Preoperative Imaging Continues to Lower Negative Appendicectomy Rates (NAR)-A Retrospective Analysis of a Tertiary Health Service in Australia
Matthew Corbitt1,2* and Michelle Cooper2,3
1 Department of Surgery, Cairns and Hinterland Hospital and Health Service, Australia
2 School of Medicine & Dentistry, Griffith University, Australia
3 Staff Specialist, Gold Coast Health Service, Australia
Submission:February 26, 2022; Published:March 14, 2022
*Corresponding author: Matthew Corbitt, Department of Surgery, Cairns and Hinterland Hospital and Health Service, Australia
How to cite this article: Matthew C, Michelle C. Preoperative Imaging Continues to Lower Negative Appendicectomy Rates (NAR)-A Retrospective Analysis of a Tertiary Health Service in Australia. Open Access J Surg. 2022; 13(5): 555873 DOI: 10.19080/OAJS.2022.13.555873.
Abstract
Aim: To analyze the Negative Appendicectomy Rate (NAR) in a single tertiary health service, compare it to published data and analyze the impact of pre-operative imaging in acute appendicitis.
Methods: A retrospective cohort study of a single health service was performed for a single year. Search terms included ‘diagnostic laparoscopy’ and ‘appendicectomy’ (both laparoscopic and open). Demographic data was extracted. The primary outcome was NAR. Secondary outcomes included tumour incidence and imaging modality accuracy as defined by NAR. Data was excluded if there was no histopathological report available.
Results: A total of 820 cases were identified, with 736 operations being performed for suspected appendicitis. A total of 633 booked laparoscopic appendicectomies were included for analysis, yielding an NAR of 11.2%. Overall tumour incidence was calculated at 1.5%. No preoperative imaging, or cases which utilized ultrasound as the only imaging modality, produced NARs of 19.3% and 17.4% respectively. Use of Computed Tomography (CT) in males under 40 was associated with lower NAR (3.0%, p=0.01) but no statistical difference was found between no imaging and ultrasound-only in this age group. Ultrasound-only was better than no imaging for females of all ages (p<0.001) and CT alone did not improve NAR in those under 40 years old (p>0.05). Preoperative CT was overall statistically significant at correctly identifying appendicitis (OR 2.80, p<0.001), giving an NAR of 7.1%.
Conclusion: This study’s NAR is better than accepted rates, however, is still high when compared internationally. There is great potential in the use of preoperative imaging to further guide correct diagnosis and operative patient selection.
Keywords: Negative Appendicectomy Rate; Radiology; Ultrasound; Computed Tomography
Introduction
Appendicectomies are the most common surgical operation performed, with approximately 29,000 being performed in Australia each year and the laparoscopic approach being the gold standard [1]. The diagnosis of acute appendicitis can be made on both clinical and radiological grounds and while there is ongoing debate regarding the role of conservative management, the standard of care remains to be surgical. Negative Appendicectomy Rate (NAR), defined as the proportion of histologically normal appendices removed in patient’s suspected of having acute appendicitis, is the clinical measure used to determine how effective a surgical service is in detecting appendicitis. Rates of up to 25% have been deemed acceptable, with even higher rates in females due to gynecological pathologies mimicking appendicitis and clouding the clinical picture [2,3]. In 2017, a multicenter audit of emergency appendicectomies in Australia determined the NAR to be 19.0%, with higher NAR in females (24.9%) than males (13%) [1]. This is comparable to the United Kingdom (U.K.), which is reportedly 20.6% [1]. however, values vary widely [4]. The primary outcome of this retrospective analysis was NAR for 2018 at a single health service in Australia, which included a secondary and tertiary hospital. Secondary outcomes included tumour incidence and accuracy of imaging modalities utilized.
Methods
Data from the Gold Coast Health service (GCUH and Robina Hospital) in 2018 was retrospectively collected from the Operating Room Information System (ORMIS) database and respective electronic medical records were then analyzed. Search terms included ‘diagnostic laparoscopy’ and ‘appendicectomy’ (laparoscopic and open). This also included partial caecectomy as all cases were booked as appendicectomies first, and subsequently progressed to partial caecectomy as an intraoperative decision rather than a pre-operative one. Data extracted included: patient age, sex, service specialty (general surgery, pediatric surgery), emergency or elective operation, length of hospital stay, imaging used in workup and appendix/operative specimen histopathology. All patient’s aged 14 years and older were included. Patient’s aged 13 years or younger are treated as pediatric at our institution and were excluded from the study as the clinical history and imaging results are less reliable. The primary outcome was Negative Appendicectomy Rate (NAR). Secondary outcomes were tumour incidence and accuracy of imaging modalities used. Negative Appendicectomy Rate was calculated both by dividing the number of pathological normal appendices by the total number of cases, as well as number of booked appendicectomies performed to measure clinical judgement. Cases were excluded if there was no histology report available on the medical record, the appendix was not removed (for any reason) or the case was initially booked by gynecology.
Data analysis was performed with R statistics package (R Core Team, New Jersey, USA). Multivariable logistic regression modelling was undertaken to determine the factors impacting the negative appendicectomy rate. Significance was determined at p<0.05.
Results
Demographics
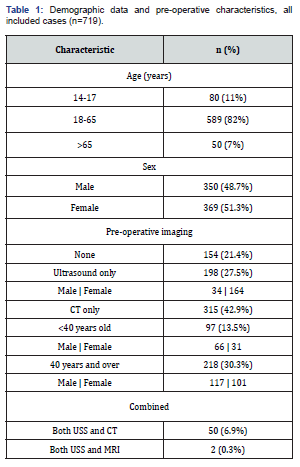
The ORMIS data identified 820 cases for analysis in 2018. There were 635 laparoscopic appendicectomies booked by general surgery for a suspected or provisional diagnosis of appendicitis, including 7 booked by Paediatric surgery which met our inclusion criteria. General surgery also booked 101 diagnostic laparoscopies. No open appendicectomies were booked. The remainder of the cases were managed by gynecology. There were 706 booked as emergency operations and 30 booked as elective, however, 13 of the elective cases were incorrectly coded and were included in the analysis. The remaining 17 cases were excluded as they were booked as either interval appendicectomies (n=11), or as another operation but progressed to appendicectomy after an unexpected intra-operative finding. There were 80 cases for patient’s aged 14-17 years old (11%), 589 for ages 18-65 (82%), and 50 for over 65 years old (7%) with the average age being 36 years old (rage: 14-89). Males comprised 350 cases (48.7%) and females 369 cases (51.3%). The average length of stay was 2.76 days (range: 0-57). No imaging was performed in 154 (21.4%) cases and an ultrasound (USS) was performed in 198 (27.5%) cases. Computed Tomography (CT) was used in 315 cases (43.8%), where 209 were for patients aged 40 years and over (66.3%) as patient’s younger than this are not routinely imaged with CT at our institution. Both USS and CT were used in 50 cases (6.9%). Only two cases used both USS and magnetic resonance imaging (MRI) preoperatively and both were for pregnant patients. See (Table 1) for further breakdown of case demographics.
Operative characteristics
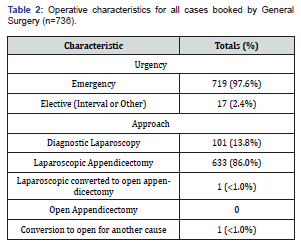
Emergency cases comprised of 98% of the data, with 86% being laparoscopic appendicectomies (Table 2). There was one laparoscopic converted to open appendicectomy and one other procedure that was converted to open for a malignant intra-operative finding. No cases were booked as open appendicectomy.
Primary outcome – NAR
Histopathological acute appendicitis was reported 639 times, giving a Negative Appendicectomy Rate (NAR) of 11.2% for all cases (n=717). However, of the 96 cases that were not appendicitis, 37 (46.2%) had an alternative diagnosis found on histopathology. The remaining 43 cases returned a normal appendix on histopathology and no alternative diagnosis was found. Two cases were excluded from the NAR calculation due to no available histology report and an abandoned operation. The NAR in males and females was also calculated, with a slightly higher rate found in females (12.9%, n=36, p>0.05) compared with males (10.9%, n=37).
Secondary outcomes
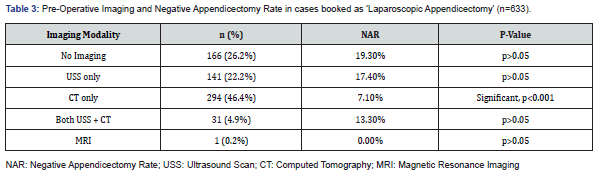
Imaging use and accuracy: In cases booked as laparoscopic appendicectomy, no imaging was performed pre-operatively in 26.2% (n=166) of cases, yielding a NAR of 19.3% (p>0.05). Ultrasound scanning and CT scanning alone were utilized in 22.2% (n=141) and 46.4% (n=294) of cases respectively, giving NARs of 17.4% (p>0.05) and 7.1% (OR 2.80, p<0.001). Cases which used both ultrasound and CT had an NAR of 13.3% and one case that used MRI correctly identified appendicitis (Table 3). Males were more likely to proceed to an operation without any imaging (86%, n=122), whereas females were more likely to have an ultrasound (79.4%, n=112). Receiving imaging of any kind was more likely to result in a correct histopathological diagnosis of appendicitis (OR 1.73, p<0.001). Female NARs were calculated: no imaging (45%), ultrasound-only under 40 years old (17.8%), ultrasound-only aged 40 and over (0%), CT-only under 40 years old (19.4%) and CT-only aged 40 and over (1.0%) (Table 4). Male NARs were calculated: no imaging (11.5%), ultrasound-only under 40 years old (20.7%), ultrasound-only aged 40 years and over (0%), CT-only under 40 years old (3.0%) and CT-only aged 40 years and older (11.1%) (Table 4). Overall, ultrasound-only was better than no imaging for females of all ages (p<0.001), however, CT-only was not better than ultrasound-only for females under 40 years (p>0.05). By comparison, CT-only for males under 40 years was better at correctly identifying acute appendicitis than ultrasound only (p=0.01). No statistical difference was found between males under 40 years who received no imaging compared with ultrasound (p>0.05). NAR, Negative Appendicectomy Rate; USS, Ultrasound Scan; CT, Computed Tomography.
Tumour incidence and meckel’s diverticulum: The overall rate of incidental malignancy was 1.5% (11/736), with approximately 50% of these being neuroendocrine tumours (n=6). The rate of Meckel’s Diverticulum identified was 0.5% (4/736).
Discussion
This single center, retrospective study again demonstrates the relatively high Negative Appendicectomy Rate (NAR) in an Australian hospital, with the calculated rate being 11.2%. While this still falls below previously published acceptable rates of 15-25% [2, 3]. our NAR is still remarkably high when compared with the United States, the Netherlands and Japan, which have reported rates as low as 4.5%, 3.3% and 2.5% respectively [5-7]. Our NAR from clinical diagnosis alone was 19.3%, which is comparable with average rates throughout Australia (19.0%), the United States (19.2%) and the United Kingdom (20.6%) [1, 5]. In 2017, a multicenter Australian study conducted by Arthur, et al. suggested that this higher NAR in Australia compared with other countries was due to low rates of preoperative imaging [1]. Approximately 76% of our patient’s (n=467) in this study underwent preoperative imaging, which is a significant improvement in this previously reported rate of 65% [1]. Moreover, the NAR rate in patients who underwent USS only was significantly less than the reported Australian average (17.4% vs. 35.7%), and our NAR with CT was comparable (7.1% vs. 6.7%). Additionally, CT scanning preoperatively in this study was significant for correctly identifying appendicitis when compared to no preoperative imaging, as was using any imaging compared with none. Ultrasound-only was better than no imaging for females of all ages (p<0.001) but no difference was found for males in the under 40 age group. This is likely because an ultrasound in females is useful for assessing for gynecological pathology, as well as appendicitis [8]. Additionally, ultrasound is further limited by significant inter-rater reliability, patient anatomy and sonographer experience [9]. However, CT-only was identified as better than ultrasound-only in males under 40 years (p=0.01), whereas there was no statistical difference for females in this category. Regardless, our rates of preoperative imaging were still far lower than those seen in the Netherlands or the United States. In 2015, 99.7% of patients in the Netherlands had preoperative imaging and nearly one-third underwent Computed Tomography (CT). Furthermore, CT utilization in the United States has been reported as high as 86.1%, yielding a NAR of 2.5% [5]. Compared with the reported Australian averages, the use of CT in our health service was greater (52.0% vs. 33.0%), and this higher use of preoperative imaging correlated with a lower NAR (11.2% vs. 18.1%). Some of the reservation with using imaging stems from acute appendicitis traditionally being a clinical diagnosis, with imaging only being used in cases where there is diagnostic uncertainty. A more reliable approach would be consistent application of the Alvarado scoring system, which has Grade IA evidence in determining which patients should undergo pre-operative imaging as recommended by the World Society of Emergency Surgery guidelines [10]. Furthermore, radiation use in younger patients has often been avoided for fear of long-term radiation exposure related complications. However, research has shown that a standard abdominal CT would give a 0.02-lifetime attributable risk of cancer in a 35-year-old compared with baseline. Additionally, a Cochrane review published in 2019 found that in adults there was negligible difference in sensitivity or specificity between low-dose and standard-dose CT abdomen/pelvis, and that contrast use was the only factor that increased sensitivity in diagnosing acute appendicitis [11]. Similar results regarding low-dose CT were also found in a 2004 study, then again in a 2018 study [12, 13]. This is largely due to the advent multiplanar reformatting techniques.
A recent UK study has also proposed that the use of preoperative imaging in appendicitis with a subsequent reduction of NAR by 15% would have lowered the cost to their health service to approximately 10% of the actual cost of progressing to an operation on clinical grounds alone, depending on the imaging modality used [14]. Similar results have also been reported elsewhere [15]. This study has some inherent limitations, the largest being that it is retrospective analysis of a single health service over a one-year period, and it would be difficult to make any conclusions drawn from this data generalizable to other Australian hospitals. Secondly, as clinicians we treat patients, and this study despite the high NAR, does not report on resolution of symptoms post appendicectomy. A follow-up study in this area could be of value. Also, the “NAR” definition appears to vary in several studies, making accurate comparisons more difficult and likely over-exaggerating the utility of radiological imaging in lowering NAR.

Conclusion
Acute appendicitis is a common surgical problem where the current gold standard in management is laparoscopic appendicectomy. Acute appendicitis is traditionally a clinical diagnosis with imaging only being used in instances of diagnostic uncertainty. Negative appendicectomy rate has previously been reported acceptable as high as 25%, however, rates worldwide are significantly decreasing as there is a shift toward preoperative imaging. In Australia, we still have high NAR’s comparatively, however, results from our hospital demonstrate this may be changing as we continue to increase our rates of preoperative imaging.
Declarations
No funding was used in this research. The authors declare no conflicts of interest. No ethics approval was required to undertake this retrospective analysis.
References
- Arthur T, Gartrell R, Manoharan B (2017) Emergency appendicectomy in Australia findings from a multicenter, prospective study. ANZ Journal of Surgery 87: 656-660.
- Raja AS, Wright C, Sodickson AD, Richard D Zane, Gordon D Schiff, et al. (2010) Negative Appendectomy Rate in the Era of CT: An 18-year Perspective. Radiology 256: 460-465.
- Webb EM, Nguyen A, Wang ZJ, Joseph W Stengel, Antonio C Westphalen, et al. (2011) The Negative Appendectomy Rate Who Benefits From Preoperative CT?. American Journal of Roentgenology 197: 861-866.
- Lim J, Pang Q, Alexander R (2016) One-year negative appendicectomy rates at a district general hospital: A Retrospective Cohort Study. International Journal of Surgery 31: 1-4.
- Tseng J, Cohen T, Melo N, Alban RF (2019) Imaging utilization affects negative appendectomy rates in appendicitis: An ACS-NSQIP study. The American Journal of Surgery 217: 1094-1098.
- Van Rossem CC, Bolmers MDM, Schreinemacher MHF (2015) Prospective nationwide outcome audit of surgery for suspected acute appendicitis. British Journal of Surgery 103: 144-151.
- Sugiura K, Miyake H, Nagai H, Yuichiro Y, Koji S, et al. (2020) Chronological Changes in Appendiceal Pathology Among Patients Who Underwent Appendectomy for Suspected Acute Appendicitis. World Journal of Surgery 44: 2965-2973.
- Javidi Parsijani P, Pourhabibi Zarandi N, Paydar S (2013) Accuracy of Ultrasonography in Diagnosing Acute Appendicitis. Bulletin of Emergency and Trauma. 1: 158-163.
- Heverhagen JT, Pfestroff K, Heverhagen AE, Klaus JK, Katharina K, et al. (2012) Diagnostic accuracy of magnetic resonance imaging: A prospective evaluation of patients with suspected appendicitis (Diamond). Journal of Magnetic Resonance Imaging 35: 617-623.
- Di Saverio S, Podda M, De Simone B, Marco Ceresoli, Goran Augustin, et al. (2020) Diagnosis and treatment of acute appendicitis 2020 update of the WSES Jerusalem guidelines. World Journal of Emergency Surgery 15: 27.
- Rud B, Vejborg TS, Rappeport ED (2019) Computed tomography for diagnosis of acute appendicitis in adults. Cochrane Database of Systematic Reviews.
- Keyzer C, Tack D, De Maertelaer V, Pascale B, Pierre Alain G, et al. (2004) Acute Appendicitis: Comparison of Low-Dose and Standard-Dose Unenhanced Multi Detector Row CT. Radiology 232: 164-172.
- Stephenson J, Al Nowfal A, Khatiwada AS, Zhia Lim, Mike Norwood, et al. (2018) Can imaging have a beneficial effect on reducing negative appendicectomy rates. Clinical Radiology 73: e21.
- Chan J, Fan KS, Mak TLA, Sook Yin Loh, Ravi Adapala, et al. (2020) Pre-Operative Imaging can Reduce Negative Appendectomy Rate in Acute Appendicitis. Ulster Medical Journal 89: 25-28.
- D’Souza N, Marsden M, Bottomley S, N Nagarajah, F Scutt, et al. (2018) Cost-effectiveness of routine imaging of suspected appendicitis. Annals of The Royal College of Surgeons of England 100: 47-51.






























