A Rare Case of Atypical Accessory Bile Duct: Luschca
Yavuz Pirhan1 and Havva Hande Keser Şahin2*
1Department of General Surgery, Amasya University, Turkey
2Department of Pathology, Hitit University, Turkey
Submission:July 06, 2020; Published:August 24, 2020
*Corresponding author:Dr. Havva Hande Keser Şahin, 1Department of General Surgery, Amasya University Faculty of Medicine, Amasya, Turkey; Hitit University Erol Olçok Training and Research Hospital, Çepni Street. 19100, Çorum, Turkey
How to cite this article:Yavuz P, Havva Hande K Ş. A Rare Case of Atypical Accessory Bile Duct: Luschca. Open Access J Surg. 2020; 12(1): 555828. DOI: 10.19080/OAJS.2020.12.555828.
Keywords: Anomalies of the biliary tract; Cholecystectomy; Accessory Luschka channel.
Introduction
We wanted to share the presence of an atypical Luschka canal that we encountered during gallbladder surgery. Laparoscopic gallbladder surgery started in the first half of the 1990s and is rapidly expanding. Today, laparoscopic cholecystectomy is also widely used and has become the gold standard. Abnormalities of the biliary tract are common due to complex embryological developmental stages. It is known that the rate of anatomic variation in the biliary tract is 10%. 90% of these variations are within the Calot triangle, whose boundaries consist of the cystic duct, the lower liver, and the main hepatic duct [1]. The Luschka channel, the most well-known of these variations, belongs to Type A in the Strasberg classification. Diagnosis is difficult because of late detection of Luschka injury. Non-surgical procedures are used primarily in the treatment, but if treatment fails, surgical treatment is performed. Our studies were carried out in accordance with the Helsinki declaration. Patients included in the study were informed about the procedures to be performed before and after the study. Informed consent was obtained from the patients.
Case

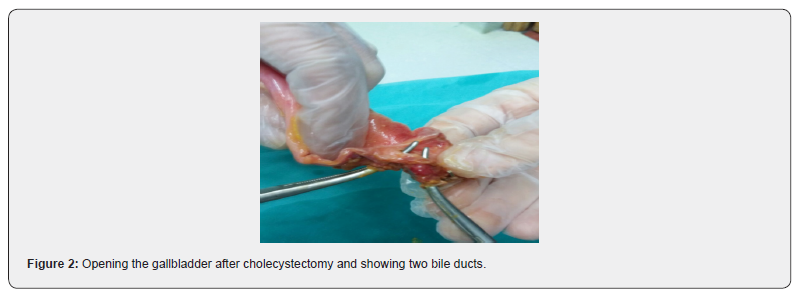
A 56-year-old man presented with dyspepsia and postprandial bloating. As a result of blood tests and ultrasound, the patient underwent surgery for elective laparoscopic cholecystectomy with the diagnosis of many stones in the gallbladder, the largest of which was 1cm in size. During routine outpatient surgery, a cystic artery, a cystic canal and an additional second canal were detected in the region of the CALOT triangle. During dissection, this duct was thought to be an accessory bile duct entering the gallbladder. Cholecystectomy was completed by double clipping this structure, cystic duct and cystic artery. As a result of examination of gallbladder specimen from the operating table, two biliary tracts and one artery which were very close to each other and unconnected were detected (Figure 1 & 2). There were no pathological results in the blood biochemistry tests performed on the 1st and 2nd postoperative days. The patient was discharged on the third postoperative day. No pathology was detected in the control at postoperative 15th and 30th days.
Dıscussion
Due to the complex stages of embryological development, anomalies of the biliary tract are common. It is known that the rate of anatomic variation in the biliary tract is 10%. 90% of these variations are within the Calot triangle, the boundary of which is called the cystic canal, lower liver and the main hepatic canal [1]. Due to anatomic variations, iatrogenic biliary tract injuries (0,2- 2%) are still encountered during laparoscopy [2]. Accessory bile ducts, which are expressed as Luschka, are still controversial in diagnosis and treatment due to their low clinical and incidence rates [3]. Accessory Luschka channel was first defined in 1863. The diameter of the channel is 1-2mm. Although it is located on the surface of the gallbladder, it does not enter the lumen of the gallbladder. It drains the subsegmental areas of the liver [4]. In our case, the diameter of the luschka duct was approximately 3-4mm and about 1cm superior to the cystic duct, coming out of the gallbladder and entering the liver. The actual incidence is still unknown. In the literature, rates ranging from 1-50% are given [5]. It is included in Type A in the Strasberg classification [6]. The mechanism of injury is related to the application of laparoscopic cholecystectomy at a deeper level than it should. Late presentation of the peritonitis due to the small diameter of the accessory Luschka canal and low leakage biliary flow is responsible for the late presentation of the clinic [7]. Another important reason is that there is no realization of injury during surgery. For these reasons, it is the most difficult type of injury to detect during laparoscopy and the latest clinical cause of all bile duct injuries. The clinic usually begins to become apparent about 10 days after surgery [7]. Biochemical parameters do not deteriorate in the early period, but change in the table in which sepsis is settled. In luschka injuries, serum bilirubin values are generally within normal limits. The clinic therefore develops slowly, and patients are generally accepted with symptoms of abdominal pain and sepsis due to bile leakage. Diagnosis begins with suspicion of luschka duct presence, then abdominal ultrasonography, magnetik rezonans colangiopancreaticography (MRCP) and endoscopic retrograd colangiopancreaticography (ERCP) is put. In the treatment, it is possible to expect closure of the accessory canal by drainage of the bile by using percutantran hepatic cholangiography (PTK) in the presence of enlarged intrahepatic biliary tract in proximal Luschka cases [8,9]. In cases that do not improve despite these treatments, drainage of saffron by open or laparoscopic surgery and ligation of the canal detected during surgery [10,11].
Conclusion
In our case, during the dissection of Calot Triangle, the Luschka was thought to be the main bile duct first, and after extensive dissection, it was concluded that this structure was Luschka. During laparoscopic cholecystectomy operations, we recommend that the cystic artery and cystic canal be clipped after the wide dissection of the Calot triangle or even the hepatic triangle in experienced hands. (Patient consent has been obtained for publication in the journal, but it has not been submitted to the Ethics Committee due to the confidentiality of the patient’s identity and the fact that the paper is a case report.).
References
- Senapathi A, Wolfe JH (1984) Accessory cystic duct -an operative hazard. J R SocMed 77: 845-846.
- Spanos CP, Syrakos T (2006) Bile leaks from the duct of Luschka [subvesical duct]: a review. Langenbeck’s Arch Surg 391:441-447.
- Parampalli U, Helme S, Asal G, Sinha P(2008) Accessory cystic duct identification in laparoscopic cholecystectomy Grand Rounds 8: 40-42.
- Aoki T, Imamura H, Sakamoto Y, Hasegawa K, Seyam Y, et al. (2003) Bile duct of Luschka connecting with the cystohepaticduct: The importance of cholangio graphy during surgery. Am J Roentgenol 180:694-696.
- Frakes JT, Bradley SJ (1993) Endoscopic stent placement for biliary leak from an accessory duct of Luchska after laparoscopic cholecystectomy. Gastrointest Endosc39:90-92.
- Strasberg SM, Hetl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopy cholecystectomy. J AmCollSurg180:101-125.
- Russell JC, Walsh SJ, Mattie AS(1996) Bile duct injuries 1989-1993. A statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. ArchSurg 131(4):382-388.
- Prat F, Pelletier G, Ponchon T, Fritsch T, Meduri B, et al. (1997) What role can endoscopy play in the management of biliary complications after laparoscopic cholecystectomy ? Endoscopy 29:341-348.
- Mergener K, Strobel JC, Suhocki P, Jowell PS, Enns RA, et al. (1999) The role of ERCP in the diagnosis and management of accessory bile duct leaks after cholecystectomy. Gastrointest Endosc 50:527-531.
- Stewart L, Way LW (2009) Laparoscopic bile ductinjuries: timing of surgical repair does not influence success rate. A multi variate analysis of factors influencing surgical outcomes. HPB [Oxford] 11(6): 516–522.
- Bektas H, Schrem H, Winny M, Klempnauer J(2007) Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems. Br J Surg 94(9):1119- 1127.






























