A Sacred Lesson to be Learned: The Sister Mary Joseph Nodule
Dave N, Kancharla P and Peterson SJ*
Department of Medicine; New York Presbyterian Brooklyn Methodist Hospital, USA
Submission: November 25, 2019; Published: December 13, 2019
*Corresponding author: Peterson SJ, Department of Medicine; New York Presbyterian Brooklyn Methodist Hospital, New York, USA
How to cite this article:Dave N, Kancharla P, Peterson SJ. A Sacred Lesson to be Learned: The Sister Mary Joseph Nodule. Open Access J Surg. 2019; 11(2): 555806. DOI: 10.19080/OAJS.2019.11.555806.
Keywords:Sister mary joseph nodule; Malignancy; Metastatic disease; Skin lesion; Chemotherapy; Abysmal prognosis
Presentation
The involvement of skin from metastatic disease is a relatively infrequent occurrence, moreover umbilical involvement is rare [1-2]. Advances in imaging and lab work has now led to the early recognition of malignancies. We show a patient with clinical evidence of what is formally known as the “Sister Mary Joseph nodule”, which is an extremely uncommon finding of an umbilical mass associated with aggressive terminal cancers. This phenomenon was initially recognized in 1928 by William James Mayo, the son of the founder of Mayo Clinic, where the nodule was observed by his surgical nurse Sister Mary Joseph. Subsequently in 1949 Dr. Hamilton Bailey, an English surgeon, published the term Sister Joseph’s Nodule to represent umbilical metastasis in the textbook “Physical Signs in Clinical Surgery”. A mere 1-3% of abdomino-pelvic malignancies metastasize to the umbilicus even though up to 65% and 28% of these nodules originate from gastrointestinal and gynaecologic origin respectively [3-7]. Patients experience such diffuse metastases that a primary neoplasm may not be found in 30% of cases [3]. Multiple studies report a mere 2-11 month survival from the time of diagnosis of a Sister Mary Joseph Nodule [8-12]. This presentation sheds light on the rapidity and morbidity associated with this physical examination findings.
Patient was a 69 year old male with no reported past medical history who presented with 4 days of abdominal pain, constipation and vomiting. He was noted to have a 7 centimeter wide umbilical mass that was necrotic in appearance that appeared over a 4 day period. This was accompanied by a 20 pound weight loss and decreased appetite over 2 months. There was no history of smoking, no prior endoscopy or familial history of malignancy or liver disease.
Assessment
The patient initially was afebrile and normotensive. His physical examination was significant for a distended abdomen with a necrotic umbilical mass, multiple smaller periumbilical nodules with surrounding erythema and decreased breath sounds at both lung bases. There was no documented jaundice, conjunctival pallor, lymphadenopathy or signs of cachexia. The initial labs showed a high white blood cell count with an elevated neutrophil percentage, a normocytic anaemia, a creatinine of 1.62 (unknown baseline) and mildly elevated liver enzymes. Initial bilirubin was normal (0.7mg/dL) with an aspartate aminotransferase (AST) of 41 and an alanine aminotransferase (ALT) of 82. Tumor markers showed the following results: CA 19-9 of 1635.3U/ML (high), Alpha fetoprotein tumor marker (AFP) of 2ng/mL (normal) and a Carcinoembryonic antigen (CEA) of 46.0ng/mL (high).
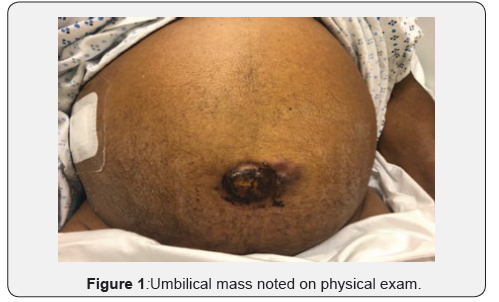
An CT scan showed multiple hepatic lesions concerning for malignancy, soft tissue fullness within the port a hepatis, intrahepatic and common bile duct dilation, soft tissue attenuation of the omentum and increased attenuation at the site of the umbilicus. There was evidence of distal esophageal thickening, distended air and fluid filled small bowel loops, bilateral inguinal adenopathy, bilateral pleural effusions, bilateral lower lobe consolidation and moderate ascites (Figure 1).
Diagnosis
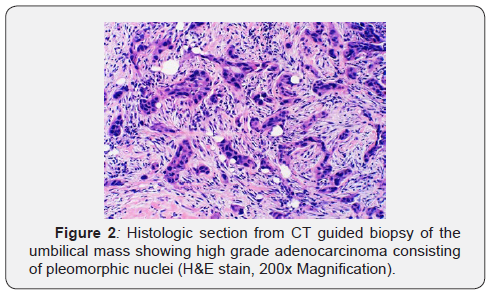
Patient was diagnosed with metastatic cancer of unknown primary, pneumonia and partial small bowel obstruction, preventing early endoscopic investigation. Colonoscopy only visualized the sigmoid with stool obscuring visualization of the rest of the rectum to the descending colon. CT guided biopsy of the umbilical mass was done, showing poorly differentiated adenocarcinoma. Immunopathology was negative for the following markers: CDX-2, GATA-3, PSA, TTF-1 and Napsin-A, making the primary malignancy still inconclusive.
From day 2 to day 9 of admission the patient’s liver function tests showed signs of increasing biliary obstruction with a total bilirubin increasing from 1.3mg/dL to 8.3mg/dL (primarily direct bilirubin). MRCP showed mildly dilated intra and extrahepatic biliary ducts secondary to obstruction by the porta hepatis from malignant implantation, EGD was subsequently normal and Endoscopic retrograde cholangiopancreatography (ERCP) showed a severe single stricture at the level of the middle third of the main bile duct. Brush pathology from ERCP also showed poorly differentiated adenocarcinoma.
Management
Patient’s clinical course was complicated by pneumonia and distal small bowel obstruction. This was later followed by worsening of biliary obstruction likely from implantation of metastatic disease and a polymicrobial abscess of the abdominal wall (superinfection of his umbilical mass). His overall picture portrayed a peritoneal carcinomatosis with liver metastasis and malignant ascites compatible with poorly differentiated carcinoma. The primary was clinically presumed to be hepatobiliary however, the final immunohistochemical stains remained inconclusive. Oncology recommend palliative chemotherapy with possibly 5-FU based with Oxaliplatin or Gemcitabine/Platinum combination as an outpatient. Patient was subsequently discharged home for outpatient palliative chemotherapy. At 1 month follow up the patient was started on modified FOLFOX 6 chemotherapy however, he was readmitted 1 week later for massive ascites. During this subsequent hospitalization the patient was made comfort care and eventually passed away. This patient died, nearly 2 months after presentation with the Sister Mary Joseph Nodule, consistent with the average survival of 2-11 months. This nodule exemplifies very late stage presentation of metastatic disease, which carries an abysmal prognosis (Figure 2).
Authorship
All authors had access to data and a role in writing this manuscript.
References
- Lookingbill D, Spangler N, Sexton FM (1990) Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J Am Acad Dermatol 22: 19-26.
- Steck WD, Helwig EB (1965) Tumors of the umbilicus. Cancer 18(7): 907-915.
- Gabriele R, Conte M, Egidi F, Borghese M (2005) Umbilical metastasis: current viewpoint. World J Surg Oncol 3(1): 13.
- Salemis NS (2007) Umbilical metastasis or Sister Mary Joseph’s Nodule as a very early sign of an occult cecal adenocarcinoma. J Gastrointest Canc 38(2-4): 131-134.
- Urbano FL (2001) Sister Joseph's nodule. (44) Hospital Physician 37(5): 33-35.
- Larentzakis A, Theodorou D, Fili K, Manataki A, Bizimi V, et al. (2008) Sister Mary Joseph's nodule: three case reports. Cases Journal. 1: 182.
- Galvan VG (1998) Sister Mary Joseph's nodule. Ann Intern Med 128(5): 410.
- Trebing D, Göring HD (2004) The umbilical metastasis. Sister Mary Joseph and her time. Hautarzt 11: 186-189.
- Barrow MV (1966) Metastatic tumors of the umbilicus. J Chron Dis 11: 1113-1117.
- Panaro F, Andorno E, Di Domenico S, Morelli N, Bottino G, et al. (2005) Sister Joseph's nodule in a liver transplant recipient: case report and mini-review of literature. World J Surg Oncol 11: 4.
- Piura B (2006) Umbilical metastasis: Sister Mary Joseph's nodule. Harefuah 11: 505-509.
- Khan AJ, Cook B (1997) Metastatic carcinoma of umbilicus: “Sister Mary Joseph’s” Cutis. 11: 297-298.






























