Monomorphic or Multivariate - Eruptive Vellus Hair Cyst
Anubha Bajaj*
Consultant Histopathologist, Panjab University, India
Submission: August 13, 2019; Published: September 04, 2019
*Corresponding author: Anubha Bajaj, Consultant Histopathologist, Panjab University, India Open Access
How to cite this article: Anubha Bajaj. Monomorphic or Multivariate - Eruptive Vellus Hair Cyst. Open Access J Surg. 2019; 11(1): 555803. DOI: DOI:10.19080/OAJS.2019.10.555803.
Preface
An exceptional, developmental anomaly of the vellus hair follicles is designated as eruptive vellus hair cyst. Esterly and Cols initially described a hyper-pigmented, monomorphic, papular eruption and instituted a nomenclature of eruptive vellus hair cyst (EVHC) in 1977. Vellus hair cysts are designated as benign lesions of the pilo-sebaceous unit demonstrating an autosomal dominant mode of disease penetrance. Lesions of eruptive vellus hair cysts can depict a spontaneous retrogression of the eruption. Natural history of vellus hair cysts is inadequately delineated [1]. Eruptive vellus hair cyst belongs to a spectrum of pilosebaceous cysts engendered from the pilosebaceous duct. “Hybrid cyst” is a terminology applicable to the differentiation of a pilosebaceous unit within analogous cysts. Multiple pilosebaceous units engender multitudinous pilosebaceous cysts with an identical pathology such as the frequent concurrence of eruptive vellus hair cyst with steatocystoma multiplex, syringoma, epidermoid cyst, trichilemmal cyst or genodermatoses such as sebocystomatosis [1,2].
Disease Pathogenesis
Eruptive vellus hair cyst is a benign disorder of obscure pathogenesis. Hypothetically, it can be contemplated as a hamartoma differentiating towards vellus hair follicle tissue and is accompanied by an obscurely engendered obstruction within the hair follicular infundibulum along with retained keratinous material and hair fragments, subsequent cystic dilatation of proximal infundibulum and secondary atrophy of hair bulb. Subjects with autosomal dominant mode of disease inheritance elucidate mutations of the keratin gene and demonstrate earlier onset of disease, in contrast to instances of acquired cysts. Primary idiopathic eruptive vellus hair cyst displays a localized discontinuity with subsequent hamartomata’s modifications of vellus hair follicle tissue. Enunciation of cytokines, stress proteins and adhesion molecules are also implicated. Despite the aforesaid theories of adjunctive pilo-sebaceous hamartomata’s lesions, chief stimulus engendering a vellus hair cyst remains obscure [2,3]. Secondary eruptive vellus hair cysts are commonly associated with nonspecific inflammatory cutaneous epithelial reactions occurring as an outcome to diverse aggravating stimuli. Follicular degeneration ensues with accompanying conditions of genodermatosis which inculcate a sequestered, hamartomatous proliferation of pilo-sebaceous epithelial cells with consequent occlusion of hair follicles at the infundibulum along with cystic dilatation of proximal. hair follicular segments and impaction of keratin and hair. Aforesaid theorem enunciates probable hamartomatous evolution of vellus hair cysts. A contemporary notion indicates that eruptive vellus hair cyst is a reactive process rather than a distinctively defined disease and is frequently associated with diverse cutaneous pathological conditions. Commonly the clinical picture is polymorphic associated with a monomorphic histological enunciation and an inconstant inter-relation amidst the two [3,4].
Disease Characteristics
Distribution of vellus hair cyst is contingent to the aggregation of pilosebaceous units , particularly within the implicated zones. Vellus hair cysts are commonly progressive, although non eruptive cysts are elucidated, or eruption can be delayed. Incidence of the frequently elucidated eruptive vellus hair cyst is reported to be at 1.6%. An estimated one fourth (25%) of vellus hair cysts involute spontaneously sequential to trans-epidermal elimination of the cyst or incurrence of foreign body granuloma contingent to inflammatory degradation of the cyst wall. Hereditary variant of eruptive vellus hair cyst was discerned in 1980. Familial incidence and occurrence of the disorder in twins is described. An autosomal dominant mode of disease inheritance is cogitated, and lesions commonly appear at birth or early infancy [2,4]. Genomic mutation of genes encoding keratin 17 are enunciated in the pathogenesis of vellus hair cysts. The condition can be sporadic and often vellus hair cysts appear in the absence of antecedent trauma or a trigger. Aforesaid cysts are enunciated in the first or second decade of life, frequently betwixt 17 years to 24 years, although no age is exempt and a subset of subjects are middle aged, beyond 35 years of age. Acquired and sporadic variants of vellus hair cysts are classified as: Primary idiopathic eruptive vellus hair cysts with spontaneous origin of lesions in the absence of adjunctive cutaneous or systemic disorders. Secondary eruptive vellus hair cysts are associated with adjuvant and variant pilo-sebaceous cysts and various cutaneous inflammatory, immunologic, genetic and metabolic cutaneous disorders. Eruptive vellus hair cysts are devoid of a racial and gender predisposition. Males and females are equally incriminated. Emergence of vellus hair cysts is not contingent to excessive exposure to sun or chemicals or mechanical trauma or application of cosmetics [3,5].
Clinical Elucidation
Vellus hair cysts are commonly underdiagnosed as the condition depicts a paucity of clinical symptoms, variable clinical features accompanied by a diverse classification of clinical skin disorders such as acne vulgaris or keratosis pilaris. Eruptive vellus hair cysts can be misinterpreted on account of an exceptional occurrence and a polymorphic clinical elucidation. Clinical presentation of eruptive vellus hair cysts is ambiguous as it recapitulates clinical manifestations of several pathological conditions. Vellus hair cyst exemplifies a cosmetic disability [5,6]. Eruptive vellus hair cysts depict a specific clinical polymorphism. The terminology of eruptive vellus hair cyst is associated with a plethora of clinical countenances such as a cyst, lesions akin to rice grain, yellow brown, yellow red or blue tinged papules, papulo-cystic lesions and a diffuse, bluish- grey facial discolouration. Eruptive vellus hair cyst can also emerge as persistent acne or comedone like lesions. Vellus hair cysts are commonly encountered in children, adolescents or young adults. Clinically, vellus hair cysts manifest as multiple, asymptomatic, discrete , smooth, reddish- brown, black or skin coloured, elevated, dome shaped, hyper-pigmented papules with a magnitude varying from one millimetre to five millimetres [5,6]. Eruption of vellus hair cyst can be a giant, solitary lesion, multiple, localized or generalized lesions, hyperkeratotic, follicular or non-follicular lesions in addition to the emergence of umbilicated and non- umbilicated lesions with centric puncta. Vellus hair cyst can be discerned universally at comprehensive skin surfaces including sites such as eyelids and labia majora although frequently incriminated sites are chest, abdomen, extremities, neck , axillae, back, face and groin. Punch biopsy or cyst extraction with forceps and an appropriate histological assessment or a fine needle aspiration is diagnostic. Potassium hydroxide preparation for cogent microscopy is beneficial. Aforesaid procedures can be painful and incur scarring [7,8].
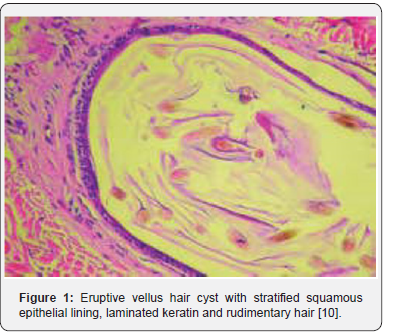
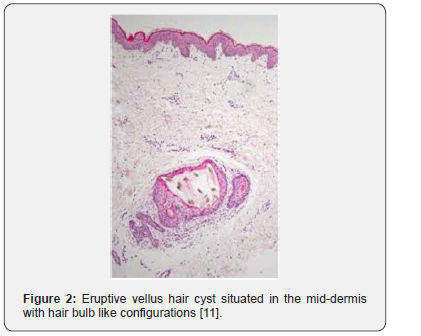
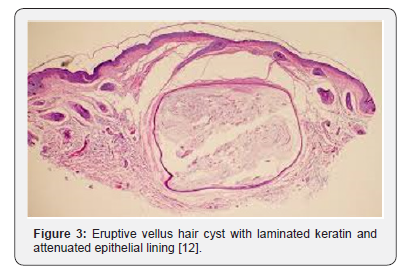
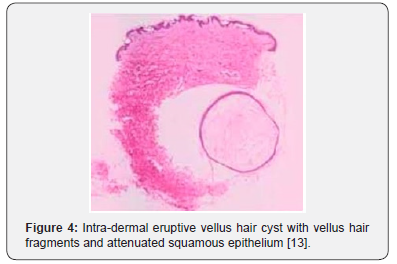
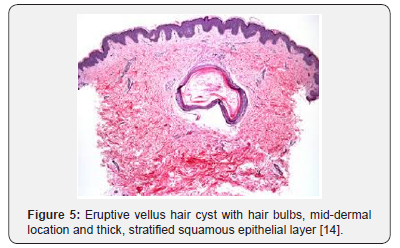
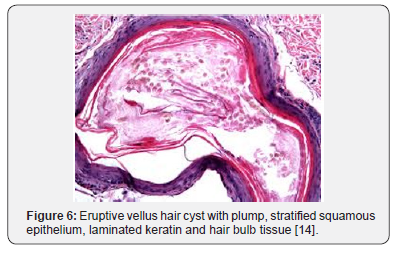
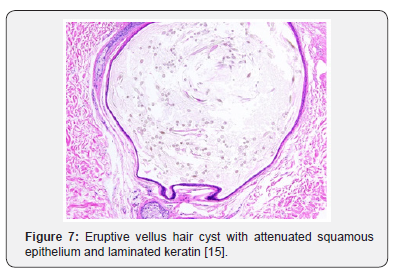
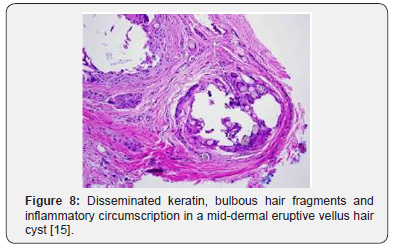
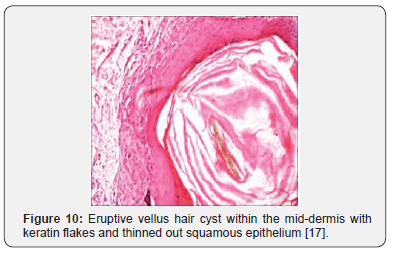
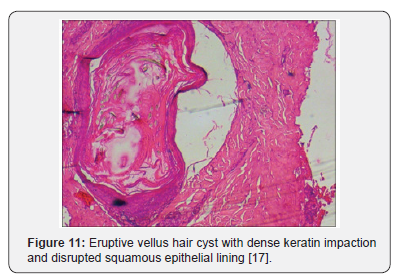
Histological Elucidation
Cogent diagnosis can be achieved on histology as eruptive vellus hair cysts are essentially monomorphic. Characteristically, cystic spaces recapitulate infundibular or isthmic portion of hair follicles and are coated by two to three layers of stratified squamous epithelium with focal granular cell layer. Cysts are enunciated in the upper or mid-dermis with an intra-cystic component of variably quantified, laminated keratin and multiple, transverse or oblique vellus hair [2,3]. Thus, eruptive vellus hair cyst is a mid- dermal keratinous cyst with minimal layering of stratified squamous epithelium encompassing rudimentary hair bulb like configurations. Vellus hair cyst incorporate multiple, fragmented vellus hair shafts and laminated, keratinous material. Cyst wall can be contiguous with atrophied hair follicle or arrector pili muscle. Vellus hair cyst can be encompassed with a granulomatous inflammation with consequent partial destruction of the cyst wall. Serial sections exemplify a lack of sebaceous glands adjoining or within the cyst wall [7,8]. Irrespective of primary or secondary origin of vellus hair cyst, morphology of the predominantly intradermal cysts is monomorphic and depicts a layer of stratified squamous epithelium with cystic contents of vellus hair and keratin. Exponential demonstration of superficial, contiguous, umbilicated lesions with cutaneous orifices can demonstrate exudation of vellus hair from skin pores [8,9] (Figure 1-11).

Immune-Histochemical Elucidation
Immune reactivity for keratin is exemplified with vellus hair cysts . However, discernment of parent cells and origin of cysts remains enigmatic. Vellus hair cysts are immune reactive for antigens of normal hair follicle infundibulum such as keratin 1/10, calretinin, and p63 and depict diminished immune staining for Ki-67 proliferation index within the cyst wall [8,9].
Differential Diagnosis
Pilo-sebaceous cysts necessitate a demarcation from infundibular cysts, steatocystoma multiplex and eruptive vellus hair cysts. Aforesaid cysts can emerge as asymptomatic papules or nodules. However, infundibular cysts are devoid of sebaceous glands or vellus hair components [2,4]. Cysts elucidated in steatocystoma multiplex arise from the sebaceous duct with a configuration of eosinophilic, hyaline, circumferential layering to the cyst wall and an absent granular cell layer. Aforesaid cysts of steatocystoma multiplex incorporate sebaceous glands or sebocytes occurring within the cyst wall. Eruptive vellus hair cysts and steatocystoma multiplex are enunciated as variants of an identical disease spectrum and concurrence of dual lesions are contemplated as “hybrid cysts”. However, dissimilarities ensue on appropriate histological assessment besides divergent immune reactive enunciation of cytokeratin K7 and K10 which further designate eruptive vellus hair cysts and steatocystoma multiplex as distinct entities [3,4].
Steatocystoma multiplex elucidates the dual cytokeratins K10 and K17 whereas eruptive vellus hair cyst usually demonstrates immune reactive K17. Associated singular vellus hair dermatoses are cogitated as “congenital vellus hamartoma”. Initially scripted by Headington in 1976, aforesaid dermatoses manifest miniature papules or nodules situated on the head and neck. Vellus hamartoma is constituted by abundant, well delineated, compact vellus hair follicles. Clinical similarity to a vellus hair cyst is discerned. However, the lesions are devoid of cyst formation on histology [8,18]. Clinical segregation from comedones, keratosis pilaris, syringoma, milia and molluscum contagiosum is required [2,3].
Investigative Profile
Dermoscopic features of eruptive vellus hair cyst are identical to non melanocytic lesions and display distinct, well circumscribed, whitish to yellow spherical arrangements with erythematous or brownish haloes. Centric grey and bluish pinpoint foci are enunciated on account of melanin represented within the pigmented hair shafts confined to the cyst cavity. Contiguity of cysts with superimposed epidermis is elucidated on dermoscopy [18,19].
Therapeutic Options
Currently, the benign eruptive vellus hair cyst is devoid of a standard therapeutic protocol. Derma-abrasion can be adapted as a therapeutic preference apart from employment of erbium YAG or vaporization by carbon dioxide laser and depicts alleviation of lesions to a certain extent [19]. Fine needle incision of the lesions is cogent, however, as the lesions are innumerable, complete resolution may be implausible. Persistent lesions are often resistant to treatment and display inadequate outcomes. Spontaneous retrogression of the lesions can ensue within months to years in the absence of therapy. Topical application of 0.05% retinoic acid cream is beneficial. Oral isotretinoin as a therapeutic modality can be challenging to adopt on account of the side-effects and limited therapeutic benefit [9,18,19].
References
- Esterly NB, Fretzin DF Hermann Pinkus (1977) Eruptive vellus hair cyst. Arch Dermatol 113: 500-503.
- Anand P, Sarin N, Rachita Misri, VK Khurana (2018) Eruptive Vellus Hair Cyst- an uncommon and underdiagnosed entity. J Trichol 10: 31-33.
- Al-Mahmoud BE, Almaslamani HA, Al Hayki NA (2018) Eruptive vellus hair cysts-is it a disease or a phenomenon. J Clin Cosmet Dermatol 2(2): 2826-2827.
- Zaharia D, Kanitakis J (2012) Eruptive vellus hair cyst: report of a new case with immunohistochemical study and literature review. Dermatology 224: 15-19.
- Haritha K, Parthasarathi A (2016) Eruptive vellus hair cyst. Indian J Paediatr Dermatol 17: 76-78.
- Karadag AS, Cakir E, Pelitli A (2009) Eruptive vellus hair cyst: an alternative diagnosing method. Indian J Dermatol Venereol Leprol 75: 537-538.
- Torchia D, Vega J, Schachner LA (2012) Eruptive vellus hair cysts: a systematic review. Am J Clin Dermatol 13: 19-28.
- Bhushan P, Singh A (2014) Facial variant of eruptive vellus hair cyst. Indian J Dermatol Venereol Leprol 80: 96.
- Torchia D, Vega J (2012) Eruptive vellus hair cysts: a systematic review. Am J Clin Dermatol 13(1): 19-28.
- Image 1 Courtesy: Bioline.org.br
- Image 2 Courtesy: Austin publishing group.
- Image 3 Courtesy: Twitter.
- Image 4 Courtesy: Semantic Scholar.
- Image 5 and 6 Courtesy: Dermatology advisor.
- Image 7 and 8 Courtesy: eScholarship.
- Image 9 Courtesy: emedicine Medscape.
- Image 10 and 11 Courtesy: Ijpd.com
- Rodgers SA, Kitgawa K (2012) Familial eruptive vellus hair cysts. Paediatr Dermatol 29: 367-369.
- Espinoza Hernandez CJ, Fonte Avalos V (2013) Eruptive vellus hair cysts: prevalence and clinical features. Gac Med Mex 149: 406-408.






























