Highly Polished Scalpel Blades Reduce Incisional Wound Scar Variability in Duroc Pigs
Haitao Chen1, Tamara Vincer2, James A Hicks2, Raphael C Lee1* and Clifford L Spiro2,3
1Avocet Polymer Technologies, United States
2Cabot Microelectronics Corp Aurora, United States
3Current Address: Entrepix Medical LLC Phoenix, United States
Submission:August 17, 2020; Published:October 12, 2020
*Corresponding author:Raphael Lee, MD, Avocet Polymer Technologies, Inc. 4047 W. 40th St. Chicago, Illinois 60632, United States
How to cite this article:Haitao C, Tamara V, James A H, Raphael C L, Clifford L S. Highly Polished Scalpel Blades Reduce Incisional Wound Scar Variability in Duroc Pigs. Open Access J Surg. 2020; 12(2): 555833. DOI: 10.19080/OAJS.2020.12.555833.
Abstract
Concern about scar appearance resulting from surgical incision remains a principal motivator for the investment in minimally invasive surgery. There are some medical circumstances where an open surgical procedure is needed and thus there continues to be a need to reduce post-surgical skin scarring. This project was designed to determine if highly polished surgical scalpel blades would result in reduced tissue damage, subsequent inflammation and scarring compared to clinical standard scalpel blades. A Duroc pig surgical incision model was used to compare scarring resulting from polished standard commercial surgical blades at three levels of enhanced surface finish to commercially available blades. Differences in scar formation (area and width) were compared among the groups at various time points (day 5, day 30 and day 60). At every postoperative time point, the polished blades demonstrated significantly smaller scar area (p < 0.05) than the corresponding control group ( Bard-Parker #15 blades). Also, we observed polished blades had significantly smaller scar width and width variance than tested commercial blades at day 60 (p < 0.05). The explanation for this effect is related to the reduced tissue trauma caused by scalpel blades produced by the fine-finishing process. The data supports the hypothesis that surgical incisions from extremely finished blades result in considerable reduction in scarring.
Keywords:Scalpel Blade; Sharpness; Polish; Scar; Pig; Hypertrophic
Introduction
The need for skin incisions to gain surgical access to the body is very likely to continue for the foreseeable future. The amount of scar that forms depends on both genetic and epigenetic factors. Genetic factors are not controllable today. On the other hand, epigenetic factors can be manipulated. The two most important epigenetic factors are the magnitude of inflammation and the mechanical tension on the healing wound. The magnitude of tissue inflammation correlates to the extent of injury. It is well documented that the extent of scarring and fibrosis is related to extent of injury [1]. Therefore, various surgical instruments and techniques have been introduced to minimize incisional tissue injury during surgical processes [1-6]. Even with new instruments and techniques, cold steel scalpel blades are still the most popular surgical device. It is not known exactly why the new technologies have not been fully embraced, but it raises a question. Can improvements be made to the cold steel scalpel blade to reduce incisional tissue trauma and improve wound healing? The objective of this study is to quantitatively determine if improving the surface topography of the scalpel blades will reduce the injury to the tissue and, in turn, improve wound healing. A surgeon’s intuition would suggest that commercially available scalpel blades are as smooth and sharp as possible. However, when visualized under scanning electron microscopy, clear lateral ridges and saw tooth edges are routinely seen. Such imperfections can create microscopic dragging forces in the extracellular matrix, thereby imparting an unsuspected degree of para-incisional trauma. The hypothesis of the study is that highly polished scalpel blades will cause less tissue damage and therefore will result in less scar formation.
Blades were polished using a variant of chemical mechanical planarization, (CMP), which is a well-established process widely employed in the manufacture of semiconductors that are used for memory storage and data processing [7]. As transistors and interconnects have shrunk to sub-10nm dimensions, computer-chip surfaces have needed to be planarized to near-atomic perfection in order to prevent circuit failures from surface topography and debris. The use of a modified semiconductor CMP process on surgical scalpels was demonstrated to be effective in dramatically reducing scalpel surface and edge topography [8]. To test whether ultra-polished scalpel blades would reduce scarring, we selected an animal model that would allow comparison of different blades in the same animal and in which the degree of scarring could be measured over a substantial period of time. We chose to compare scar sizes using high-resolution imaging while minimizing genetic and some epigenetic variability measurements of para-spinal cranial-caudal oriented wounds in a Duroc pig animal model. Recently, we completed a similar study regarding healing and trauma in Guinea pigs [9] where we observed significant benefits in healing and scarring with the more refined surface of the scalpel. However, it is well established that Duroc pigs best replicate human tissue response to trauma including propensity for hypertrophic scarring [10,11].
The wound healing responses of the highly polished scalpel blades are compared to existing commercially available scalpel blades that manifest from 1-3 orders of magnitude coarser surface topography along with ragged edges that naturally arise from the mechanical grinding processes used in current manufacturing practices. We measured the influence of blade surface finish in terms of overall wound healing and scarring. Time periods of 5, 30 and 60 days were chosen to represent the three phases of the wound healing cycle, i.e., inflammation, proliferation and remodeling, respectively.
Materials and Methods
Scalpel blades
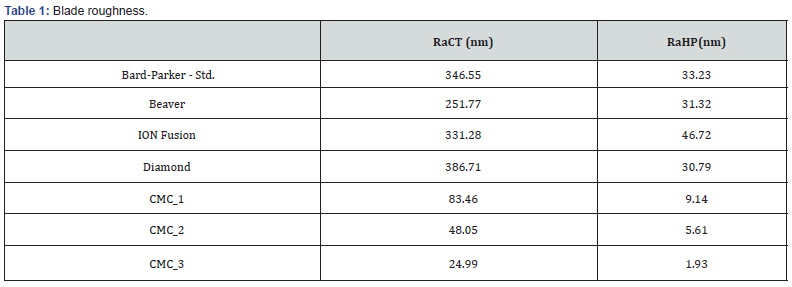
We applied to commercially available #15 stainless steel slot scalpel blades, an advanced surface finishing technology which is a variant on chemical mechanical planarization, CMP. Chemical mechanical planarization has long been used in semiconductor processing, to polish the advanced circuitry on silicon semiconductor wafers. As evident from Table 1 and Figure 1, the surgical scalpels and slot blades in wide use today are replete with texture. In this study, we evaluated four commercial blades: the popular Bard-Parker #15; the Beaver #67 blade; an Ion Fusion blade that has a hard-metallurgical coating that appears to be conformal; a synthetic polycrystalline diamond blade, and three polished versions of the Bard-Parker #15
that have been progressively polished by the proprietary semiconductor-like polishing processes.
This study included seven different scalpel blades: four commercial blades and three experimental blades polished using proprietary surface modification methods. One of the most common blades used in surgical applications is the stainless-steel Bard-Parker #15, for this reason it was used as the control. The other commercial blades were the Beaver, Ion Fusion #15, and diamond. These appear as optical micrographs at 400x, Figure 1, using a Keyence VHX-1000 white-light optical microscope. A new blade was used for each incision except the diamond blade. Two diamond blades were used, sterilized, and reused throughout the experiment to replicate the reusable nature of this type of blade. The following is a list of the blades used in this experiment, and Figure 1 shows a magnified representation of each blade edge.
i. Blade A – standard Bard-Parker #15 from Becton Dickinson (Franklin Lakes, NJ USA)
ii. Blade B – Beaver blades from Becton Dickinson
iii. Blade C – Ion Fusion #15 from Ion Fusion Surgical™ (Lakeside, CA, USA)
iv. Blade D – Diamond blades from Element Six Ltd. (Ascot, Berkshire, UK)
v. Blade CMC_1 (Spiro 2019)
vi. Blade CMC_2 (Spiro 2019)
vii. Blade CMC_3 (Spiro, 2019)
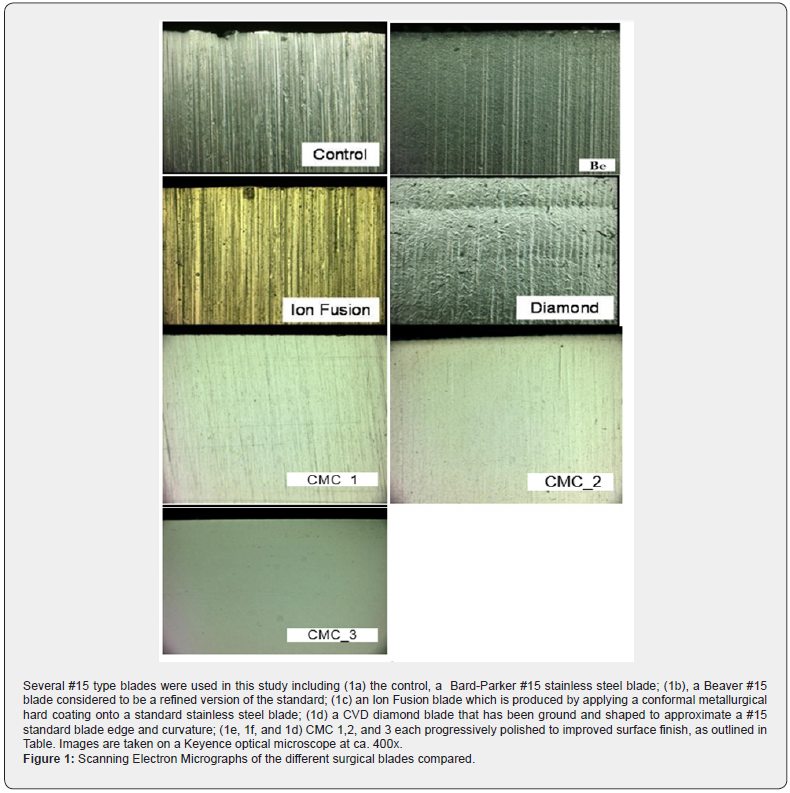
For the purpose of understanding, the reader should consider CMC processes 1, 2 and 3 [12] as successively refined in surface, as can be seen in Table 1. In Table 1, we see two values for blade roughness as measured using a Veeco white- light interferometer. The first column, Ra CT measures surface roughness after curvature and tilt are subtracted, but which captures both local roughness and the macro roughness associated with grind striations in the metal. The Ra HP has additional filtering of the data to remove macro-waviness, and represents a much more localized roughness. Scalpel blades were immediately put into an alcohol bath following incisions. After surgeries were completed, blades were moved from the alcohol bath to de-ionized water for subsequent analysis, none of which were found to reveal significant changes. Once surgeries for the day were completed, diamond blades were cleaned using the methods provided by the manufacturer and sterilized in hospital facilities.
Experimental design and data collection
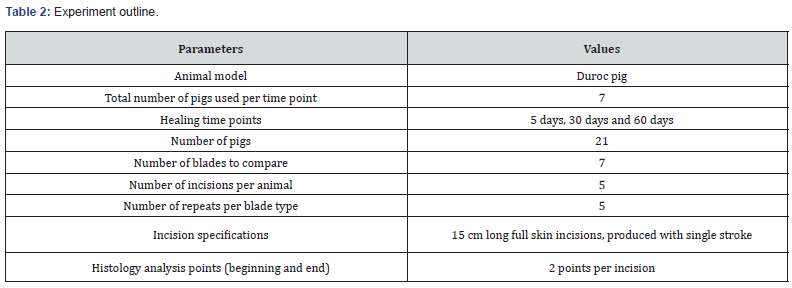
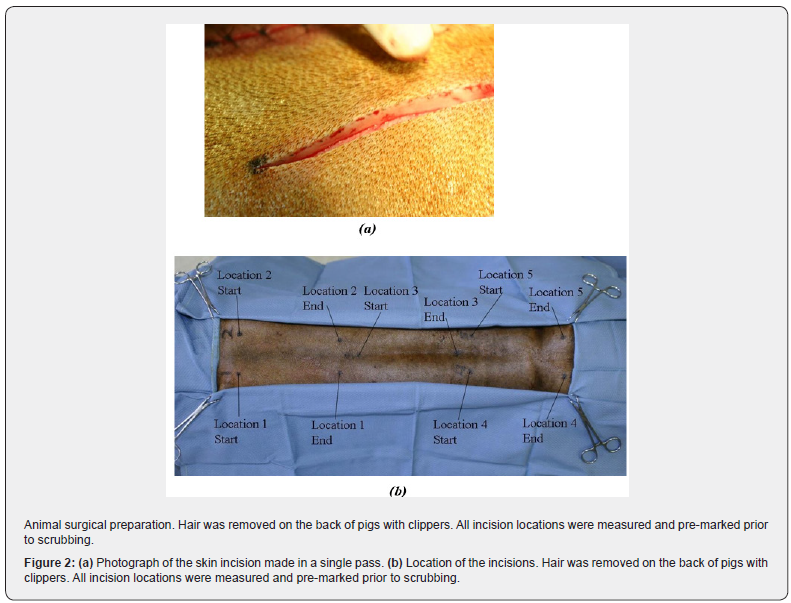
Table 2 shows an overview of the experimental approach used in this study. A total of 21 Duroc pigs were used with five 15cm long incisions per pig (Figure 2) yielding a total of 105 separate incisions and scars, each of which were analyzed in a variety of ways (see below). A total of seven different blades were used to create the 105 scars, yielding 15 data points per blade.
The animal protocol was approved by the Michael Reese Hospital Animal Care and Use Committee, using the guidelines put forth by the National Institutes of Health (NIH) described in The Guide for the Care and Use of Laboratory Animals (NIH Publication no. 86-23, 1985, Department of Health and Human Services). The animals were divided into three groups of seven by the duration over which the wounds were allowed to heal: 5, 30, or 60 days post-operation. All blades were sterilized prior to experimental use. Incision sites were pre-marked and a single veterinary surgeon performed all incisions in an attempt to reduce variability and ensure uniformity in length and depth. Blade types were blinded to the surgeon to reduce bias. The wounds were closed with 2-0 monofilament vinyl sutures spaced 1-1.5 cm apart along the length of the incision by the surgeon. A total of 10 to 11 simple interrupted sutures were placed in each wound immediately after each incision and wound edges were easily approximated.
Parallel paravertebral dorsal skin incisions
Using a large animal model such as a Duroc pig allows multiple incisions to be made with enough separation to prevent interaction. All incisions were made under appropriate general anesthesia by a veterinarian. Because paravertebral incisions were made, it was possible to compare left and right-side responses. The incisions were made through the skin in a single pass with the blade held at a 45-degree angle and a blade cutting guide inserted beneath the skin to protect against injury to fascia and muscles.
Post-operative care and follow-up procedures
The animals were maintained on 100% FI02 ventilator support until awake enough for extubation. The surgical incisions were covered with sterile gauze and elastic surgical net covering wrap and allowed to recover in a clean isolated cage near the operating room. They were moved to pens after 24 hours. All animals were administered a 5-day series of antibiotics and buprenorphine (pain reliever) for 2-3 days post-operation. Sutures were removed at 10 days post-operation. Digital photographs of the wound areas were taken on the day of surgery, the following predefined days and the final day.
Histology staining
Biopsies, approximately 1.5 cm long by 0.5 cm wide with full thickness strips of tissue, were removed on the last day and fixed in formalin and sent to pathology labs for staining. Biopsies were taken approximately 1 cm from the start and end of all incisions. Slides were prepared with hematoxylin and eosin (H&E) stain and Masson’s trichrome stain.
Histology slide digitization
All slides (H&E and trichrome) were scanned and digitized using a Microtek scanner at 4000 dpi. The area for each scan was individually selected to cover the entire tissue section. The resulting images were used in scar area and width measurements.
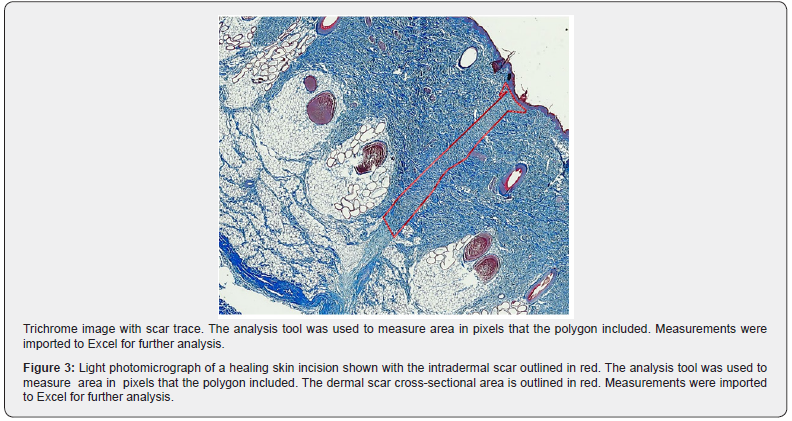
Scar area measurement methods
The amount of granulation tissue surrounding each incision was calculated from cross sections of scar tissue stained with Masson’s trichrome. Images were opened in Photoshop and displayed with the red channel only, which allowed ready assessment of scar tissue. A polygon was traced around the boundary of scar down to the dermal-subcutaneous junction. Images were converted back to RGB format and a red trace was added on top of the polygon with the stroke tool (Figure 3). Analysis of variance (ANOVA) was used to determine any statistically significant differences (0.05 level) across the blade groups at each time point.
Visible scar width measurements
Using the same Masson’s trichrome images from the scar area measurements, the visible scar width was measured for both the start and end of the incision. The two measurements were averaged and the average value was reported for scar width. All measurements were taken perpendicular to the skin surface as opposed to the scar orientation. Only the 60-day slides were reviewed.
Results
Animal response
Twenty-one animals underwent general anesthesia and postoperative recovery in a large animal research facility. All animals survived. Pain was well managed with analgesics and the animals ate regularly. There were no animals that developed a wound infection or dehiscence. The protective vests were effective in preventing the animals from rubbing their incisions against the stalls. The animals continued to gain weight throughout the postoperative observation period.
Analysis of digital photographs
Figure 4 gives the digital photos of scar information in the 5-day study. Images were taken at incision location 2 of animals (Figure 2), which were cut by Beaver, CMC_1 and CMC_2 blades, respectively, on the day of surgery (day 0) and 3 and 5 days postoperation. The start and end of incisions are oriented as shown at the top of each column. The redness appears to decrease dramatically from day 3 to day 5. Wounds remained closed at all time points and no obvious sign of infection was observed.
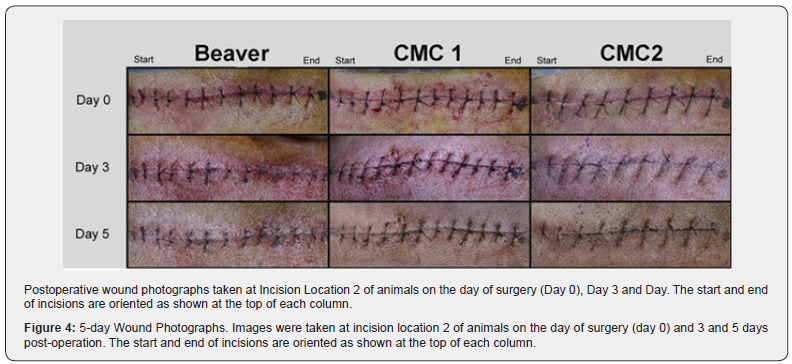

Figure 5 shows the digital photos of scar formation in the 60- day study. Images were taken at incision location 2 of animals, which were cut by Beaver, Ion Infusion and CMC_1 blades, respectively, on the day of surgery (day 0) and 30 and 60 days postoperation. Hair on the back of pigs grew in and around wounds by day 30. Wounds appear flat and somewhat depigmented compared to normal cutaneous tissue. Redness in wounds was minimal by day 30. Some scarring occurred adjacent to incisions due to suture placement, but most likely did not have a significant effect on histological measurements since biopsies were taken between suture segments. Moreover, it appears that the redness of the incisions created by the polished blades decreased faster than the others (Figures 4 and 5), which indicates that this type of blade may result in reduced tissue damage and inflammation.
Scar area measurement results
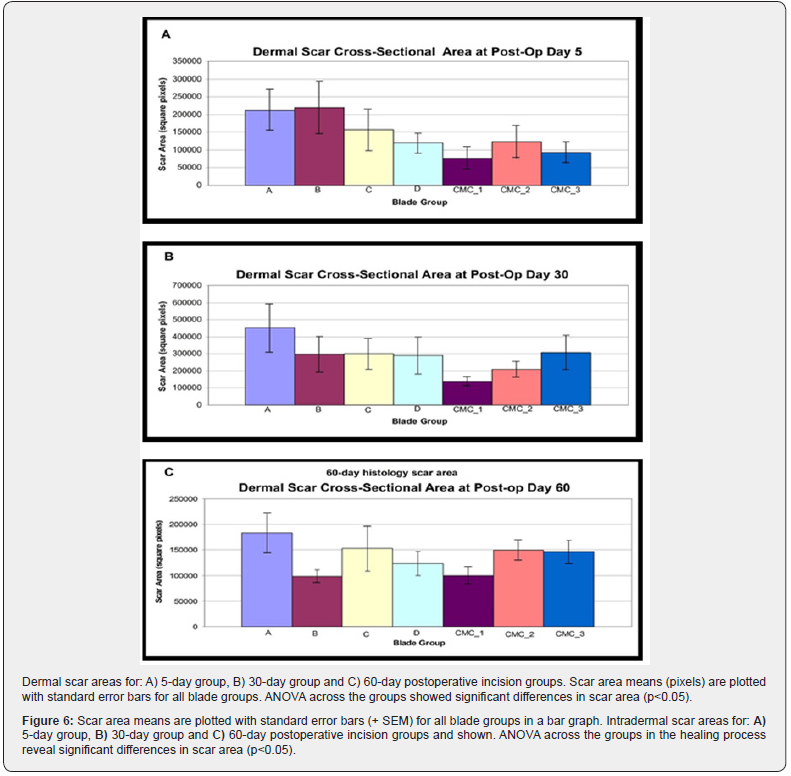
Figure 6 gives histology scar area at 5, 30 and 60 days, respectively. Nearly all blade groups had lower means with a near monotonically downward trend with improved finish, and compared to control ( Bard-Parker #15) at all time points except group B (Beaver blade) at day 5. ANOVA analysis showed significant differences in scar area across the blade groups (p<0.05). We find CMC_1 has significantly smaller means (with 95% confidence) when compared to the all other blades in the 5-day study and the 30-day study.
Visible scar width measurements results
The width of the visible scar is what is seen after surgery and healing is complete. The 60-day group was chosen to represent the remodeling phase of the wound healing process. It was found that in this group we had significantly less variation in the width of the visible scar when using CMP-processed blades as compared to the control (95% confidence). In addition, Figure 7 shows that the CMC_3 blades have a significantly tighter distribution than any of the commercial blades when comparing the width of the visible scar (95% confidence). This could be very important when considering what marks are left behind after surgeries.

Discussion
The conventional cold steel scalpel has long been and remains the most widely used surgical device because of its accuracy, simple design and ease of use. However, in order to improve the wound healing process, various other surgical devices such as the diamond-blade laser scalpel, CO2 laser, Shaw heated scalpel, and electro scalpel have been explored to reduce tissue injury and scar formation and to quickly establish [1-3,5,6,13]. Most of those instruments use heat energy during surgery, which might cause problems including thermal tissue damage, diminished tensile strength, decreased incision precision, delayed wound healing, longer inflammation, and less defined wound borders [1-3,5,6,13]. In addition, there is no evidence that those devices reduce final scar formation. The ultrasonic scalpel has been investigated and the results did not support that it is a better surgical device than the conventional cold steel scalpel (Sinha 2003). Meanwhile, compared with the cold steel scalpel, the previously mentioned surgical instruments are much more complicated, which indicates a higher cost for the surgical process. Therefore, improvement of the design and finishing process of current scalpels could possibly provide a more efficient and feasible way to enhance wound healing after surgery. A typical blade is manufactured by punching a blank from a thin strip of steel, followed by metallurgicalhardening, and subsequent rotary grinding of the edges. A grinding wheel consists of a ceramic binder and numerous embedded individual synthetic diamond crystals that stand proud from the ceramic binder. During grinding, the diamonds plough into the steel, leaving a series of quasi-parallel gouges approximately equal to the height of the diamonds. The diamonds have a breadth of heights and diameters, and may be fractured or released during grinding, all of which adds to the irregular blade topography. From Table 1, we see a roughness average of between 250 and 400 nm for the commercial offerings, while advanced polishing takes the surface roughness to 25 nm.
At the intersection of the two ground surfaces is the primary cutting edge where the largest incisional forces occur. A rough blade edge and surface will naturally widen the wound compared to a smooth surface. However, there may be more than simple surface geometry in play. A histological comparative analysis of conventional scalpel wounds and those produced by a mid- IR laser [14] demonstrated that the standard scalpel leaves an incisional gap of 40-120 microns arising from the blade, but also leaves a wake of damage an additional 400 microns on either side of the wound ascribed by the authors as damage to the extracellular matrix fibers. We speculate that the ragged edge from the grinding operation catches, snags, and tears these fibers, whereas the polished blade has no such topography to engage the fibrous matrix. Thus, the hypothesis is, ‘Would applying the proprietary polishing technology to surgical cutting tools result in reduced tissue damage, subsequent inflammation, and improved scarring?’ Since scarring is associated most commonly with excessive tissue disruption or inflammation, it is proposed that surgical instruments designed to reduce tissue injury or an inflammatory response would provide a substantial benefit to surgical patients with regard to scarring. From the images of the blades (Figure 1) and roughness data (Table 1), we can see that blade edges and fascia smoothness are much-improved, suggesting a basis for reduced friction, drag, and tearing at the cellular level.
The polished blades appear to have benefited wound healing by reducing the inflammatory response, which has been indicated by faster de-redness in the all polished blades (Figure 4). This is because the blades have more uniform edges and a smoother surface, which presumably might cause less para-incisional cell and matrix injury and therefore induce less inflammatory response. Moreover, the polished and more uniform cutting surface may also address a common surgeon’s complaint that the ragged and ground metal cutting surface employed today has high variation in quality and consistency; thus the polishing process could allow for surgeons to perform surgery in a more controlled and predictable way. However the cutting forces and feel with polished blades will differ somewhat from conventional blades, and surgeons employing the new scalpels would need to adapt to slightly different cutting forces both laterally and downward. We make three observations of the data that support the hypothesis. First, many of the pairwise comparisons of blade surface finishes show significant benefits at 95 and 90% confidence; second, we see a near perfect monotonic trend toward improvement in outcomes when compared to type of surface finish; and finally, many of the blade pairwise comparisons show reduced variances in outcomes to 90 or 95% confidence. We feel that these three measures are indicators that blade surface does indeed have an important influence on physiological outcomes, which is consistent with the data we had obtained previously on Guinea pigs [9], where we reported faster wound closure, reduced trauma, as well as improved scarring using the more finished blades.
Volozhin et al. [4] studied time courses of wound healing of laser and scalpel incisions using a rat model. The scalpel wound was smaller than that of the laser before 10 days but wound healing in all groups was mainly complete by the 15th day and there was no obvious difference between the two groups at that time point. This phenomenon is believed to be a delay of the wound healing process, which is due to local tissue damage by thermal energy or other factors during the surgical process. Similarly, in our experiments, compared with polished blades, the wounds created by the other blades had a later healing process. This is because more extensive injuries of epidermis and formation of a larger dense scab on the wound surface were seen in the cases of the as-received ground metal blades, which possibly inhibit reepithelization at the incision site. The injury of tissues and cells by all blades induce an inflammatory response which stimulates collagen biosynthesis. However, prolonged inflammation is usually related to increased fibrosis, which is not favorable in an optimal wound healing process. Therefore, reduced inflammation caused by polished blades would benefit wound healing.
Histological analysis was used to evaluate scar area for each wound. Histology has been widely used in wound healing assessment. However, most of the evaluations have been qualitative (Millay 1987, Sinha 2003). In those cases, analog scales were used and the evaluations were done by visual examination by physicians or pathologists. While those evaluations could provide some useful information for the wound healing progress and comparison, the results might not be objective and lack quantitative support. In this paper, the histology slides from the experiments were digitalized and the images were processed and analyzed by the software as described in the “Materials and Methods” section. The quantitative measurements of the scar area and skin width were generally repeatable and self- consistent. The scar area results suggested the trend towards less scar formation for the increasingly polished blades. Also, the CMC_3 blades produced less scar width and smaller width variance than the other blades (Figure 7). We suggest that reduced scar width and smaller variance are due to less tissue injury induced by surfacefinished blades because of their more uniform surfaces and edges (Figure 1). The variance of some scar area measurements was high (Figure 6). We recognize that there are several sources of variation that cannot be perfectly controlled including animal-toanimal physiology, incision-to-incision variation, and wound-towound location. Moreover, the population size, seven subjects in each group and five incisions for each type of blade in the current experiments, though is generally acceptable for meaningful statistical data analysis, still restricts further result interpretation.
Conclusion
The study in this paper examined if reduction in blade surface roughness can improve wound healing and achieve less scar formation. The highly polished blades appeared to benefit wound healing by reducing tissue damage and the inflammatory response. The scar areas evaluated by the histological study showed significant differences to 95% between any of the blade groups. A considerable decrease in scar areas was observed in polished blades compared with the control group at all time points. Polished blades also demonstrated less scar formation than all the commercial blades at day 5 (CMC_1 and CMC_3) and day 30 (CMC_1 and CMC_2). CMC_3 blades had significantly smaller scar width and width variance than the commercial blades at day 60 (p < 0.05). All the results suggest that polished blades may benefit wound healing by generating less tissue damage and reducing inflammatory response.
Acknowledgement
The authors appreciate the technical support of Anita Mehta, PhD and Casey Hathcock, PhD in conduct of the testing protocol. The funding for the project was provided by Cabot Microelectronics Corporation.
References
- Vincent JG, Doting J (1989) From Flintstone to diamond blade: a new multifunctional instrument for use in coronary surgery. Eur J Cardio-thorac Surg 3 :373-375.
- Vore SJ, Wooden WA, Bradfield JF, Aycock ED, Vore PL (2002) Comparative healing of surgical incisions created by a standard "bovie," the Utah Medical Epitome Electrode, and a Bard-Parker cold scalpel blade in a porcine model: A pilot study. Annals of Plastic Surgery 49: 635-645.
- Millay DJ, Cook TA, Brummett RE, Nelson EL, O’Neill PL (1987) Wound –healing and the Shaw scalpel. Archives of Otolaryngology-Head & Neck Surgery. 113: 282-285.
- Volozhin AI, Merkulov SY, Eliseenko VI, Danilin NA (1991) Time course of healing of experimental laser and scalpel wounds of the skin. Bulletin of Experimental Biology and Medicine 11: 884-886.
- Sinha UK, Gallagher LA (2003) Effects of steel scalpel, ultrasonic scalpel, Co-2 laser, and monopolar and bipolar electrosurgery on wound healing in guinea pig oral mucosa. The Laryngoscope 113 (2003): 228-236.
- Fukuda Y, Ito Y, Azumi H, Eid NAS, Li ZL, et al. (2002) Cell death and proliferation in Nd-YAG laser, electrocautery, and scalpel wounds on mice skin. Journal of Dermatological Science 28: 106-118.
- Li Yuzhou (2008) Microelectronic Applications of Chemical Mechanical Planarization, ISBN 978-0-471-71919-0, Wiley Interscience, New York, USA.
- Clifford Spiro, George Steuer, Frank Kaufman (2005) Method of sharpening cutting edges USPTO Patent US7037175B1.
- Zhang Z, Despa F, Yu N, Chioffe M, Spiro CL, et al. (accepted, manuscript in revision) Effect of scalpel cutting edge roughness on wound healing response. Journal of American College of Surgeons.
- Zhu KQ, Engrav LH, Gibran NS, Cole JK, Matsumura H, et al. (2003) The female, red Duroc pig as an animal model of hypertrophic scarring and the potential role of the cones of skin. Burns 29(7): 649-664.
- Xie Y, Zhu KQ, Deubner H, Emerson DA, Carrougher GJ, et al. (2007) The Microvasculature in Cutaneous Wound Healing in the Female Red Duroc Pig Is Similar to That in Human Hypertrophic Scars and Different from That in the Female Yorkshire Pig. J Burn Care Res. 28(3):500-506.
- Spiro CL (2019) Note added in proof. This work was originally sponsored by Cabot Microelectronics, Aurora, IL where the scalpel polishing process was originally developed and where the blades used in this study were produced. As such, we have retained the original product designation CMC_1,2, and 3 in the text in 2018, all rights to this technology were transferred to Entrepix Medical, LLC, of Phoenix AZ, 85034, now the sole source provider of these products.
- Keel DM, Goldman MP, Fitzpatrick RE, Butterwick KJ (2002) Diamond laser scalpel vs. steel scalpel: A side by side comparison of cutaneous wound healing. Lasers in Surgery and Medicine 31: 41-44.
- S Amini-nik, D Kraemer, ML Cowan, P Nadesan, et al. (2010) Ultrafast Mid-IR Laser Scalpel: Protein Signals of the Fundamental Limits to Minimally Invasive Surgery. PLoS ONE 5(9): e13053.






























