Community Transitional Nursing Decreases the Incidence of Periprosthetic Joint Infection (PJI)
Liangxiao Bao1, Zhanjun Shi2 and Jianlong Li3,4*
1Deputy Chief Nurse, Head Nurse in Department of Orthopedic Surgery, Nanfang Hospital, Southern Medical University, China
2Professor, Chief Physician, Director in Department of Orthopedic Surgery, Nanfang Hospital, Southern Medical University, China
3Physician in Department of Orthopedic Surgery, Nanfang Hospital, Southern Medical University,China
4Research Scholar in the Department of Pediatrics, Weill Cornell Medicine, United Sates
Submission:April 04, 2021; Published: April 19, 2021
*Corresponding author:Jianlong Li. M.D., M.D., Physician in Department of Orthopedic Surgery, Nanfang Hospital, Southern Medical University, Guangzhou 510515, China, and Research Scholar in the Department of Pediatrics, Weill Cornell Medicine, New York, NY 10021, United Sates
How to cite this article:Liangxiao B, Zhanjun S, Jianlong L. Community Transitional Nursing Decreases the Incidence of Periprosthetic Joint Infection (PJI). Open Access J Surg. 2021; 12(5): 555850. DOI: 10.19080/OAJS.2021.12.555850.
Abstract
Objective: To explore the clinical effects of transitional nursing intervention from hospitalization to community in reducing the risk of infection after total knee arthroplasty (TKA).
Methods It is planned to enroll patients who came to our hospital for total knee arthroplasty from January 2017 to January 2020. They will be randomly divided into two groups, receiving routine care (control group) and special community transitional nursing (experimental group). Analyze the satisfaction rate of the two groups of patients, the healing of the incision 2 weeks after surgery, blood cell analysis, inflammatory indicators (C-reactive protein, CRP. Procalcitonin, ProCT. Erythrocyte sedimentation rate, ESR), serum albumin (ALB), blood glucose level, and the incidence of peripheral prosthesis infection (PJI) in 3 months after surgery to compare the effects of different nursing interventions on the infection risk after TKA.
Results There was no significant difference in general clinical data (age, gender, etc.) between the two groups of patients; The Grade A incision healing rate in the community transitional nursing group (98.1%) was higher than that of the conventional care group (88.5%) (P=0.00066) 2 weeks after surgery. WBC, CRP, and ESR in the community transitional nursing group were lower than those in the conventional care group 1 and 3 months after surgery (P<0.05), while hemoglobin (HGB) and ALB were higher than those in the conventional care group and blood glucose level was more stable (P <0.05). Satisfaction rate was also significantly higher than those in the conventional care group (99% and 90.5%, P<0.05). It was further found that patients with infection in the special community transitional nursing group had longer operation time, long-term uptaking glucocorticoid and poor blood glycemic control (P<0.05).
Conclusion High-quality community transitional nursing intervention can reduce the incidence of PJI after TKA and improve patients’ satisfaction rate.
Keywords:Community transitional nursing; Total knee arthroplasty; Periprosthetic joint infection; Patients’ satisfaction rate.
Introduction
With economic development, people’s living standards have greatly improved, and aging has become more and more common. The incidence of pain and dysfunction, which particularly affects life, is increasing in joint diseases. In order to improve joint function, relieve pain, and improve the quality of life, end-stage knee joint diseases can only be solved by artificial joint replacement [1]. Artificial joint replacement is an orthopedic surgery that uses engineering methods to design artificial joints to replace human joints through surgical replacement, so as to solve the patients’ pain and restore the patients’ physical strength [2]. As an increasingly widely used technology, joint replacement surgery has become an important treatment for various joint diseases, and the number of replacements continues to increase. The popularity of artificial joint replacement is undoubtedly a boon for the majority of patients. Nearly 4 million patients in the United States receive joint replacement every year, and it continues to grow [3].
However, due to the large wound, the long operation time, and the implantation of larger prosthesis, the blood supply of the injured part was poor. In addition, the patients and their families failed to grasp the good wounds during the transition from hospitalization to the community. Nursing techniques are particularly prone to bacterial infections, including skin infections and infections around the prosthesis. Infection is the most serious and common complication of artificial joint replacement, especially the incision grade B healing, grade C healing and periprosthetic joint infection (PJI). The reported incidence of PJI is about 1.41% [4]. PJI treatment is complicated, the treatment period is long, and the disability rate is high. It brings huge health and economic burdens to patients and society, and the consequences are even catastrophic. How to prevent infection, detect infection, and treat infection has always been one of the hotspots and difficulties in orthopedics research [5].
However, there are few reports on the nursing intervention of patients after joint replacement in the process of transition from hospital to community. Although patients and their family members have been guided by medical staff during their hospitalization, for which they have mastered some nursing knowledge and rehabilitation skills, continuous and effective community nursing supervision and guidance are still missing. Community transitional nursing work has always been vulnerable in postoperative care for orthopedic patients in our country, which otherwise causes many infections after joint replacement. Therefore, a series of detailed nursing guidance work such as sterile dressing change, dietary guidance, and rehabilitation exercise assistance in community transitional nursing is particularly urgent and necessary. According to the prospective design, this study compared the impact of different nursing interventions on PJI and found that effective community transitional nursing intervention can reduce the risk of postoperative infection.
Materials and Patients
Material source
It is planned to randomize suitable patients who underwent knee replacement surgery at the Department of Orthopedic Surgery, Nanfang Hospital of Southern Medical University from January 2017 to January 2020. A total of 400 suitable cases will be included as of the time of the study. Inclusion criteria: clinically diagnosed as knee osteoarthritis, rheumatoid arthritis stationary phase, traumatic arthritis, single unilateral or bilateral total knee arthroplasties, no other organ infections during the perioperative period, great compliance of patients and their families. Exclusion criteria: malignant tumors around the joints, septic arthritis, hemophilic arthritis or other infectious arthritis, combined with infections of other organs, incompliance of patients and their families, and less than 2 years of the expected survival period especially those aged. Among them, the conventional family care group is identified as the control group, with a total of 200 cases; the community transitional nursing intervention group is the experimental group, with a total of 200 cases. All patients received informed consents and signed the consent forms. The clinical trial was registered and approved by the Ethics Committee of Nanfang Hospital.
Experimental methods
Prospective analysis of whether patients undergoing TKA will eventually affect the healing of incisions after different cares, patients and their families’ satisfaction rate during diagnosis and treatment periods, and reexamination of inflammatory indicators (including white blood cell, WBC. C-reaction protein, CRP. Procalcitonin, ProCT, Erythrocyte sedimentation rate, ESR, etc.), hemoglobin (HGB), platelet (PLT), blood glucose level (Glu), blood albumin (ALB) in 1 and 3 months after surgery, and the incidence of PJI in 3 months after surgery. The diagnostic criteria of PJI are based on an article published by Bryan D. Springer in The Journal of Arthroplasty in 2015 as a reference standard [6].
Nursing intervention
The administrative nurses of the inpatient department are in patience, comprehensive in knowledge and enthusiastic when making appointments for patients and their family members. They show hospitality when patients are admitted, and carefully explain the precautions for admission. They have a calm tone and avoid using harmful words, always attempt to relieve the tension and as well as fear of the patients and their families. Timely comfort patients, encourage patients, enhance their understanding of the disease and surgery, and enhance their confidence in overcoming the disease. However, in conventional nursing appointment, patients would only be noted with the anticipated admission date and place, as well as some other necessary information that need to be noted during the admission procedure. Nurses would not take other comforting measures including behaviors and body languages to soothe patients.
Preoperative education
Preoperative care: Instruct patients to clean the whole body and special disinfection of the operation area. Soak the feet with disinfectant and clean the lower limbs. Distribute post-operative daily necessities, guide post-operative rehabilitation exercise methods and bed urination and defecation methods. No skin preparation in the surgical area.
Postoperative care: The conventional nursing care group will only check vital signs according to general care, distribute rehabilitation exercise instruction books and videos, and allow patients to leave the hospital and go home 3 days after surgery. However, the details of community transitional nursing intervention are as follows.
Community transitional nursing intervention
Postoperative care: The ward environment is clean, and the bedding is updated as soon as possible. After the operation, the patient was returned to the ward, and the nursing staff used the bed board to transfer the patient from the flatbed to the sickbed. In the supine position, the head is tilted to one side, the lower limbs are placed straightly, monitor the vital signs. Timing turns them over and pat the back, and lower limbs receive air pressure treatment regularly. Check whether the drainage tube is unobstructed, the amount of drainage and the nature of the drainage fluid, so the signs of bleeding can be found in time. The drainage tube should be removed within 24-48 hours after surgery. Strengthen the incision care, strictly adopt aseptic operations, and observe whether the incision dressing is clean or not and whether there is leakage. Both lower limbs were placed with a 30° elevation, and the surgical incision external dressing was given ice physiotherapy within 48 hours after surgery to prevent invisible blood loss in the joints. As the lower limbs are not sensitive to pain and temperature after subarachnoid anesthesia, it is appropriate to strengthen the warmth of the lower limbs, especially the feet, to prevent freezing. The next day after surgery, patients can be instructed to exercise lower limb function, step by step, to prevent deep vein thrombosis. If the catheter is indwelled, perineal care is performed every 8 hours. At the same time, the patient is instructed to drink plenty of water without holding back the urine. Observe the urine volume and color to control the fluid intake from infusion and food, making sure the catheter is removed no later than 24 hours after surgery and recovering from anesthesia.
Doctor-patient communication:Strengthen communication, and promptly report back to physicians when they find that individual patients have questions about surgery or medical care, and jointly answer patients’ questions, concerns and dissatisfaction, and make solutions accordingly.
Rehabilitation guidance: Explain in detail the postoperative precautions, especially the nursing knowledge to prevent infection around the prosthesis, and in the meanwhile teach the patients to improve limb functioning. When the surgical site has pain and/or persistent unrelieved redness of the skin, or inflammation in other parts of the body such as periodontitis, carbuncle, pneumonia and other inflammatory symptoms, patients should promptly report to the relevant medical surgeons and nurses to prevent the spread of infection.
Community Guidance: Nursing staff will be deployed in the same city to visit regularly, and the incision dressing will be changed to observe whether the incision is exuded. If there is any leakage, change the dressing immediately, if not, change the dressing every 2 days. The dressing refreshment processing is strictly aseptic. Doctors or nurses are required to wear a hat, mask and sterile gloves. In addition, instruct functional exercises, such as raising the lower extremity by 30° in the lying position, alternately change to the other lower extremity after fatigue. At the same time, tighten the tibialis anterior muscle, quadriceps femoris and iliopsoas. Plantar flexion exercises the back muscles of the calf. Strengthen the extension and flexion of the hip and knee to prevent stiffness. Guidance on diet and life, each meal contains eggs, lean meat such as beef, fish and milk in order to have enough nutritional intake. Supervise the rehabilitation work of patients. Patients from different cities will be given rehabilitation exercise guidance programs including books, pictures and videos, and they will revive one-to-one guidance via video call. Ensure patient’s recovery process can be followed up seamlessly.
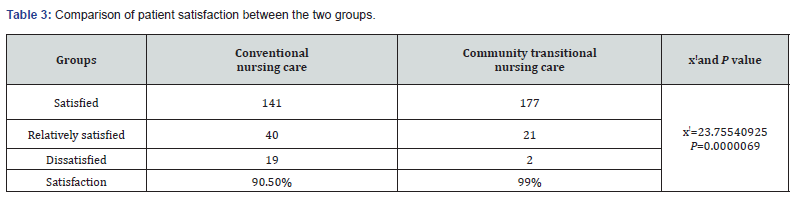
Patients’ satisfaction rate
Compare the two groups of patients’ satisfaction rate with medical care. Use our hospital’s self-made patient satisfaction questionnaire to allow patients to self-test, with a full score of 100. There are three levels of satisfaction rate: satisfied (above 90 points), relatively satisfied (75-89), and dissatisfied (<75 points). The calculation formula for satisfaction rate is: (satisfied + relatively satisfied)/total number of cases × 100%.
Time of suture removal
From the day of surgery to the day of suture removal, the time for suture removal is calculated. Generally speaking, it takes 2 weeks for those normal limbs. The knee joint can be extended appropriately according to the healing situation due to more flexion and extension activities.
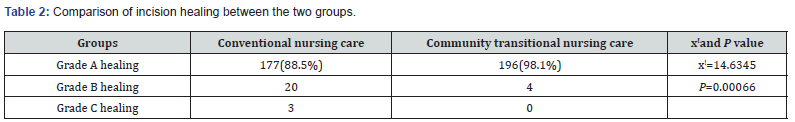
Incision healing
According to the 9th edition of the book “Surgery” (editors: Xiaoping Chen, Jianping Wang, and Jizong Zhao), incision healing is divided into three levels: Grade A: excellent healing, that is, primary healing without adverse reactions; Grade B: poor healing, that is poor healing but not purulent; Grade C: the incision is purulent and requires incision and drainage.
Statistical methods
All data is calculated with SPSS22.0 software, and GraphPad Prism 8 software is used for drawing. If it is a categorical variable, use Spearman’s correlation analysis. If it is a continuous variable, use Pearson analysis to test the influence of the same influencing factor on the factor. One-way ANOVA is used to test the influence of multiple influencing factors on the factor. Multivariate analysis of variance is used, and t Test is used between the two groups. The measurement is expressed as 𝑋 ± s, using x^2 test or Fisher’s exact test. P<0.05 is considered as statistically different. P<0.01 is considered as a significant statistical difference, and P<0.001 is considered as an extremely significant statistical difference.
Results
Comparison of general clinical data between the two groups
The two groups of patients had no difference in the patients’ age, gender, and disease types: osteoarthritis, rheumatoid arthritis, traumatic arthritis, combined underlying diseases, operation time, drainage time, catheter indwelling time, or uptaking glucocorticoid (Table 1). Therefore, it was feasible to compare the risk of postoperative infection with different nursing interventions.

In the community transitional nursing intervention group, the incision healing was better
There were 197 cases in the community transitional nursing intervention group reaching grade A healing, so, the grade A healing rate (98.1%) was higher than that of the conventional nursing control group (88.5%). In the community transitional nursing intervention group, only 4 cases had grade B healing, while 20 cases in the conventional care control group had grade B healing. What’s more, 3 cases in the conventional care group had grade C healing, which was 0 in community transitional nursing group (Table 2, P<0.05).
Comparison of patients’ satisfaction rate
Patient’s satisfaction rate in the community transitional nursing intervention group was 99%, while patients’ satisfaction rate in the conventional nursing group was 90.5%. The patients’ satisfaction rate in the community transitional nursing group was significantly higher than that in the conventional nursing group (Table 3, P <0.05).
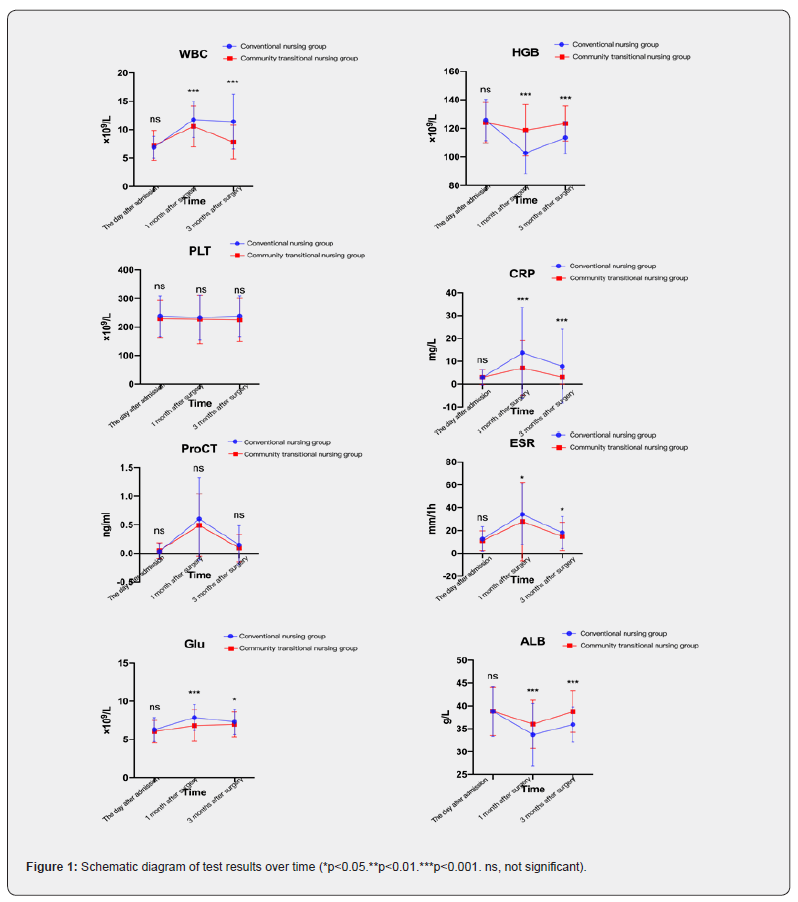
Comparison of blood test results of patients 1 month and 3 months after surgery
A blood test was taken in the morning after admission to the hospital as the baseline value. The patients were asked to return to the hospital for blood test within 1 month and 3 months after the surgery. The review items included blood cell analysis, CRP, ProCT, ESR, ALB and Glu. The results showed that the WBC, CRP, and ESR levels of the patients in the community transitional nursing intervention group were lower than those in the conventional group, and a better concentration of blood glucose was kept. While the HGB and ALB levels were higher (Figure 1), suggesting the effectiveness of dietary guidance and strengthened supervision.
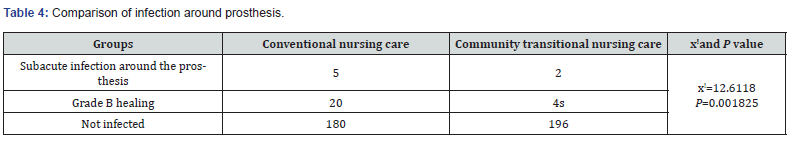
Comparison of infection around prosthesis in 3 months after operation
In the community transitional nursing intervention group, 2 cases of subacute periprosthetic infection occurred. The joint cavity could draw dark red to yellow liquid, with the feeling of subcutaneous pressure fluctuation. The dark red skin was painful, but no liquid under subcutaneous suction, which was considered as subcutaneous fat and necrotic tissue accumulation. The patient also developed transient fever, and gradually improved after the administration of broad-spectrum antibiotics. There were 5 cases of subacute periprosthetic infection in the conventional care group, of which 3 cases improved after antibiotic treatment, while the other 2 patients had recurrent fever and knee joint pain which did not relieve. They were given incision and drainage, a large amount of hydrogen peroxide, chlorhexidine and normal saline irrigation and soaking, indwell one irrigation tube and one drainage tube, separately. The difference between the two groups was statistically significant (Table 4, P<0.05).
Analysis of the causes of Grade B healing and infection around the prosthesis
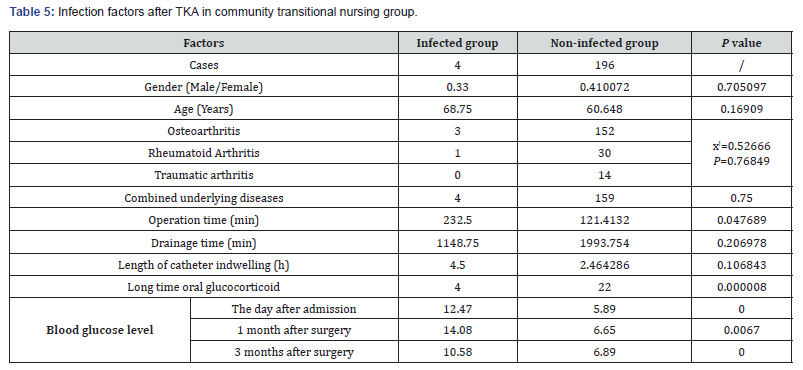
After strict community transitional nursing intervention, there were still patients with grade B healing or infection around the prosthesis. In order to explore the related factors, the patients with grade B healing and subacute PJI in the community transitional nursing intervention group were classified as the infected group, and the others as the non-infected group. After analysis, the susceptibility factors of patients with this type of infection included prolonged use of glucocorticoid, poor control blood glucose, and long operation time (Table 5, P<0.05).
Discussion
The knee joint is the most complex and largest joint in the human body, and osteoarthritis is the main cause of knee pain in middle-aged and elderly patients [7]. Pain is known as the fifth vital sign [8]. The extremely high disability rate caused by knee joint destruction is more common in long-term physical labor, obesity, and other secondary diseases. Knee arthroplasty is an extremely effective treatment method for solving end stage knee joint diseases. It is considered as one of the major inventions of the 21st century, which can alleviate patients’ pain, improve functioning and quality of life [9]. However, infection after knee arthroplasty is the biggest complication of this operation, which is catastrophic [10,11]. Each step error of the medical care and the patient himself may lead to PJI. Once PJI appears, it will bring huge physical, psychological pain and economic burden to the patient. Therefore, how to reduce the incidence of PJI has become one of the most difficult research points in orthopedic medical care.
Our study uses different nursing interventions for patients undergoing total knee arthroplasty to explore which factors in the nursing process will affect post-knee arthroplasty infections. The results found that the patients’ incisions healed better under the community’s high-quality transitional nursing intervention, the grade A healing rate was significantly higher than that of the conventional nursing intervention group, and the patients with peripheral prosthesis infection and grade B healing were significantly lower than the conventional nursing group. As we all know, the joint replacement incision is relatively large. Once the incision becomes infected and fails to receive timely and effective anti-infective treatment, the probability of continuing to develop into infection around the prosthesis is greatly increased. Therefore, better incision healing from community transitional nursing intervention helps reduce the risk of postoperative incision infection and reduces the infection rate around the prosthesis after artificial joint replacement. The satisfaction rate of patients and their families under the intervention of high-quality community transitional nursing has increased significantly, which helps to improve the doctor-patient relationship. Patients and their families are willing to report their discomforts and give their feedback about the physical reactions after medical treatments at any time. Medical staff can timely adjust the treatment plan and clinical practice work. Patients and their families are willing to actively cooperate with medical staff to fight against the common enemy: knee joint disease and other combined underlying diseases. And they will not break the doctor’s instructions or eat unapproved foods and drugs. It is helpful for reducing the risk of infection after TKA.
Blood tests were taken 1 month and 3 months after surgery. The results showed that the levels of inflammatory indicators (including WBC, CRP, and ESR) in the community transitional nursing intervention group were lower than those in the conventional group, suggesting that the body’s stress mechanism against infection faded faster than the normal care group, which means they would return to normal levels faster than conventional group. It is reported that IL-6 can also be used as a new inflammatory index [12], which will be carried out in followup studies to further improve accuracy of our research. Compared with non-diabetic patients, patients with hyperglycemia or diabetes have lower limb function scores after surgery [13], and poor blood sugar control has become one of the risk factors for infection after TKA [14,15]. After the community transitional nursing intervention, the patient’s overall blood glucose control is better, which is obviously conducive to excellent wound healing and further reduces the risk of infection around the prosthesis. In addition, a sharp decline in HGB and ALB occurred due to losing during surgery and poor appetite during the perioperative period. The concentration of HGB and ALB may indicate the risk of infection after joint replacement [16]. Based on dietary adjustment program from community transitional nursing and patients’ positive cooperation, HGB and ALB levels has been significantly improved, prompting the effectiveness of dietary guidance and strengthening supervision, which can enhance the body’s immunity and anti-infection ability. The community transitional intervention group expects zero infection and 100% satisfied. However, cases with infection still happen. The analysis found that this sort of patients has a long operation time, nonideal control of blood sugar, and long-term oral glucocorticoid, which are similar to the results of previous studies [16]. However, it was found that there was no statistical difference if enroll the combined basic diseases. The reasons were considered to be the failure to classify and compare various basic diseases or the sample number was too small. In order to reduce the risk of infection after joint replacement, the above-mentioned risk factors can be deeply improved, and the nursing work should be done well. At the same time, it also requires the surgeon to have mature skills and plan well before the operation to shorten the anesthesia and operation time. In addition, persistently high blood sugar levels will reduce immunity, cause immune disorders, and increase the risk of infection. It is necessary to consult with an endocrinologist to take care of the patient’s blood sugar level, making sure it’s in the best state before performing surgery, and continue to closely track and adjust blood sugar levels after surgery. For patients who take glucocorticoid for a long time, blood sugar is difficult to control, because glucocorticoid suppresses the body’s immunity. Further, metabolic disorders occur, and the risk of incision infection increase. After consultation with the relevant clinical professionals, the glucocorticoid should be reduced as much as possible till it’s being worn off before the operation is performed. Serum albumin level can be used as a nutritional indicator to observe the nutritional status of patients. When its concentration reduces, it will reduce the blood’s ability to carry nutrients and metabolites and will also lead to a decrease in plasma osmotic pressure and incision leakage, which is not conducive to incision healing and increases risk of infection.
In summary, by taking high-quality community transitional nursing interventions for patients undergoing TKA, the risk of infection can be reduced. However, a comprehensive cooperation of surgeons and nurses is needed to intervene and effectively control the risk factors of postoperative infection in advance, so as to control the infection rate after joint replacement to a minimum and eventually eliminate it.
Acknowledgement:
This work was supported by 1. Promotion of appropriate technologies for health and family planning in 2018, Guangdong Health Office Letter [2018] No. 532, 2. National Natural Science Foundation of China (81902730), 3. Guangdong Medical Science and Technology Research Fund Project (A2019213), 4. President’s Foundation of Nanfang Hospital, Southern Medical University (2017B030).
Conflict of Interest
No conflict of interest is declared by the authors.
References
- Connelly JW, Vincent PG, Pakdee R, Christian SN, Charles RB, et al., (2020) Which Preoperative Factors are Associated with Not Attaining Acceptable Levels of Pain and Function After TKA? Findings from an International Multicenter Study. Clin Orthop Relat Res 478(5): 1019-1028.
- Xiao-Hong Wang, Da-Yong Song, Xiang Dong, Toru Suguro, Cheng-Kung Cheng, et al. (2019) Motion type and knee articular conformity influenced mid-flexion stability of a single radius knee prosthesis. Knee Surg Sports Traumatol Arthrosc 27(5): 1595-1603.
- Hilal Maradit Kremers, Dirk R Larson, Cynthia S Crowson, Walter K Kremers, Raynard E Washington, et al. (2015) Prevalence of Total Hip and Knee Replacement in the United States. The Journal of bone and joint surgery. American volume 97(17): 1386-1397.
- Huotari K, M Peltola, E Jamsen (2015) The incidence of late prosthetic joint infections: a registry based study of 112,708 primary hip and knee replacements. Acta Orthop 86(3): 321-325.
- Lazaros A Poultsides, Georgios K Triantafyllopoulos, Vasileios I Sakellariou, Stavros G Memtsoudis, Thomas P Sculco (2018) Infection risk assessment in patients undergoing primary total knee arthroplasty. Int Orthop 42(1): 87-94.
- Springer BD (2015) The Diagnosis of Periprosthetic Joint Infection. J Arthroplasty 30(6): 908-911.
- Tecklenburg K, D Dejour, C Hoser, C Fink (2006) Bony and cartilaginous anatomy of the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc 14(3): 235-240.
- Scher C, Lauren Meador, Janet H Van Cleave, M Carrington Reid (2018) Moving Beyond Pain as the Fifth Vital Sign and Patient Satisfaction Scores to Improve Pain Care in the 21st Century. Pain Manag Nurs 19(2): 125-129.
- Abdelaal, Restrepo, PF Sharkey (2020) Global Perspectives on Arthroplasty of Hip and Knee Joints. Orthop Clin North Am 51(2): 169-176.
- Rezapoor M, J Parvizi (2015) Prevention of Periprosthetic Joint Infection. J Arthroplasty 30(6): 902-907.
- Reinhard Windhager, Markus Schreiner, Kevin Staats, Sebastian Apprich (2016) Megaprostheses in the treatment of periprosthetic fractures of the knee joint: indication, technique, results and review of literature. Int Orthop 40(5): 935-943.
- Shaoyun Zhang, Bin Xu, Qiang Huang, Huan Yao, Jinwei Xie, et al. (2017) Early Removal of Drainage Tube after Fast-Track Primary Total Knee Arthroplasty. J Knee Surg 30(6): 571-576.
- Bryon J X Teo, Hwei-Chi Chong, William Yeo, Andrew H C Tan (2018) The Impact of Diabetes on Patient Outcomes After Total Knee Arthroplasty in an Asian Population. J Arthroplasty 33(10): 3186-3189.
- Hilal Maradit Kremers, Laura W Lewallen, Tad M Mabry, Daniel J Berry, Elie F Berbari, et al. (2015) Diabetes mellitus, hyperglycemia, hemoglobin A1C and the risk of prosthetic joint infections in total hip and knee arthroplasty. J Arthroplasty 30(3): 439-443.
- Esa Jämsen, Pasi Nevalainen, Jarkko Kalliovalkama, Teemu Moilanen (2010) Preoperative hyperglycemia predicts infected total knee replacement. Eur J Intern Med 21(3): 196-201.
- Fernando D Nussenbaum, David Rodriguez-Quintana, Sara M Fish, David M Green, Catherine W Cahil (2018) Implementation of Preoperative Screening Criteria Lowers Infection and Complication Rates Following Elective Total Hip Arthroplasty and Total Knee Arthroplasty in a Veteran Population. J Arthroplasty 33(1): 10-13.






























