Assessment of Clinical Outcomes of Pedal Arteries Angioplasty for Patients with Critical Lower Limb Ischemia in Suez Canal University Hospital
Hatem H Mohamed, Mohamed M El Yamany, Meera R Boulos* and Sherif A Reffat
Consultant Histopathologist, Panjab University, India
Submission:August 08, 2020; Published:September 16, 2020
*Corresponding author:Dr. Meera R. Boulos, Vascular and Endovascular Unit, Department of Surgery, Suez Canal University Hospital, Ismailia, Egypt
How to cite this article:Anubha B. Assessment of Clinical Outcomes of Pedal Arteries Angioplasty for Patients with Critical Lower Limb Ischemia in Suez Canal University Hospital. Open Access J Surg. 2020; 12(1): 555830. DOI: 10.19080/OAJS.2020.12.555830.
Preface
Background: Patients with lower extremity peripheral artery disease (PAD) experience substantial functional disability due to claudication, rest pain, and minor or major tissue loss [1]. Arterial revascularization is the optimal treatment to prevent limb loss. Several clinical trials have reported that the existence of pedal artery disease results in worse wound healing. Hence, adjunctive revascularization procedures for pedal artery disease might improve the rate of wound healing [2,3].
Aim of the study: To evaluate the clinical outcomes of pedal arteries angioplasty among patients with critical lower limb ischemia regarding severity of rest pain, duration and rate of wound healing. Patients and methods: Between June 2017 and January 2019, this study was carried out as an interventional study on 30 consecutive CLI patients who underwent infra-genicular endovascular revascularization, using Planter Loop Technique then divided into 3 groups complete PAA, incomplete PAA, non-PAA. Study was conducted in Vascular Surgery unit, Department of Surgery Suez Canal University Hospital and to evaluate the clinical outcomes of pedal arteries angioplasty. Results: On table post-procedural foot angiography showed 10 patients (33%) had successfully PAA, 12 patients (40%) had incomplete PAA and 8 patients (27%) had non-PAA. The mean (and standard deviation) of the ABPI raised from 0.53 (+/- 0.22) before the intervention to 0.926 (+/- 0.108) post procedural. Patients with PAA showed better relieve of rest pain, less duration and rapid rate of wound healing than the others. Conclusion: Endovascular treatment is increasingly becoming the first-choice strategy for patients with CLI. Pedal-plantar arch angioplasty in situation with extensive arterial disease below the ankle in patients with CLI is an adjunctive technique that can help achieve tissue perfusion and subsequently accelerate the wound healing and relieve rest pain.
Keywords:Limb salvage; Pedal arch angioplasty; Peripheral vascular disease
Introduction
Patients with lower extremity peripheral artery occlusive disease (PAOD) experience substantial functional disability due to claudication, rest pain, and minor or major tissue loss [1]. Critical limb ischemia is a major cause of morbidity and mortality worldwide and is characterized by multilevel disease, often involving the tibiopedal vessels. The pedal arch describes the connection between the anterior and posterior circulation in the foot [4]. An intact pedal arch has been associated with improved wound healing, as well as a higher patency rate for bypass grafting and percutaneous interventions for inflow disease [5-7]. Pedal arch intervention should therefore be considered in patients with rest pain, ulcers, gangrene, major tissue loss, with a goal of restoring arterial flow to the tissues [8].
Patients and Methods
This was an interventional study took place in the Vascular Surgery Unit, Surgery department, Suez Canal University Hospital during the period from June 2017 till January 2019.
Inclusion criteria: included
i.Both sexes ages from 18 -80 years old.
ii. All patients with critical lower limb ischemia involving the foot present with one or more of the following: Rest pain not relieved for 2 weeks, Ulcer of toes or forefoot not healed for 6weeks and Gangrene of toes or forefoot.
iii. Patients with normal or non-significant stenosis at common iliac artery, common femoral artery and upper superficial femoral artery are suitable for antegrade trans-femoral pedal arteries angioplasty.
Exclusion criteria: included
i. Patients refuse to be included in the study.
ii. All arterial lesions associated with A-V malformation and aneurismal dilatation.
iii. Patients presented with proved vasculitis.
iv. Patients who are not fit for angioplasty as:
v. Patients with Chronic liver disease if there is prolonged PT.
vi. Patients with Heart failure if the patient is orthopneic and cannot lay on table for long time).
vii. Patients with impaired renal function. Procedures and methods
i. Detailed history.
ii. Full vascular examinations.
iii. Imaging & investigations (CTA & Duplex).
Technique
i. Patients fasted for 4 hours pre-operative, then the procedure was performed under local anesthetic (5-10 ml of 1% lignocaine).
ii. Site of arterial puncture: antegrade puncture of the IPSIlateral CFA.
iii. Every case was studied individually, the procedure was done in operation room under complete aseptic technique, and mobile C arm (Philips flat panel C arm 15 KW) with vascular imaging capabilities.
iv. Patients was placed supine. The ipsilateral common femoral artery was punctured using a single-piece 18-gauge needle. After selective wiring of the superficial femoral artery, an 11-cm-long, 6-F Terumo introducer sheath (Terumo Interventional Systems, Somerset, NJ) was place. Heparin 50 IU/ kilo was given IV, half of the dose was given when the procedure continued for more than one hour.
v. Baseline angiography was performed to obtain pictures of the femoropopliteal tract, as well as below the knee vessels (BTK) and foot vessels.
vi. Regarding on table pre procedural angiography, all cases had diseased infra-genicular vessels. According to Kawarada [2] classification which described three types of pedal arch disease, we found that all cases had absent pedal arch (APA); as they had neither of the dorsalis pedis artery nor none of the plantar arteries were patent and the circulation of the foot was established through collateral vessels.
vii. Once baseline angiography is obtained, the revascularization strategy was planned. The lesions may be crossed trans-luminally or subintimal.
viii. A 0.018-inch (Boston Scientific, V-18 control wire, 0.018 x 300 cm) hydrophilic guide-wire was advanced into the occluded pedal artery with the support of a microcatheter 0.018 in all presenting cases as our 1st choice. V-14 (Boston Scientific, V-14 control wire, 0.014 x 300 cm) was tried after V-18 failure confirmed.
ix. The use of appropriate x-ray equipment capable of subtraction angiography and magnification is crucial to carefully navigate the wire through the anastomotic connections between the dorsalis pedis and plantar artery. A very useful trick is to bring the balloon catheter to the distal dorsalis pedis or plantar artery and then to inject contrast locally to assess a possible road of connection. The availability of a low-profile, dedicated balloon catheter is then very important to follow the wire through tortuous vessels. Local injection through the balloon catheter can also be used to confirm the correct intraluminal position before inflation.
x. Specifically, two approaches can be attempted in each patient: (1) antegrade recanalization of the anterior tibial artery and the dorsalis pedis followed by retrograde recanalization of the plantar artery and then of the distal posterior tibial artery or (2) antegrade recanalization of the posterior tibial artery and the plantar artery followed by retrograde recanalization of the dorsalis pedis and then of the distal anterior tibial artery.
xi. The inflation should last between 60 and 180 seconds. The balloon size for foot vessels and plantar arch is usually 2.5 mm. The inflation pressure ranges between 7 and 10 atm, and the anastomotic region is included in the target segment undergoing dilatation. Associated femoral, popliteal and tibial vascular lesions if found were treated as well.
xii. After inflation, the balloon was retrieved, while leaving the guidewire in place, to perform digital subtraction angiography and appraise post percutaneous transluminal angioplasty (PTA) results. If angiographic success is apparent, the guidewire was retrieved, and final control angiography was performed. Otherwise, subsequent inflations at higher pressure or with larger balloons was performed for any residual stenosis greater than 30%.
xiii. Routinely or If spasm occurred, 0.1–0.2 mg of nitroglycerin was infused as an intra-arterial in bolus.
xiv. On table post-procedural angiography of the foot was used to divide the patients into the following three groups according to the post-procedural angiography status of the pedal arch: complete pedal artery angioplasty (complete PAA), incomplete pedal artery Angioplasty (incomplete PAA) group, and non-pedal artery angioplasty (non PAA) group.
xv. After the procedure, homeostasis was achieved with Manual compression of the accessed PA (7-10 minutes), followed by a compressive bandage was performed in all procedures.
xvi. Technical success was defined as restored patency with no stenosis greater than 30% as per reporting standards. A poor result was defined as improvement in patency but with stenosis greater than 30% whilst failure will be defined as no change in patency or failure to cross the lesion.
xvii. Post procedural medication: All patients were medicated on: LMWH (low molecular weight heparin) for 3 days and Dual anti platelets for 3 months.
Follow-up for both groups
ABI, symptoms, pulses & duplex were assessed in these intervals: Next day, After one week and Every month till 6 months post procedural.
Results
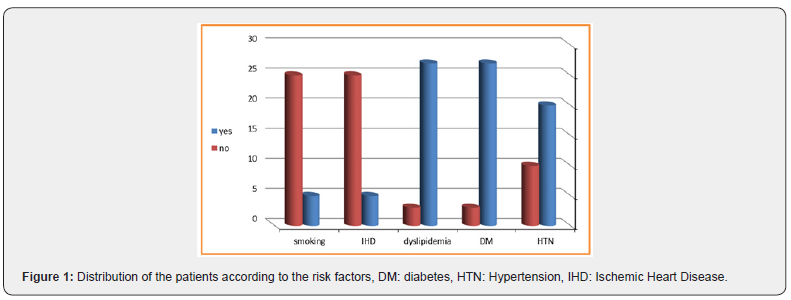
Between June 2017 and January 2019, 30 consecutive CLI patients underwent infra-genicular endovascular revascularization at our vascular unit in SCUH. The ratio of male to female patients nearly equal; 16 men (53.3%) and 14 women (46.7%) with a mean age of 61.63 ± 8.865 years. Regarding the risk factors, 27 patients (90%) were diabetics, 20 patients (67%) were hypertensive and 5 patients (17%) had ischemic heart disease. Regarding the dyslipidemia, 27 out of the thirty patients (90%) were positive. Only 5 patients were smokers and they were all males, while only 5 of the females reported negative smoking, as shown in Figure 1.
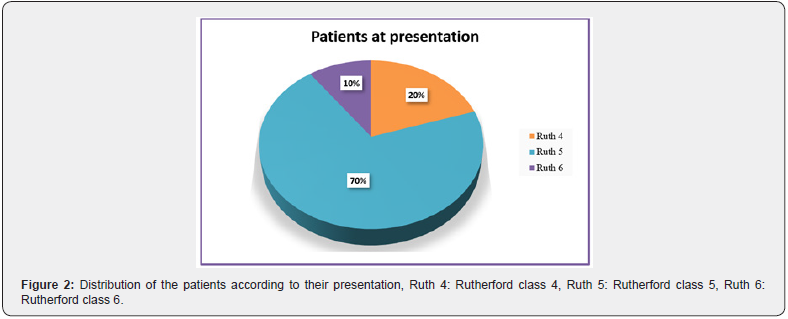
Regarding the presenting symptoms, 6 of the patients (20%) presented with ischemic rest pain (Rutherford class 4) which was of grade 7 according to pain scale, three patients among the latter group had associated toes discoloration. We also found that 21 patients (70%) presented with minor tissue loss (Rutherford class 5), while only 3 patients (10%) presented with superficial heel gangrene (Rutherford class 6), as shown in Figure 2.
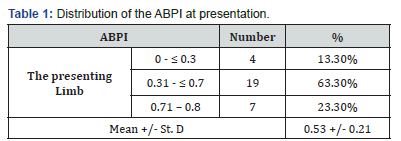
Concerning, Ankle brachial index pre-intervention: ABPI in the presenting limb ranged between 0 and 0.8 with a mean of 0.53 (+/- 0.21), as shown in Table 1.
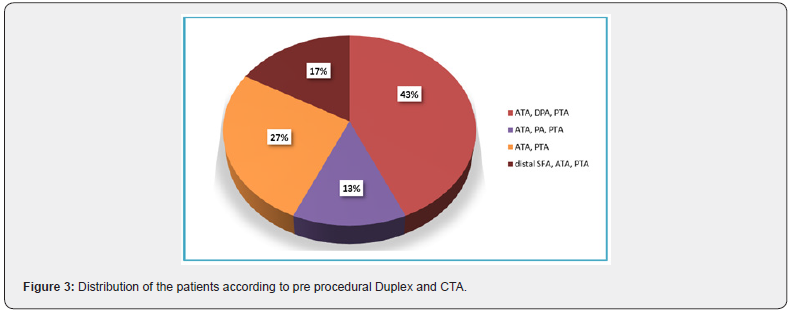
Regarding pre procedural Duplex and CTA; it showed that only 5 patients (16.6%) had significant distal SFA lesion associated with tibial disease, as shown in Figure 3.
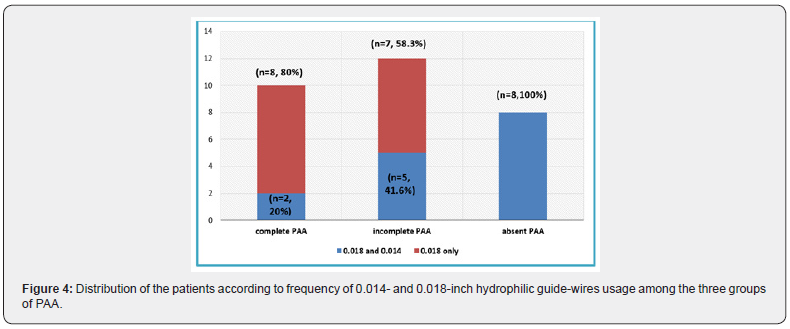
On table diagnostic angiography showed that all cases had diseased infra-genicular vessels, diseased pedal vessels and absent pedal arch. Angioplasty was carried on using planter-Loop technique. Complete PAA was achieved in 10 cases, 8 patients using V-18 and 2 patients using V-14 wires following V-18 trial. Incomplete PAA was achieved in 12 cases, 7 patients using V-18 and 5 patients using V-14 wires following V-18 trial. Non PAA was done in 8 cases despite both V-14 and V-18 trials, (p = 0.003, significant), as shown in Figure 4.
In all patients with non PAA, we failed to cross the pedal arch using 0.018 or 0.014-inch hydrophilic guide-wire, as shown in Figure 5.
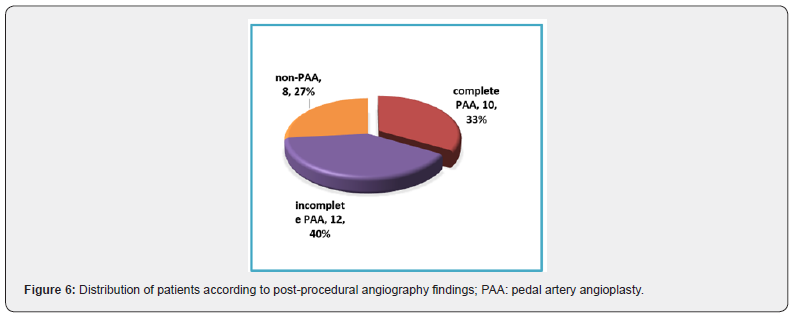
In such cases, unfortunately we were not able to use retrograde pedal and digital access techniques as they usually require an adequate access site, which was very restricted due to ulcers and infections. Five patients among 8 cases who had non-PAA (62.5%) and 9 patients (75%) among 12 cases who had incomplete PAA had associated foot wounds or infection obscuring distal access site. Retrograde pedal and digital access techniques were not feasible even in the remaining non wounded cases as they had extensive pedal artery disease disturbing their original arterial mapping, and the foot blood supply was depending mainly on the patency of the newly developed collateral channels between them. On table post-procedural angiography of the foot was used to divide the patients according to the pedal arch status into the following three groups; 10 patients (33%) had successfully PAA, while 12 patients (40%) had incomplete PAA. Eight patients (27%) had failed pedal artery angioplasty (non-PAA) and ended up with tibial angioplasty only, as shown in Figure 6.

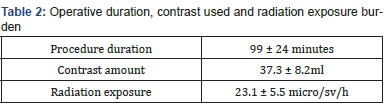
Average duration of the procedure, contrast used and radiation exposure burden are shown in Table 2. All surgeons working adherent to the operation table were wearing radiation personal protective equipment. During the hospital stay, all 27 patients (90%) presented with tissue gangrene, foot wounds or toes discoloration, underwent aggressive wound management. Surgical treatment of the wound consisted of debridement without bone resection in 4 cases (13.3%) while toe/ray amputation was done in 13 cases (43.3%). On the other hand, 7 patients who presented with patches of dry gangrene (23.3%) or those 3 patients who presented with toes discoloration (10%) underwent conservative management with no further surgical intervention post angioplasty as the gangrene shortly started to slough and the discoloration disappeared later during their post operative period, as shown in Figure 7.

Also, the mean (and standard deviation) of the ABPI raised from 0.53 (+/- 0.22) to 0.9 (+/- 0.07) at by the end of 6th month follow up period, as shown in Figure 8.
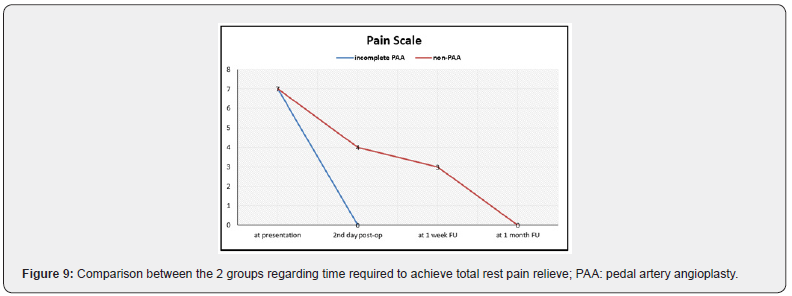
Regarding, during the 6 months follow-up period, all 6 patients with rest pain (grade 7) at presentation reported total relieve of symptoms post procedural. Those who had incomplete PAA reported more reported faster relieve of pain than those who had non PAA, (p = 0.008, significant), as shown in Figure 9.
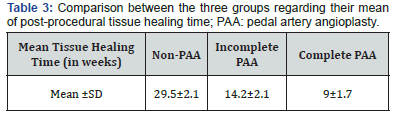
Concerning, During the follow-up, patients with PAA showed more dramatic rapid wound healing more than the others, with P=0.001, as shown in Table 3, and Figure 10.

During the follow-up, neither of the recovered patients reported recurrence of symptoms nor loss of the previously retrieved distal pulse. Only one patient started to develop infective gangrene of the adjacent toe which was treated by surgical debridement for the infective toes. None of the patients developed neither extensive foot infection nor gangrene nor required major limb amputation. The following are 2 case examples that underwent PAA.
Case 1: Sixty years old female patient, diabetic. She presented with dry gangrene over fore-foot and distal phalanx of RT big toe, ischemic ulcer at dorsum of RT fore-foot. By clinical examination, palpable femoral pulsation bilaterally, non-palpable pop nor Tibial pulsations, Rt LL ABPI was over ATA and PTA 0.8. Duplex showed that she has occluded PTA, distal peroneal a., DPA. Ballooning Angioplasty of peroneal a., ATA, DPA and complete PAA was achieved. First day post-op palpable ATA, PTA, ABI 1 over both ATA, PTA. The patient showed similar results over her periodic FU visits after one week up to 6 months. Fore-foot dry gangrene sloughed, and ischemic ulcer healed within 2 months, as shown in Figure 11 & 12.



Discussion
Critical limb ischemia secondary to infra-genicular PAD is associated with high amputation and low survival rates [9,10]. The re-establishment of pulsatile flow to the pedal and plantar arches in below the knee region is a key factor to foot and limb salvage [11,12]. The demographic data and risk factors of the studied patients were as expected for this type of disease [13-15]. Although the sample size was small, but diabetes, hypertension and hyperlipidemia all were prevalent among the studied group of patients. Most of the patients in this study were diabetics (90%), hypertensive (67%) and dyslipidemia (90%); which is similar to Mohammed Ali et al. [16] study which is a similar research conducted here at Egypt.
Regarding the presenting symptoms, a study conducted in Japan by Tatsuya Nakama et al. [17] involving 275 patients showed that most enrolled limbs, 200 limbs (77.8%) were classified as Rutherford Class 5. Is spite of different sample sizes, our study shows similar results as 21 cases out of 30 of the presenting patients (70%) presented with minor tissue loss (Rutherford class 5). Nakama et al. [17] also showed that 128 involved limbs (49.8%) underwent surgical debridement or minor amputation [17]. Nevertheless, all 24 patients (80%) in our study presented with tissue gangrene or foot wounds underwent aggressive wound management as well. That implies that all patients involved presented with critical limb ischemia.
This was associated with low mean ABPI (0.53 +/- 0.21) in this study. This is common in similar studies in the same community [18], which may reflect an awareness or financial problems that prevent the patient from seeking medical advice in early stage of this disease. This, most probably, should affect the outcome of management for such cases, making the comparison of interventional outcome with the international publications difficult. Complete PAA was achieved in 10 cases; 8 patients using V-18 and 2 patients using V-14 wires following V-18 trial. Incomplete PAA was achieved in 12 cases; 7 patients using V-18 and 5 patients using V-14 wires following V-18 trial. Non PAA was done in 8 cases in spite of both V-14 and V-18 trials. On the other hand, several studies such as Nakama et al/ [17], Nicola et al/ [19] and Manzi et al. [20,21] studies all showed that the procedure was performed using 0.014-inch hydrophilic guide-wire as their 1st choice mainly in all cases. Nakama et al. [17] reported successful crossing of occluded pedal vessels using V-14 in 140 patients (54%) who underwent PAA, while in the remaining 117 patients (45.5%) failure to cross the pedal lesion occurred. However, Nicola et al. [19] showed that they successfully achieved complete PAA in 42 patients (30.7%), incomplete PAA in 60 patients (43.8%), and non-PAA in 35 patients (25.5%).
On the other hand, Mohamed Ali et al. [16] study that was conducted in Egypt as well had the same 0.018-inch hydrophilic guide-wire used in their procedure. By applying the aforementioned protocol, they successfully managed to cross the pedal-plantar arch lesions in 19 (90.5%) patients, and failed to cross the pedal-plantar arch lesions in two (9.5%) patients and unfortunately, they ended up in below-the-knee amputation owing to an associated extensive tibial artery disease and aggressive foot infection. That may imply that both wires have comparable results regarding passing the pedal arch vascular lesions. We used a low profile dedicated 2.5 mm balloon catheter in 22 cases. Complete and incomplete PAA was achieved in 10 and 12 patients consecutively. On the other hand, 3 mm balloon catheter was used in all tibial angioplasty. These results are consistent with the previous mentioned studies [16,17,19-21] as they used different low-profile balloon catheters all ranged between 2-3 mm for same range of inflation time.
In all patients with non PAA or incomplete PAA, we failed to cross the pedal arch using 0.018 or 0.014-inch hydrophilic guide-wire. In such cases, unfortunately we were not able to use retrograde access techniques as they usually require an adequate access site, which was very restricted due to ulcers, infections or extensive pedal artery disease disturbing their original arterial mapping, and the foot blood supply was depending mainly on the patency arterial collaterals. These restrictions were found and proved in other studies as well [11,22-24]. Some technical solutions were introduced but still controversial. Angiosomeoriented direct revascularization, which might improve the blood supply toward target wounds, is a widespread strategy [8,25]. However, other studies showed that the effectiveness of the angiosome concept is still controversial [26]. Based on the fact that in patients with pedal artery disease, original angiosome mapping is already destroyed, and the blood supply toward the target wounds depends on the patency of the newly developed collateral channels [17]. These results are consistent with those of Azuma et al. [27] and Attinger et al. [28] as well. For example, our study shows that regardless the angiosomal blood supply dilated in the cases, all of them showed slowly progressive incomplete wound healing by the end of our 6 months follow up period. Thus, this support the argument that the angiosome theory is not totally effective in patients with pedal artery disease.
Our study shows that patients who underwent PAA showed a higher rate of complete wound healing and shorter time to heal than patients without PAA. These results are similar to Mohammed Ali et al. [16] study as 19 (90.5%) patients got their wounds completely healed during 3 months duration. Utsunomiya et al. [29] and Nakama et al. [17] showed similar results as well. During 6 months follow-up period, neither of our patients reported recurrence of symptoms. Only 3 patients (10%) started to develop infective gangrene of the adjacent toe which was treated by surgical debridement for the infective toes. None of the patients developed neither extensive foot infection nor gangrene nor required major limb amputation. On the contrary, Mohammed Ali et al. [16] study showed that during the one year follow-up, two patients underwent limb amputation owing to failed crossing of the pedal-plantar arch and only one (6.25%) patient underwent limb amputation after one year, while all the remaining patients had complete wound healing within 6 months duration. Khalil et al. [30] highlighted similar results where the major limb amputation at one year was 4%.
Conclusion and Recommendations
i. Endovascular treatment is increasingly becoming the first-choice strategy for patients with CLI. Pedal-plantar arch angioplasty in situation with extensive arterial disease below the ankle in patients with CLI is an adjunctive safe technique that can help achieve tissue perfusion and subsequently accelerate the wound healing and relieve rest pain. We recommend the following:
ii. Pedal arch angioplasty can improve the clinical outcomes with accelerated wound healing in patients with CLI.s
iii. We successfully were able to pass pedal vessel lesions using V-18 guide-wire in most cases whether they had complete or incomplete PAA; therefore, it represents a fine 1st choice in CLI cases with extensive pedal disease.
iv. The pedal plantar loop technique is a safe and feasible technique and appears to provide a proper revascularization of the foot arteries.
v. Further studies in this research area with larger sample size, more equipment, and different techniques and longer follow up period.
vi. Provide proper health education to all patients with possible risk factors.
References
- Hulbert KF (1965) Torticollis. Postgraduate Medical Journal 41(481):699-701.
- Chandler FFA, Altenberg A (1944) Congenital muscular torticollis. JAMA 125(7): 476-483.
- Valentino K, Tothy AS (2020) Fibromatosis Colli- a case report. Adv EmergNurs J 42(1): 13-16.
- Adamoli P, Pavone P (2014)Rapid spontaneous resolution of Fibromatosis Colli in a 3-week old girl. Case Rep Otolaryngol 2014: 264940.
- Chao M, Pegbessou PE (2015) Congenital Fibromatosis Colli or torticollis- it’s diagnosis and management in two cases. Pan Afr Med J 22: 74.
- Smith A, Cronin M (2019)Paediatric neck lumps- An approach for the primary physician. Australian Journal of General Practice 48(5): 289-293.
- Garetier M, Breton S (2012) Fibromatosis Colli. Medical Press41(2):213-214.
- Khan S, Jetley S, Zeeba J, Musharraf H (2014) Fibromatosis Colli – a rare cytological diagnosis in infantile neck swelling. J Clin Diagn Res 8(11): FD08-FD09.
- Image 1 Courtesy: Webpathology.com
- Image 2 and 3 Courtesy: Basic Medical Key.
- Image 4 Courtesy: Research Gate
- Image 5 Courtesy: Pacific group of e-journals.com
- Image 6 Courtesy: Pathology outlines.
- Image 7 and 8 Courtesy: Paediatric and Orthopaedic Pathology






























