Pheochromocytoma Associated with Von Recklinghausen’s Disease: Case Report
Nadjet Azzi1, Meziane El Houcine1, Becherki Yakoubi2*, Radia Ait Chaalal3 and Tabouche Mounir3
1Department of Surgical, BEO University Hospital, Algeria
2Department of Neurosurgical, BEO University Hospital, Algeria
3Department of Radiology, BEO University Hospital, Algeria
Submission:July 03, 2020; Published:August 20, 2020
*Corresponding author:Becherki Yakoubi, Neurosurgical Department of BEO University Hospital, Algiers, Algeria
How to cite this article:Nadjet A, Meziane E H, Becherki Y, Radia Ait C, Tabouche M. Pheochromocytoma Associated with Von Recklinghausen’s Disease: Case Report. Open Access J Surg. 2020; 12(1): 555827. DOI: 10.19080/OAJS.2020.12.555827.
Summary
Pheochromocytomas are neuroendocrine tumors developed at the expense of cells derived from the neural crest. They occur sporadically in 50–55% of cases, but they can be familial in 5 to 10% of cases and then be isolated or integrated into an inherited syndrome of multiple neuroendocrinopathy. The association of von Recklinghausen’s disease and a pheochromocytoma is found in 10% of cases. The properly operated pheochromocytoma is radically and definitively cured as long as it is benign and sporadic.
Keywords: Pheochromocytoma; Von recklinghausen; NEM type1
Introduction
Von Recklinghausen’s disease or neurofibromatosis type 1 (NF1) is a genetic disease with a prevalence of 1/2500 births. Its association with a pheochromocytoma varies from 0.5 to 5%. The latter is most often asymptomatic. Pheochromocytomas are rare neuroendocrine tumors. They are usually benign (3 to 14% of malignant forms). The majority of cases of pheochromocytomas are sporadic, however 10% to 20% are familial forms, isolated or integrated into an inherited syndrome of multiple endocrine neoplasias. We report an unusual historical form associated with a very symptomatic pheochromocytoma [1-3].
Clinical Case
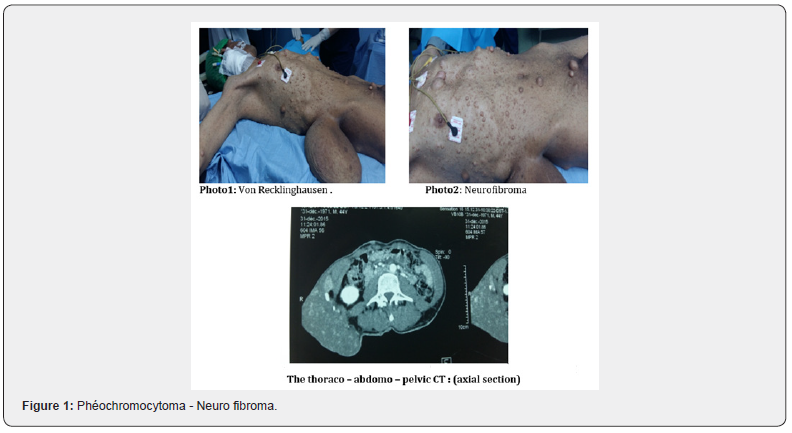
We report through an observation the case of a pheochromocytoma observed in the context of a type 1 neurofibromatosis of Von Recklinghausen photo 1. 43-year-old patient with a family history of NF1 (the mother) consults for hypertension with sweating, palpitations, evoking a pheochromocytoma. It presents “cafe au lait” spots, axillary lentigines, Lisch nodules and disseminated cutaneous neurofibromas, the largest of which measures 30cm photo 2. Biology finds a significant rise in methoxylated derivatives: normetanephrines = 2550nmol / 24h (44-213), metanephrines: 1005nmol / 24h (40–228) and chromagranin A: 900ng /mL (20–115).
The thoraco – abdomo – pelvic CT finds a right adrenal mass of 62 × 60 × 45mm, oval and well limited, discreetly hypodense, increasing heterogeneously after injection of the contrast agent Figure 1. MIBG scintigraphy favoured a neuro-ectodermal process. In addition, he had neurofibromas at the posterior mediastinal, pleural level. The cerebral CT was normal. Doppler ultrasound of the renal arteries did not show stenosis. This patient is referred to surgery for excision of pheochromocytoma and bulky neurofibroma with anatomopathological study [4-6].
Surgery
It is a secretory neuroendocrine process compatible with a pheochromocytoma.
After preparation of the patient, the indication was given for a laparoscopic trans peritoneal adrenalectomy.
Description of the technique:
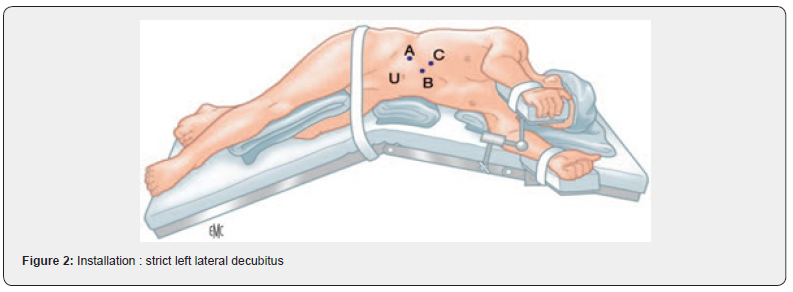
Installation: strict left lateral decubitus (Figure 2) endotracheal intubation (Figure 3), general anaesthesia.
Creation of a pneumoperitoneum by open coelio at the level of the right anterior axillary line. And placement of trocar n ° 10 followed by the other trocars (n ° 10, 10 ,5 ,5) following the left costal awning Figure 2.

1st time: Figure 4(a)
i. Detachment of the peritoneum under the liver to the right triangular ligament.
ii. Incision of the posterior peritoneum along the inferior vena cava, until the location of the middle capsular vein.
2nd time
i. Individualization of the middle Capsular vein (clipped and sectioned) Figure 4(b).
ii. Release of adrenal mass with section of capsular pedicles
iii. Upper and lower Figure 4(c).
iv. Checking the haemostasis
v. Closure of the trocar orifices.

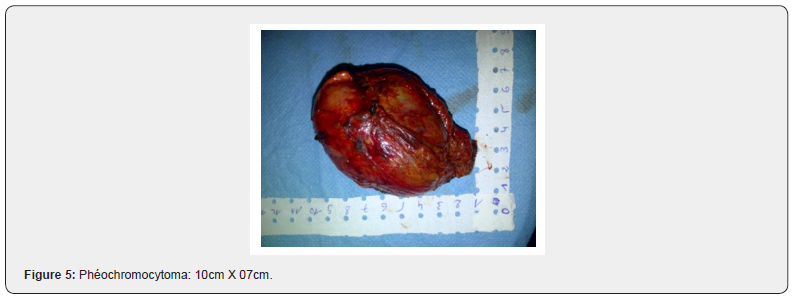
(Figure 5) The anatomopathological study was in favour of a benign pheochromocytoma.
This observation is distinguished by the historical aspect of the clinical picture of NF1 and the very symptomatic character of the pheochromocytoma which is associated with it [6-11].
Discussion
The diagnosis of pheochromocytoma is based on the plasma and urine measurements of methoxylated derivatives; tumor localization is done on imaging (MIBG, CT, MRI scintigraphy). However, when isolated or integrated into an inherited NEM type 1 syndrome; biological screening is compulsory (search for CMT and hyperparathyroidism), however clinical signs (café au lait spots, axillary lentigine, skin neurofibroma, bone lesion) allow the diagnosis of Von Recklinghausen disease to be made. Neurofibromatosis type 1 or Von Recklinghausen disease is an inherited disease caused by a mutation in NF-1 that codes for an activating protein guanosine-5’-triphosphate (GTP). It is an autosomal dominant disease, but in 30 to 50% of cases, the mutation occurs de novo and is post-zygotic.
Neurofibromatosis type 1 is characterized by skin neurofibromas, cafe-au-lait spots, axillary and inguinal lentigines, ocular (Lisis nodules of the iris and optic glioma), skeletal abnormalities and a higher frequency of leukaemia’s and glial tumors. In 0.1 to 5.7% of cases (3.3-13% in autopsy studies), patients develop pheochromocytoma (95% of cases) uni- or bilateral (14%) or paraganglioma of sympathetic origin (6% of cases) which can be rarely malignant (10% of cases).
As the clinical diagnosis of neurofibromatosis type 1 is relatively simple in adults, the genetic test is generally not performed, and it is not indicated in a patient with a sporadic pheochromocytoma. Neurofibromatosis type 1 is a common condition (1/3,500), however the prevalence of pheochromocytoma in NF1 is rare, not exceeding 5%. Neurofibromatosis type 1 is a genetic disease and a rare cause of pheochromocytoma.
Conclusion
Von Recklinghausen’s disease is a hereditary condition, is transmitted in the autosomal dominant mode, which requires genetic screening, because it has a variable expression depending on the individual. The association of Von Recklinghausen’s disease and a pheochromocytoma is found in 10% of cases. The properly operated pheochromocytoma is radically and definitively cured as long as it is benign and sporadic.
References
- Proye C (1999) Les phé In: Chapuis, Peix J C chirurgie des glandes surrénales. Arnette, Paris, France,pp.89-114.
- Proye C (1998) Aspects modernes de la prise en charge des phéochromocytomes et des paragangliomes abdomino-pelviens. Ann chir52: 643-656.
- Brunetti G,Jaud V, Vitris M,Derosier C,Larregle R, et al. (1983) Phéochromocytome en Afrique noire. A propos de 3 nouveaux cas observés en un an à l’hôpital principal de Dakar. Dakar méd28: 421-430.
- Proye C, Thevenin D, Cecat P (1989) Exclusive use of calcium channelblockers in preoperative and intraoperative control of pheochromocytoma : hemodynamics and free catecholamineessays in tenconsecutive patients. Surgery 106:1144-1154.
- Ryan T, Timoney A, Cunningham J (1993) Use of transoesophagealechocardiography to managebeta-adrenoreceptor block and assessleftventricularfunction in a patient withpheochromocytoma. BrJAnaesth70: 101-103.
- Nguessan HA, Keli E, Casanelli JM, Yapo P, Yakpa P, et al. (1990) Pheochromocytoma in black Africa. Report of 9 cases. Chirurgie 116(3): 315-319.
- Paineau J, Blanloeil Y, Legrand D, Pineau M, Letessier E, et al. (1988)Postoperativehypoglycemiaafter excision of pheochromocytoma:A case. Presse Medicale 17(10) : 475-478.
- Billard V, Cheikh M, Delaporte-Cerceau S, Raffin-Sanson L M (2009) Anesthésie pour traitement des tumeurs endocrines. Ann Fr AnesthReanim28: 549-563.
- Wather MM, Hering J, Enquist E, Keiser HR (1999) Von Recklinghausen’sdisease and pheochromocytomas. J urol 162(5): 1582-1586.
- RRabli, HFekak, K Moufid, AJoual, SBenani(pheochromocytome et maladie de Von Recklinhausen.
- Chelou DL, SzoldA, KlausuerJM (2002)The surgicalapproach to adrenaltumors.Harefuah 141(9): 766-769, 860.






























