Mortality After Hepatobiliary and Pancreatic Surgery in Queensland, Australia (2007-2018): An Analysis of 30-Day Mortality Data After Hepatobiliary and Pancreatic Surgery
Tristan Anderson1*, John North2, Professor Praga Pillay1,3
1QE11 Jubilee Hospital, Department of Surgery, Queensland, Australia
2Queensland Audit of Surgical Mortality, Royal Australian College of Surgeons, Australia
3Griffith University, Australia
Submission:March 08, 2021; Published: April 08, 2021
*Corresponding author: Tristan Anderson, MBBS, BE, QE11 Jubilee Hospital, c/o Department of Surgery, Coopers Plains, Queensland, Australia; Princess Alexandra Hospital, 199 Ipswich Road, Woolloongabba, QLD, 4102, Australia
How to cite this article: Tristan A, John N, Professor P P. Mortality After Hepatobiliary and Pancreatic Surgery in Queensland, Australia (2007-2018): An Analysis of 30-Day Mortality Data After Hepatobiliary and Pancreatic Surgery. Open Access J Surg. 2021; 12(5): 555849. DOI:10.19080/OAJS.2021.12.555849.
Abstract
Introduction: Hepatobiliary and Pancreatic surgery (HBPS) carries a significant morbidity and mortality which prompts appropriate pre-operative risk mitigation of patients. With an aging population, who inherently have a higher perioperative risk, it is important to determine which factors predispose HBPS patients to death after their surgeries. We analysed the QASM data between 2007-2018 specific to HBPS, to identify what characteristics led to patient death.
Method: Patients (18 years of age and older) who died while under the care of a surgeon after HBPS were identified via the Queensland Audit of Surgical Mortality (QASM) database, and their characteristics were analysed.
Results: A total of 118 eligible patients were identified for analysis, 103 (87.3%) of these were 50 years of age or older. Most admissions were emergencies (69.5%). Nearly all the patients (89.0%) had comorbidities, and older patients tended to have more comorbidities compared to their younger counterparts. ASA physical status was three or higher for most patients (83.5%) who died after HBPS. Gallbladder and/or biliary tract operations were far more numerous than others (78.8%). Nearly two thirds of patients had complications (61.9%).
Conclusion: Older age, in association with multiple medical comorbidities are overwhelming responsible for mortality post HBPS. When these patients present acutely with cholecystitis, only limited medical optimisation is possible which compounds their risks of perioperative mortality.
Keywords: Hepatobiliary and Pancreatic Surgery; Mortality; Audit; Risk.
Introduction
Hepatobiliary and Pancreatic surgery (HBPS) carries a significant morbidity and mortality due to the complex nature of the surgery and the patients’ pre-existing co-morbidities. For that reason, it is important to appropriately risk stratify patients who are referred for surgery. This enables better management of high-cost resources and leads to an overall improvement in healthcare [1,2]. Patients with comorbidities are at a higher risk of a complicated post-operative course especially if they are elderly [3-5]. Over the last 20 years in Australia, the elderly population (≥65 y.o.) has increased from 12.2% to 15.7% and is expected
to increase more rapidly over the coming years [6], so more preparation is required for the increase in HBPS.
The aim of this study was to analyse the mortality data after HBPS in Queensland over an 11-year period from 2007 to 2018, with a view to determining what patient characteristics contributed to the deaths. The Queensland Audit of Surgical Mortality (QASM) records all surgical mortalities within Queensland hospitals, both public and private. It is compulsory for administrators to report such deaths to QASM, irrespective of the cause of death [7]. Data is conveyed to QASM by the treating surgeon via a generic surgical case form (Appendix 1). A peer review of the case reported is then
undertaken and a confidential feedback is given to the surgeon –
mainly for educational purposes.
Method
Data was retrospectively collected from the QASM database, over 11 years (2007-2018). A list of HBP surgical procedures undertaken (Appendix 2). A total of 184 deceased patients were identified. Surgical Trauma with no hepato-biliary injuries were excluded (66 cases) allowing 118 cases for analysis.
Results
Of the 118 cases who died there were 72 (61.0%) males and 46 (39.0%) females. The average age was 68.3 (range 19-94 years). For those aged ≥50 years, there were 103 cases (87.3%) with 64 males and 39 females. There were 15 cases below 50 years: 8 males, 7 females (Table 1).
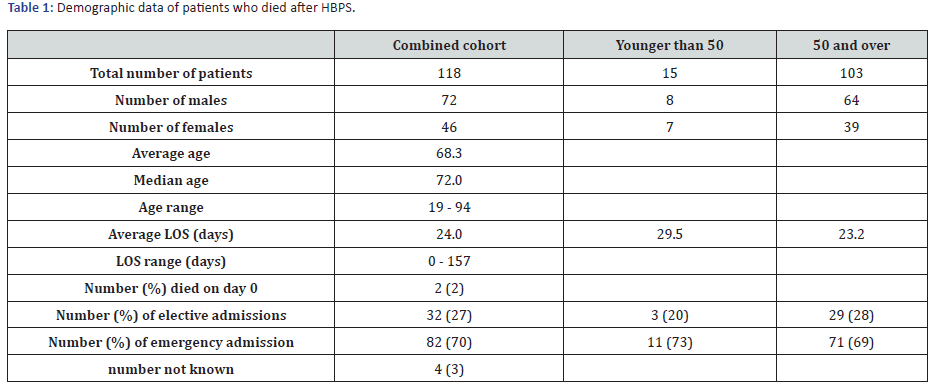
LOS, Length of stay (days)
Emergency admissions were the commonest at 82 (69.5%), elective admissions were less common with 32 cases (27.2%); the admission data in 4 cases was not recorded. The average length of stay (LOS) was 24.0 days. For patients over 50 years average LOS was 23.2 (including 2 deaths on day 0). For patients under 50 years average LOS was considerably longer at 29.5 days. Comorbidities were present in 105 cases (89.0%) and included cardiovascular 61.9%, respiratory 40.9%, and renal disease 38.1%. The ASA (American society of Anaesthesiologists [8]) physical scoring system being ≥3 in 83.5% of patients. Seventeen cases were ASA 5 and not expected to survive (Table 2).
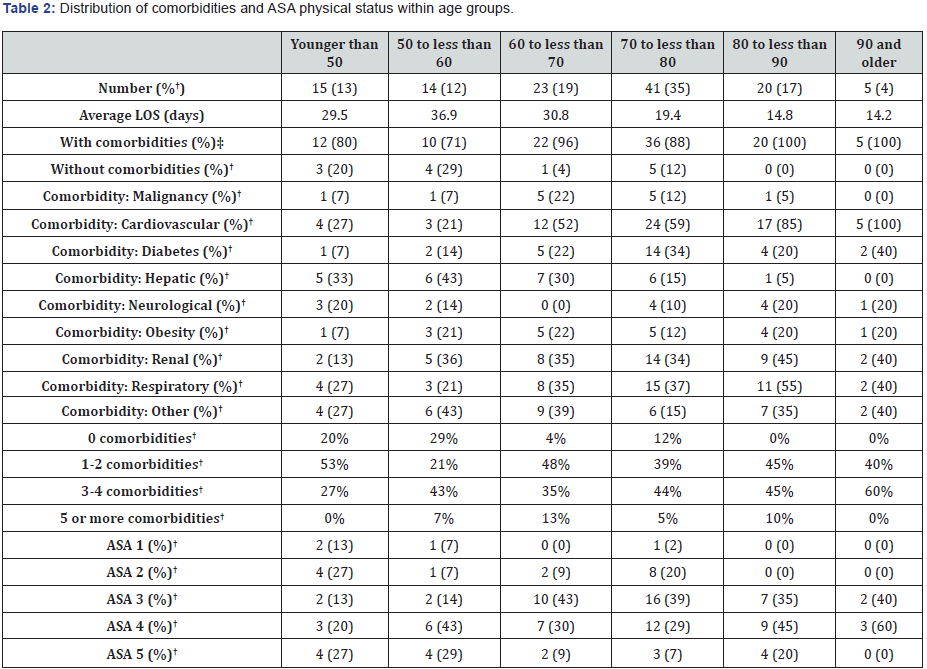
†percentage of cohort; †percentage of age group
The surgical procedures were classified into three groups for
analysis (Table 3):
i. Gallbladder and/or Bile ducts – 93 patients (78.8%)
ii. Liver – 24 patients (20.3%)
iii. Pancreas – 10 patients (8.5%)
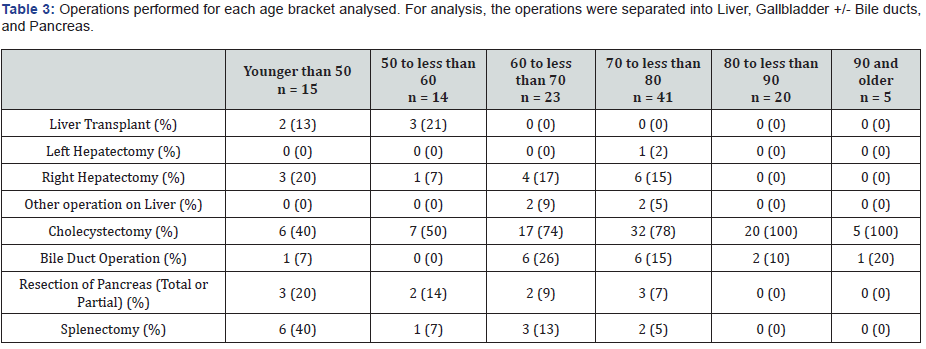
Those aged 50 years and over had mostly gallbladder/and
or bile duct surgery 86/103 (83.5%) while those under 50 years
7/15 (46.7%) had biliary surgical procedures. Postoperative
complications were high 73/118 (61.9%); of these 40 (33.9%)
had an unplanned admission to the Intensive Care Unit (ICU) and
38 (32.2%) needed a return to the operating theatre for postoperative
problems. In 12.7% of cases no complications were
recorded even though the patients had unplanned admission to
ICU or reoperations. An important tool in the audit assessment
is that of the surgeon’s opinion of the risk of death in each case
(Table 4).
Ninety-eight per cent of surgeons responded as follows:
i. 70/118 (60.3%) were at high risk of death. Of these
high-risk patients, 13/15 (86.7%) were under 50 years and
58/101 (57.4%) were ≥50 years.
ii. Thirty-one (26.7%) patients were at moderate risk.
iii. Fifteen (12.7%) patients were at low risk.

Discussion
Our analysis indicated that age was a significant factor in
determining mortality after HBPS, with 87% of deaths occurring
in patients 50 years and over, and particularly between the ages
70 to 79 years. This can be related to the very high ASA scores
and comorbidities in this group of patients. Some studies have indicated that age alone is not an absolute determinant of
outcome after HBPS [2,9-12]. Notably, the common theme within
these studies is rigorous patient selection based on preoperative
assessment, and the subsequent exclusion of patients with
significant comorbidities or high ASA scores. In contrast, our
data includes both elective and emergency cases which involved
several patients with an ASA score of four or more. In addition,
preoperative optimisation was limited for many of these patients.
In our study, the number of co-morbidities per patient
increased with age, with those over 70 years having three or
more comorbidities. Patients with comorbidities have a higher
rate of post-operative morbidity and mortality [3,13] with one
study identifying a four-fold increase in mortality in the presence
of three or more comorbidities [4]. Additionally, in our study the
number of patients with cardiac and respiratory disease increased
with age; similar studies with comorbidities confirmed a higher
mortality [3-5,13]. In our study some 83% of patients older than
60 years had gallbladder and/or bile duct surgery. 25 of these
patients were older than 80 years with all of these very elderly
patients dying due to established sepsis and multiorgan failure.
Nikfarjam [14] showed that patients over 80 years are more likely
to have gangrenous cholecystitis and this was found in our study
as well. The surgeons risk assessment in this study indicated that
many cases were at high risk.
When compared, our cohort of specific HBPS mortality to the
Queensland and Australian general surgical mortality data from
similar periods, notable differences were seen. The median age was
younger in our cohort, consisted of more elective admissions, had
fewer patients with high ASA scores, and had fewer comorbidities.
The post-operative complication rate in our cohort of patients was
almost double both the QASM [15] and ANZASM [16] findings:
61.9% in comparison to 33.3% and 33.9% respectively. Our cohort
consisted of younger and healthier patients, but the significantly
high post-operative complication rate directly contributed to
patient deaths. Post-operative complications have been shown to
be a “strong predictor of death” [15].
Conclusion
We have analysed the mortality data after HBPS and identified common characteristics. Of the patients who died, increasing age in association with several comorbidities and emergency surgery were common. When compared to the state and national data, the HBPS cohort analysed from QASM were younger and healthier but their post-operative course was considerably more complicated. Evidence shows that patient optimisation prior to surgery is ideal, but our analysis suggests that this may not always be applicable potentially leading to an increased rate of complications and postoperative death.
Disclosure Statement
There are no financial interests that relate to the research in this article.
List of Hepatobiliary and Pancreatic Surgeries
Operation
Cholecystectomy
Bile duct or Biliary
Liver resection or Hepatectomy
Shunt surgery for portal hypertension
Pancreatectomy
Necrosectomy (Pancreas)
Splenectomy
Duodenectomy
Choledochoduodenostomy
Choledochojejunostomy
Hepaticojejunostomy
Pancreaticogastrostomy
Pancreaticojejunostomy
Bile Duct
Excision of bile duct
Extirpation of lesion of bile duct
Extirpation of lesion of bile duct
Open operations on prosthesis in bile duct
Repair of bile duct
Incision of bile duct
Plastic repair of sphincter of Oddi using duodenal approach.
Incision of sphincter of Oddi using duodenal approach.
Other operations on ampulla of Vater using duodenal approach.
Other open operations on bile duct
Therapeutic percutaneous attention to bile duct connection
Therapeutic percutaneous insertion prosthesis into bile duct
Other therapeutic percutaneous operations on bile duct
Therapeutic operations on bile duct along T tube track
Percutaneous examination of bile duct
Other operations on bile duct
Pancreas
Transplantation of pancreas
Total excision of pancreas
Excision of head of pancreas
Other partial excision of pancreas
Extirpation of lesion of pancreas
Connection of pancreatic duct
Other open operations on pancreatic duct
Open drainage of lesion of pancreas
Incision of pancreas
Open examination of pancreas
Other open operations on pancreas
Therapeutic percutaneous operations on pancreas
Diagnostic percutaneous operations on pancreas
Liver
Transplantation of liver
Partial excision of liver
Extirpation of lesion of liver
Repair of liver
Incision of liver
Other open operations on liver
Therapeutic endoscopic operations on liver using laparoscope
Diagnostic endoscopic examination of liver using laparoscope
Transluminal operations on blood vessel of liver
Other therapeutic percutaneous operations on liver
Diagnostic percutaneous operations on liver
Other puncture of liver
Other operations on liver
Spleen
Total excision of spleen
Other excision of spleen
Other operation on spleen
Duodenum
Connection of stomach to duodenum NEC
Excision of duodenum
Open extirpation of lesion of duodenum
Bypass of duodenum
Other open operations on duodenum
Other operations on duodenum
Operations on duodenal ulcer
References
- Mann CD, Palser T, Briggs CD, (2010) A Review of Factors Predicting Perioperative Death and Early Outcome in Hepatopancreaticobiliary Cancer Surgery. HPB 12(6): 380-388.
- Kocher HM, Tekkis PP, Gopal P, Patel AG, Cottam S, et al. (2005) Risk-Adjustment in Hepatobiliarypancreatic Surgery. World Journal of Gastroenterology 11(16): 2450-2455
- Egeli T, Unek T, Agalar C, (2019) Survival Outcomes After Liver Transplantation in Elderly Patients: A Single-Centre Retrospective Analysis. Transplantation Proceedings 51: 1143-1146.
- Shin DK, Kim SH, Moon DB, Shin H, Ki Hum K(2018) Impact of Preoperative Management in Patients Older Than 80 Years Requiring Cholecystectomy. Annals of Hepato-Biliary-Pancreatic Surgery 22: 380-385.
- Prashant S, Jonathan T, Mauricio S, James S, Peter D (2012) Advanced Age is a Risk Factor for Post-Operative Complications and Mortality After a Pancreaticoduodenectomy: A Meta-Analysis and Systematic Review. HPB 14: 649-657.
- Australian Bureau of Statistics (2019) Twenty years of population change. Australian Bureau of Statistics 2019. Canberra, Australia.
- Royal Australian College of Surgeons. Queensland audit of surgical mortality [Internet]. Melbourne VIC: Royal Australian College of Surgeons.
- American Society of Anaesthesiologists. Standards and Guidelines (2019) American Society of Anaesthesiologist, . Schaumburg, IL, US State.
- Faraj W, Alameddine R, Mukherji D (2013) Postoperative Outcomes Following Pancreaticoduodenectomy: How Should Age Affect Clinical Practice? World Journal of Surgical Oncology 11: 131.
- Kim J H, Min S K, Lee H, Hong G, Lee H K (2016) The Safety and Risk Factors of Major Hepatobiliary Pancreatic Surgery in Patients older than 80 years. ASTR 91(6): 288-229.
- Lu Q, Lu JW, Wu Z, Xue Min Lu, Jian Hu Liu, et al. (2018) Perioperative Outcome of Elderly Versus Younger Patients Undergoing Major Hepatic or Pancreatic Surgery Clin Interv Aging 13: 133-141.
- Wickremesekera SK, Seo H B, Trimber MA, Bann S, Tse K (2016) A Morbidity/Mortality Analysis of a Tertiary Level Upper Gastrointestinal/Hepatopancreaticobiliary Surgical Unit. NZMJ 129: 81-91.
- Bentrem DJ, Cohen ME, Hynes DM, Ko CY, Bilimoria KY (2009) Identification of Specific Quality Improvement Opportunities for the Elderly Undergoing Gastrointestinal Surgery. Archives of Surgery 144(11): 1013-1020.
- Nikfarjam M, Yeo D, Perini M (2013) Outcomes of Cholecystectomy for Treatment of Acute Cholecystitis in Octogenarians. ANZ Journal of Surgery 84: 943-948.
- Queensland Audit of Surgical Mortality ( Queensland Audit of Surgical Mortality (QASM) Report 2007-2016. Australasian College of Surgeons. QASM: East Brisbane, Australia.
- Australian and New Zealand Audit for Surgical Mortality (2016) Australian and New Zealand Audit for Surgical Mortality National Report 2016. Royal Australasian College of Surgeons. ANZASM, North Adelaide, Australia.






























