A Rare Case of Symptomatic Bochdalek Hernia in 58-years-Old Male
Vladislav Stoyanov* and Veselina Ivanova
Medical Institute – Ministry of Interior, Bulgaria
Submission:January 31, 2021;Published:February 17, 2021
*Corresponding author: Vladislav Stoyanov, M.D., PhD, Medical Institute – Ministry of Interior, Sofia, Bulgaria
How to cite this article: Vladislav S, Veselina I. A Rare Case of Symptomatic Bochdalek Hernia in 58-years-Old Male. Open Access J Surg. 2021; 002 12(4): DOI:10.19080/OAJS.2021.12.555844.
Abstract
Bochdalek hernia in adults is rare. It can be found accidentally or when it is symptomatic. It‘s a congenital defect of posterolateral part of the diaphragm and may contain different abdominal organs like stomach, omentum major, spleen, small or large intestine. The most commonly used diagnostic methods are CT, MRI, barium swallow test of upper GI, gastroduodenoscopy. Open surgery or mini-invasive surgical methods can restore the congenital defect. Depends on the size of the hernia, plastic reconstruction of the diaphragm can be done or using of two-component meshes. After surgery the prognosis is usually favorable.
Keywords: Bochdalek hernia; Diaphragmal hernia; Congenital.
Introduction
Bochdalek hernia is rare. This type of hernia was first described in 1754 by McCauley and subsequently studied and named after the Czech pathologist, Vincenz Alexander Bochdalek (1801–1883) [1]. It is a congenital defect in the posterolateral part of the diaphragm, resulting from a defect in its development. In 85% of cases, these hernias are left-sided [2-8]. The incidence of congenital diaphragmal hernias is approximately 1: 2000 to 1: 3000 [2]. They most often appear in childhood, with respiratory problems. They are more common in men and the male-female ratio is 1.72: 1 [5].
Bochdalek hernia in adults is very rare. About 100-150 cases have been described in the literature [4]. Most often they are asymptomatic, and which are found during computer tomographic (CT) examination done on another occasion. The omentum most often enters the hernial defect, less often the spleen, small intestine or large intestine can be found. In very rare cases, it is symptomatic and can lead to respiratory disorders, herniated organ dysfunction or incarceration. Diagnosis of these hernias involves X-ray examination, which most often shows an organ with a hydro aerial level above the diaphragm. Contrast enhanced CT is most useful for diagnosis. It shows a soft tissue or fat formation on the upper surface of the diaphragm.
Case report
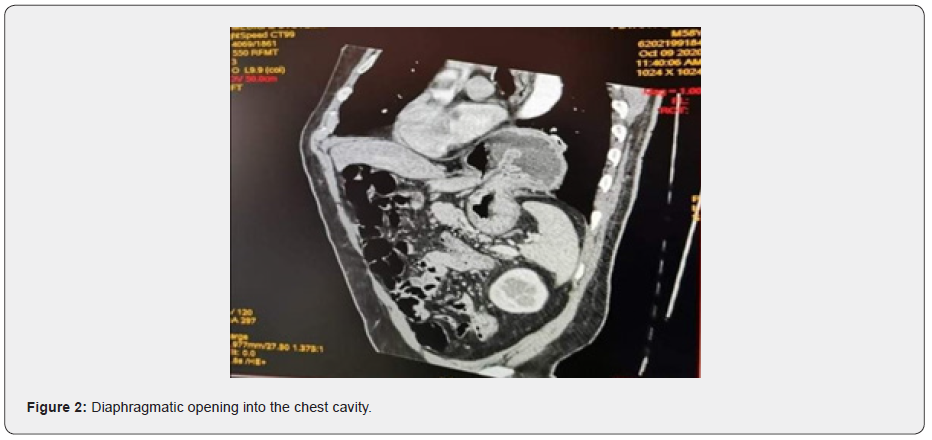
58-year-old male admitted to the surgical clinic with complaints of abdominal pain and bloating, nausea without vomiting, shortness of breath and heaviness in the left chest, appearing after feeding for several months. Upon admission, the patient underwent X-ray examination of the chest that shows a hiatal hernia, as well as imaging test for the upper GI tract - examination of the stomach with barium swallow test - evidence of hiatal hernia (Figure 1). The CT scan revealed a diaphragm defect and data on a changed location of the stomach with the location of the fornix between the spleen and the tail of the pancreas, and the body and most of the antrum pass through the diaphragmatic opening into the chest cavity (Figure 2). The result of gastroduodenoscopy was that ½ of the stomach is herniated into the thoracic cavity. Blood tests show normal value. From the tests performed in this way, it was established that it was a diaphragmatic hernia.
Results
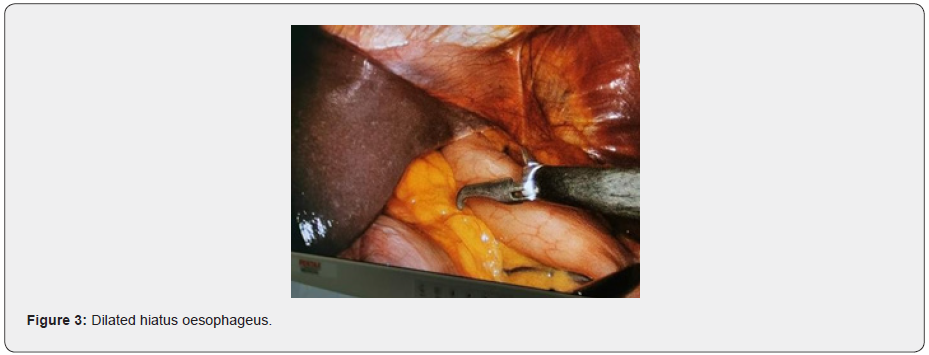
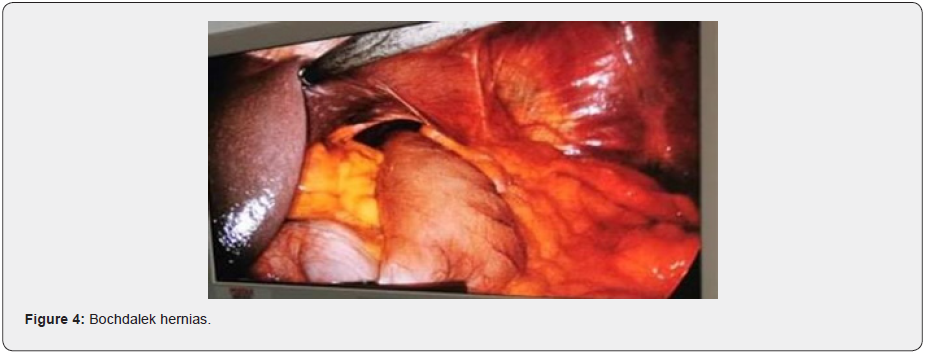
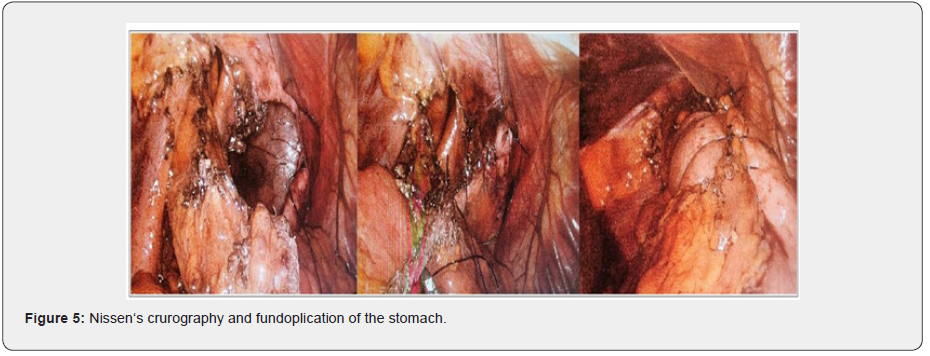
The patient was offered laparoscopic surgery. He underwent nasogastric tube preoperatively. 5 trocars were used, located in typical places. Intraoperatively, a diaphragmatic defect was found to the left of the left crus of diaphragm, about 6 cm in size, with a hernia of 2/3 of the stomach and omentum major and a slightly dilated hiatus oesophageus (Figures 3 and 4). It was considered to be a Bohdalek diaphragmatic hernia and an enlarged hiatus esophageus. We reposited the stomach in the abdominal cavity. The peritoneum was incised along the greater curvature and using LigaSure the left curvature and the fundus of the stomach were mobilized, dividing the short gastric vessels. The hernial sac around the stomach was released and excised. The peritoneum on the right around the lesser curvature was incised, visualizing the right crus of the diaphragm and esophagus. Using a blunt and sharp way passed behind the esophagus and mobilized the gastroesophageal ligament. Then we done a plastic reconstruction of the diaphragm with a continuous stitch. Nissen‘s crurography and fundoplication of the stomach was done (Figure 5). Antibiotic therapy with ceftriaxone and metronidazole was used, as well as prophylaxis with low molecular weight heparin. The postoperative period went smoothly. The patient was upright and actively moved a few hours after surgery, fed on the 2nd postoperative day and discharged on the 4th postoperative day. At follow-up 3 months after surgery, the patient feels well and has no complaints from the gastrointestinal tract and respiratory system.
Discussion
Bochdalek hernia is the result of a disorder in the development of the diaphragm. The diaphragm begins to form during the 4th week of gestation, and its posterolateral part originates from the pleuroperitoneal membrane. During the embryonic period, the connection between the pleural and peritoneal cavities is made through the Bochdalek opening. This communication usually closes around the 8th week of gestation. If this does not happen, a defect remains in place. The right pleuroperitoneal canal closes earlier than the left, as a result of which most Bochdalek hernias are left-sided [2,3]. Diaphragmatic hernias are most often diagnosed before birth, but in rare cases they may not appear until adulthood.
They are most often asymptomatic and are found accidentally when CT is performed on another occasion. In their study, Brown, et al. [4] found that only 14% of patients were symptomatic at the time of diagnosis, with the most common complaints being chest pain or tension, respiratory distress, obstruction, and dysphagia. Diagnosis of Bochdalek hernia is difficult and is more often confused with hiatal hernia. The diagnostic methods used are chest radiography, barium swallow test of upper GI tract, CT and MRI. The most informative method is CT, in which the herniated organs and the location and size of the diaphragmatic defect are visualized [7].
The treatment of these hernias is surgical. It can be performed both by open surgery or mini- invasive techniques. Both abdominal and thoracic access are possible. The defect can be repaired by plastic reconstruction of the diaphragm or by various prosthetic materials. The use of polypropylene mesh allows the correction of the defect without tension, but on the other hand there is a risk of causing erosions in neighboring organs. By using two-component meshes to close the defect, the risk of such a complication can be avoided [6,7].
Conclusion
Bochdalek hernia in adults is very rare. Mini-invasive surgical treatment is best method of choice. The prognosis after surgery is good. Complications are rare. Conflict of Interests: Declare no conflict of interests.
References
- Brown SR, Horton JD, Trivette E, Hofmann LJ, Johnson JM (2011) Bochdalek hernia in the adult: demographics, presentation, and surgical management. Hernia. The Journal of Hernias and Abdominal Wall Surgery 15 (1): 23-30.
- Gue RS, Winkler L, Bochdalek Hernia (2020) In: StatPearls [Internet]. Treasure Island (FL) StatPearls Publishing.
- L Topor, T Pătrăncuş, R Caragaţa, A Moga (2015) Left congenital diaphragmatic hernia – Case report Chir (Bucur) 110(1): 84-87.
- Mark E, Mullins, Jeffrey Stein, Sanjay S, Saini, et al. (2001) Prevalence of Incidental Bochdalek's Hernia in a Large Adult; American Journal of Roentgenology 177(2).
- Shanmugam H, Brunelli L, Botto LD, Krikov S, Feldkamp ML (2017) Epidemiology and Prognosis of Congenital Diaphragmatic Hernia: A Population-Based Cohort Study in Utah. Birth Defects Res 109(18): 1451-1459.
- SR Brown, JD Horton, E Trivette, LJ Hofmann, JM Johnson (2011) Bochdalek hernia in the adult: demographics, presentation, and surgical management. Hernia 15(1): 23-30.
- T Toydemir, H Akinci, M Tekinel, E Süleyman, B Acunaş, et al. (2012) Laparoscopic repair of an incarcerated Bochdalek hernia in an elderly man Clin (Sao Paulo) 67(2): 199-200.
- Yusuf Yagmur, Ebral Yiğit, Mehmet Babur, Serdar Gumuş (2016) Bochdalek hernia: A rare case report of adult age. Annals of Medicine and Surgery 5: 72-75.






























