 1999, the rate of amputation for PAD patients increased from 1.8 to 11.4/10 000 patients/year and the increase was observed to be associated with age and male gender of patients [3]. In addition, this group demonstrated that diabetes was present in 48% of patients, conferring a 10 times risk of lower limb amputation (LLA). In the same cohort it was demonstrated that major lower limb amputation has a poor prognosis, characterized by 40% mortality in a two-year period. Another study by Scott, similarly, showed that major lower limb amputation is a high-risk procedure with a high 30-day mortality of 12.4% and that an increase in age was associated with an increase in the risk of mortality following LLA for PAD patients [12]. Rowe et al reported that there was an association between increased application of endovascular technology and reduced rates of amputation in patients with PAD [13].
Jain [14] demonstrated that individuals with PAD and DM1 are more likely to be amputated compared to PAD and DM2 (17.7% vs 10.6%). However, PAD and DM2 patients were observed to be older than PAD and DM1. Kolossvary reported that 50.4% of LLA for PAD had diabetes [2]. In a study by Wolthuis [2] the drop in hemoglobin following surgery was higher among nontourniquet patients (14.8%) compared to tourniquet patients (5.6%), with a higher need for transfusion in the non-tourniquet group. The revision rate was 14.3% in the tourniquet group and significantly higher in the non-tourniquet group (38.3%) [7]. Interestingly, according to this work, mortality was higher among tourniquet (7.1%) than non-tourniquet patients (6.4%), however the difference in mortality was not statistically significant, P = 0. 895. According to Choksy intraoperative blood loss was higher among non-tourniquet patients; 550 (255-1058) ml compared to tourniquet patients 255 (155-572.5) ml [6]. In addition, there was a significantly greater drop in hemoglobin concentration (median and IQR) in non-tourniquet compared to the tourniquet group (1.8 g/dl (0–1.2) vs1.0 g/dl (0.6–2.4) and the difference was statistically significant, P = 0.035. Therefore, the requirement for blood transfusion was lower in the tourniquet group. The rate of wound healing, breakdown and revision were similar in the tourniquet and non-tourniquet groups, respectively (59 vs 57%, 0 vs 9%, 14 vs 9%) [15-26].
Conclusion
The study provides valuable insight into the differences between tourniquet and non-tourniquet for lower limb amputations, with respect to outcomes such as blood loss (both intraoperative blood loss and total blood loss), revision rate, operation time, complications and mortality. However, not all the studies provide the entire list of outcomes. The weakness of the study is that there is a paucity of randomized control studies (RCTs) investigating tourniquet use in lower limbs amputation in PAD patients. We recommend doing more prospective investigation for lower limb amputations.
References
- McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 88: 105906.
- Wolthuis AM, Whitehead E, Ridler BM, Cowan AR, Campbell WB, et al. (2006) Use of a pneumatic tourniquet improves outcome following trans-tibial amputation. Eur J Vasc Endovasc Surg 31(6): 642-645.
- Saied A, Mousavi AA, Arabnejad F, Heshmati AA (2015) Tourniquet in surgery of the limbs: a review of history, types, and complications. Iran Red Crescent Med J 17(2): 9588.
- Lu CW, Chen YS, Wang MJ (2004) Massive pulmonary embolism after application of an Esmarch bandage. Anesth Analg 98(4): 1187-1189.
- Murphy C, Winter D, Bouchier-Hayes D (2005) Tourniquet injuries: pathogenesis and modalities for attenuation. Acta Orthop Belg 71(6): 635.
- Sharma JP, Salhotra R (2012) Tourniquets in orthopedic surgery. Indian J Orthop 46: 377-383.
- Mohd J, Lone ZA, Singh A (2019) A prospective randomized controlled study for assessment of use of pneumatic tourniquet in above knee amputation of ischemic limb in peripheral vascular disease. The Indian Journal of Applied Research 9(7): 25-26.
- Carmona GA, Hoffmeyer P, Herrmann FR, Vaucher J, Tschopp O, et al. (2005) Major lower limb amputations in the elderly observed over ten years: the role of diabetes and peripheral arterial disease. Diabetes Metab 31(5): 449-454.
- Wied C, Tengberg PT, Holm G, Kallemose T, Foss NB, et al. (2017) Tourniquets do not increase the total blood loss or re-amputation risk in transtibial amputations. World J Orthop 8(1): 62.
- Kolossváry E, Ferenci T, Kováts T, Kovács L, Járai Z, et al. (2015) Trends in major lower limb amputation related to peripheral arterial disease in Hungary: a nationwide study (2004–2012). Eur J Vasc Endovasc Surg 50(1): 78-85.
- Spoden M, Nimptsch U, Mansky T (2019) Amputation rates of the lower limb by amputation level–observational study using German national hospital discharge data from 2005 to 2015. BMC Health Serv Res 19(1): 1-9.
- Rowe VL, Lee W, Weaver FA, Etzioni D (2009) Patterns of treatment for peripheral arterial disease in the United States: 1996-2005. J Vasc Surg 49(4): 910-917.
- Hsu CY, Chen YT, Su YW, Chang CC, Huang PH, et al. (2017) Statin therapy reduces future risk of lower-limb amputation in patients with diabetes and peripheral artery disease. J Clin Endocrinol Metab 102(7): 2373-2381.
- Jain N, Agarwal MA, Jalal D, Dokun AO (2020) Individuals with peripheral artery disease (PAD) and type 1 diabetes are more likely to undergo limb amputation than those with PAD and type 2 diabetes. J Clin Med 9(9): 2809.
- Malyar NM, Freisinger E, Meyborg M, Lüders F, Gebauer K, et al. (2016) Amputations and mortality in in-hospital treated patients with peripheral artery disease and diabetic foot syndrome. J Diabetes Complications 30(6): 1117-1122.
- Berli MC, Wanivenhaus F, Götschi T, Böni T, Rancic Z, et al. (2019) Predictors for reoperation after lower limb amputation in patients with peripheral arterial disease. Vasa 48(5): 419-424.
- Choksy SA, Chong PL, Smith C, Ireland M, Beard J (2006) A randomized controlled trial of the use of a tourniquet to reduce blood loss during transtibial amputation for peripheral arterial disease. Eur J Vasc Endovasc Surg 31(6): 646-650.
- Scott SW, Bowrey S, Clarke D, Choke E, Bown MJ, et al. (2014) Factors influencing short‐and long‐term mortality after lower limb amputation. Anesthesia 69(3): 249-258.
- Fortington LV, Geertzen JH, van Netten JJ, Postema K, Rommers GM, et al. (2013) Short- and long-term mortality rates after a lower limb amputation. Eur J Vasc Endovasc Surg 46(1): 124-131.
- Wied C, Tengberg PT, Kristensen MT, Holm G, Kallemose T, et al. (2017) Total blood loss after transfemoral amputations is twice the intraoperative loss: an observational cohort study of 81 nontraumatic amputations. Geriatr Orthop Surg Rehabil8(3): 123-127.
- O'Brien PJ, Cox MW, Shortell CK, Scarborough JE (2013) Risk factors for early failure of surgical amputations: an analysis of 8,878 isolated lower extremity amputation procedures. J Am Coll Surg 216(4): 836-842.
- Bourke HE, Yelden KC, Robinson KP, Sooriakumaran S, Ward DA (2011) Is revision surgery following lower-limb amputation a worthwhile procedure? A retrospective review of 71 cases. Injury 42(7): 660-666.
- Iannuzzi JC, Chandra A, Rickles AS, Kumar NG, Kelly KN, et al. (2013) Resident involvement is associated with worse outcomes after major lower extremity amputation. J Vasc Surg 58(3): 827-831.
- Noordin S, McEwen JA, Kragh Jr CJ, Eisen A, Masri BA (2009) Surgical tourniquets in orthopedics. J Bone Joint Surg 91(12): 2958-2967.
- Klenerman L (1962) The tourniquet in surgery. J Bone Joint Surg Br 44(4): 937-943.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 62(10): e1- 34.






























