Hip Dislocation in Patient with Down syndrome: Case Report and Literature Review
Zaidman M1*, Katzman A2 and Eidelman M2
1Hadassah Medical Center, Jerusalem, Israel
2Rambam Medical Center, Jerusalem, Israel
Submission: March 15, 2019;Published: April 15, 2019
*Corresponding author: Zaidman M, Hadassah Medical Center, Jerusalem, Israel
How to cite this article: Zaidman M, Katzman A, Eidelman M. Hip Dislocation in Patient with Down syndrome: Case Report and Literature Review. Open Access J Surg. 2019; 10(3): 555789. DOI: 10.19080/OAJS.2019.10.555789.
Abstract
Down syndrome or trisomy of chromosome 21 is considered to be the most common chromosome abnormality with the incidence of 1.7 of every 1000 live births [1,2]. The orthopaedic disorders are the next only to the congenital heart disease [3]. Since the effective treatment of heart problems increased survival and life expectancy of the patients with Down syndrome [2-5] the management of orthopaedic disorders became of growing importance. The purpose of the article is to share our experience in treatment of fixed anterior hip dislocation with severe acetabulum dysplasia in child with Down syndrome and to summarize the literature data referred to the incidence of hip dislocation, predisposing factors, hip joint morphology, natural history, conservative and surgical treatment options and their outcomes.
Keywords: Down Syndrome; Hip Dislocation; Salter Osteotomy; Femoral Osteotomy.
Introduction
9 years old girl with Down syndrome was admitted to our institution due to fixed right hip anterior dislocation. The girl’s mother stated her daughter had right hip dislocation at list once a day but was able to reduce it by her own. She was never referred to the doctor because of her hip dislocations before as it seemed not to cause any disability. Her medical history was remarkable for hypothyroidism treated with eltroxin.

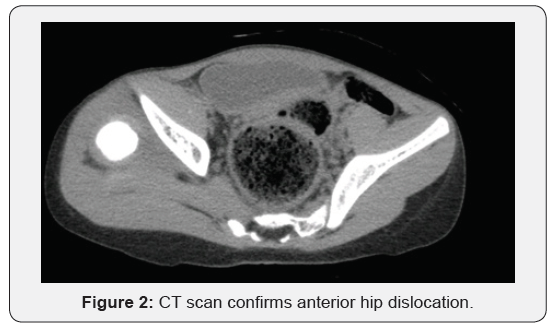
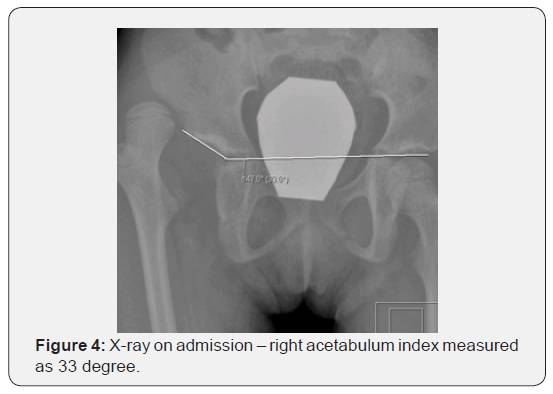
Physical examination revealed prominent limping on ambulation, positive Galeazzi sign (Figure 1), femoral head could be palpated in the right groin region, and the girl was pain free throughout her right hip range of motions. She had generalized join laxity and muscle hypotonia. Radiological examination confirmed right hip dislocation. CT scan demonstrated anterior position of femoral head, shallow acetabulum with severe anterior and posterior wall deficiency (Figures 2 & 3), and signs of soft tissue interposition. Acetabulum index was measured as 33 degree (Figure 4) and femoral anteversion as 70 degree.

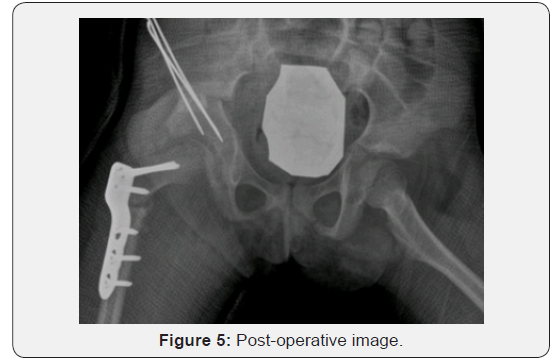
As the attempt of closed reduction under general anaesthesia was unsuccessful because of residual femoral head subluxation and gross instability the girl underwent open reduction with capsule plication, femoral varus derotational osteotomy (VDRO) with one centimetre femoral shortening, Salter osteotomy and one and a half hip spica application. In addition, the bone graft strips were put on the capsule around the acetabulum (Figure 5). Femur was derotated for thirty degree for femoral anteversion correction. Neck shaft angle was ninety five degree after the varus osteotomy. Paediatric locking hip plate (Synthes) was used for femoral osteotomy fixation. The spica cast was removed in 8 weeks after the surgery. The hip joint remained stable on the last follow up visit 12 month following the surgery.
Literature Review
Introduction
Trisomy of chromosome 21 is considered to be the most common chromosome abnormality with the incidence of 1.7 of every 1000 live births [1,2]. Down syndrome is a multi-system disorder. Forty to sixty per cent of patients sustain congenital heart abnormalities [2].
The orthopaedic disorders are the next only to the congenital heart disease [3] and mostly include cervical spine instability, hip subluxation or dislocation, patellar instability, scoliosis, metatarsus varus, pes planus [2-4,6]. Since operative survival for congenital heart disorders and life expectancy dramatically increased in recent years [2-5] the paediatric orthopaedic surgeon more often has to face with the management of orthopaedic problems which are usual cause of compromised walking ability.
syndrome.
Shaw et al. [1] examined 114 patients with Down syndrome with age ranged from ten to 43 years and found 7.9% of overall incidence of hip abnormalities including dysplasia, avascular necrosis or slipped capital femoral epiphysis. 2.9 % of the patients sustained hip joint dysplasia or dislocation. Wolf et al. [6] described the incidence of 1%-7% of hip instability in trisomy 21 patients. Bennet et al. [3] examined 220 institutionalised patients aged 5 to 62 years (average 26 and a half years) and reported the incidence of 4.5 per cents of hip dislocation. Hresko et al. [4] found hip abnormality in 28% of 65 adults with Down syndrome what was statistically correlated with ambulation ability. 18% had hip dysplasia. The authors followed up by serial examinations the subgroup of 18 patients and observed that hip instability could occur in adulthood after skeletal maturity and became worse with time.
Predisposing Factors of Orthopaedic Disorders
Carter et al. [7] investigate the incidence of generalised joint laxity in patients with congenital hip dislocation and in normal schoolchildren. They found the generalised joint laxity in 7 per cent of normal schoolchildren. The per cent was considerably higher in those with congenital hip dislocation. Based on the received data the authors inferred that generalised joint laxity which is often familiar was an important predisposing factor to congenital hip dislocation in boys but less important in girls with exception of familiar cases. Joint laxity and muscles hypotonia are well recognized features of Down syndrome. Most of the authors postulated the generalized joint laxity and muscle hypotonia to be the major predisposing factors of the most of orthopaedics disorders including hip dislocation in Down syndrome [2,5,6,8,9].
Livingstone et al. [10] in his report based on examination of 39 children with Down syndrome related the increased incidence of orthopaedic problems to muscle hypotonia rather than to generalize joint laxity. Applying strict Carter and Wilkinson criteria the authors didn’t reveal generalized joint laxity in children with Down’s syndrome in their series. Shaw et al. [1] suggested the joint laxity to be not predisposing but causative factor. The authors believe that also patients with Down syndrome may have hip dysplasia but more often the joint laxity allows hip subluxation resulting in consequence dysplasia and habitual or persistent dislocation.
Hip Joint Morphology in Patient with Down Syndrome
Shaw et al. [1] studied the roentgenographic anatomy of hip joints in 114 patients. The morphological features they described were deeply seated in acetabulum femoral head, the acetabulum roof – more horizontal. The neck – shaft angle was normal but femoral anteversion was moderately increased. One can expect such anatomical features of hip joint to contribute to femoral head stability in patients with Down syndrome.
Bennet et al. [3] also found the acetabulum of patients with trisomy 21 to be deeper as compared with normal child. Wolf et al. [6] described two cases of bilateral acetabular posterior wall deficiency noted on three-dimensional reconstruction computed tomography. Aprin et al. [8] considered that moderate to severe femoral neck anteversion and increased neck shaft angle are common feature of the hips in patients with Down syndrome.
Natural History
The natural history of untreated hips in patients with Down syndrome suggests progressive function deterioration and secondary degenerative arthritis in adulthood. Untreated unstable hips ultimately end up with fixed dislocation in the late teens or early twenties [5,6].
That corresponds with the results of Bennet et al. [3] based on examination of 220 patients with Down syndrome. According to their data the hips were stable but hyper mobile until the age of two years. Between two till ten years-habitual hip dislocation may occur. Leaving untreated the instability may lead to acute dislocation after the age of seven or eight years. Acute dislocation could be easily reduced under anaesthesia. With time containments is reduced and acetabulum dysplasia progressed. Between late teens of early twenties fixed dislocation occurs but pain usually is not a prominent feature [3].
Hresko et al. [4] reported increased incidence of hip instability in adults with Down syndrome which progressed from mild to severe subluxation or dislocation and can occur after skeletal maturity. Turra et al. [11] described two untreated cases of habitual monolateral hip dislocation in Down syndrome. In one case the year after the onset of hip dislocation the posterior wall smoothing was already obvious on CT scan. In the other case habitual hip dislocation progressed from subluxation to fixed dislocation at the end of 9 years follow up. Increased per cent of hip instability and dislocation observed in adults with Down syndrome [4] supports the progressive feature of the disorder.
Conservative and Surgical Treatment and their Outcomes
Bennet et al. [3] adviced all children with trisomy 21 should be regularly tested for hip instability. The authors considered closed reduction and hip spica immobilisation was only occasionally successful. If the hip joint remained unstable after 6 weeks of hip spica treatment the authors suggested the operative treatment to be carried out. They recommended to full fill capsular plication combined with pelvic or/and femoral osteotomy. Also, the operative treatment was successful only in fifty per cent of patients; the successfully treated patients were doing much better than those left untreated. The best results were if the operation was done at the stage of habitual dislocation. If fixed dislocation was the case, the authors offered leaving it alone as the results of operative treatment at that stage were poor. If the pain was an issue in the phase of fixed dislocation, the authors suggested the Schantz procedure to be done. As a complication of surgical treatment – infection may be a problem.
Wolf et al. [6] described two cases of posterior acetabular wall deficiency with hip dislocation in patients with Down syndrome successfully addressed by modified Pemberton osteotomy to provide better posterior wall coverage of femoral head. The joints left stable more than ten years on the follow up. Packer [12] reported 3 cases of recurrent hip dislocation successfully treated by innominate osteotomy. Immobilisation alone has not provided hip stabilization. One patient had Down’s syndrome and all three children had generalised joint laxity.
Gore [13] treated the posterior hip dislocation in patient with Down’s syndrome by capsule plications with a posterior approach after failed attempts of spica cast immobilization. The hip stayed stable during long term follow up. However, the author could observe subsequent the femoral head subluxation with secondary degenerative arthritis development in 20 years [14].
Kirkos et al. [15] described multidirectional habitual hip dislocation with no signs of hip dysplasia in a 3 years old girl with Down syndrome successfully treated by hip spica application for 12 weeks. The hip remained stable on the 12 months follow up after spica removal. Greene [5] advocated for non-surgical method of treatment of hip dislocation in patient with Down’s syndrome by using the principle of prolong immobilization or casting. He reported his experience of treatment of two children (three hips) at the stage of bilateral habitual hip dislocation by abduction orthosis full time for 6 months followed by night time treatment for additional 4 months (the first case) and complete unilateral hip dislocation addressed by closed reduction and spica cast immobilization for 4 months and ambulatory abduction orthosis for 8 month (the second case). The author believed that non operative management could be successful and avoids such complication as infection which is rather common in patients with trisomy 21.
The increased infection rate after operative treatment was mentioned by Berghof et al. [16] and occurred in 2 cases out of 7. The second or third operation was needed for consequent hip instability following the primary surgery in the author’s series. Bettuzzi et al. [17] described two cases of successful treatment of habitual hip dislocation in 4 years old girl and symptomatic hip subluxation in 11 years old girl with Down syndrome. The authors recommended capsule plication, femur varus derotational osteotomy combined with Pemberton osteotomy.
Aprin et al. [8] treated six patients with Down syndrome (10 hips) with hip dislocation. The authors suggested closed reduction and spica cast immobilization for the first dislocation and operative treatment – for recurrent instability. If the acetabulum was sufficient – the authors recommended capsule plication combined with varus derotational femoral osteotomy, if the acetabulum was dysplastic – Salter Innominate osteotomy should be added. Beguiristain et al. [18] offered femoral derotational osteotomy with capsule plication as a treatment of choice for early stages of hip dislocation in Down syndrome [19].
Discussion
Trisomy 21 is the most common chromosome abnormality. Due to improved management of heart problems life expectancy of children with Down syndrome dramatically increased. Orthopaedic surgeon has to face with management of orthopaedic disorders mostly related to generalized joint laxity and muscle hypotonia. One of the most significant abnormalities which can compromise ambulating ability and to lead to painful condition is hip joint instability. The natural history of hip instability is often progression to habitual hip dislocation which ends up with fixed hip dislocation and degenerative painful osteoarthritis.
Hip dysplasia is relatively rare. Although a few cases of posterior wall insufficiency were reported, the acetabulum tends to be deeper in patients with Down syndrome.
No one of the authors has submitted big enough amount of clinical cases for evidence based conclusion and treatment options recommendations. Most of the authors suggested the attempt of conservative treatment by immobilization to be carried out which could be successful in some cases. If conservative treatment failed – the operative treatment should be undertake and usually included pelvic and proximal femur osteotomy with capsule plication. Better results were described before the fixed hip dislocation occurred. High infection rate and re-dislocation could be an issue.
We described the fixed anterior hip dislocation followed the stage of habitual hip dislocation in 9 years old girl with Down syndrome and classical presentation of generalized joint laxity and muscle hypotonia. The challenge was combined severe anterior and posterior acetabular wall deficiency. Anterior direction of hip dislocation advocated for improving the anterior coverage of femoral head, what could be achieved by innominate osteotomy combined with varus derotational femoral osteotomy.
Because of posterior wall deficiency the main issues of concern were not to create posterior femoral head instability and dislocation by acetabulum reorientation with innominate osteotomy and by over correction of femoral anteversion. However, because of the anterior direction of hip dislocation and gross anterior instability we decided to perform the Salter osteotomy. We corrected 30 degree of anteversion. The posterior hip stability was checked intraoperative. The operated hip remained stable on the last follow up 12 months following the surgery.
Conclusion
Nine years old girl with Down syndrome sustained fixed anterior hip dislocation combined with anterior and posterior wall deficiency was successfully treated by Salter osteotomy, VDRO, open reduction with capsule plication and placing the “bone chips” around the capsule. We believe that chosen option could be a treatment of choice for such complicated presentation. The placement of the “bone chips” on anterior and posterior capsule around the acetabulum could contribute to joint stability in the cases of prominent acetabulum insufficiency. The femoral shortening might be useful in the case of fixed hip dislocation. The case discussion contributes to gained knowledge and experience of hip joint instability management in patients with Down syndrome.
References
- Shaw ED, Beals RK (1992) The Hip joint in Down syndrome: a study of its structure and associated disease. Clin Orthop 278: 101.
- Marder E, Dennis J (2001) Medical management of children with Down’s syndrome. Current Pediatrics 11: 57-63.
- Bennet GC, Rang M, Roye DP, Aprin H (1982) Dislocation of the hip in trisomy 21. J Bone Joint Surg 64-B: 289-294.
- Hresko MT, McCarthy JC, Goldberg MJ (1993) Hip disease in adults with Down syndrome. J Bone Joint Surg (Br) 75-B: 604-607.
- Greene WB (1998) Closed treatment of hip dislocation in Down syndrome. J Pediatr Orthop 18: 643-647.
- Wolf SK, Gross RH (2003) Posterior acetabular wall deficiency in Down syndrome. J Pediatr Orthop 23: 708-713.
- Carter C, Wilkinson J (1964) Persistent joint laxity and congenital dislocation of hip. J Bone Joint Surg 46(B): 40-45.
- Aprin H, Zink WP, Hall JE (1985) Management of dislocation of the hip in Down syndrome. J Pediatr Orthop 5: 428-431.
- Cristofaro RL, Heskiaoff D (1981) Bilateral habitual hip dislocation in a child with Down’s syndrome. Clin Orthop 155: 41-42.
- Livingstone B, Hirst P (1986) Orthopedic disorders in school children with Down’s syndrome with special reference to the incidence of joint laxity. Clin Orthop 207: 74-76.
- Turra S, Gigante C, Iacobellis C (1995) Voluntary hip dislocation in Down’s syndrome: report of two cases. Chir Organi 80(2): 245-248.
- Parker JW, Lefkowitz LA, Ryder CT (1972) Habitual dislocation of the hip treated by innominate osteotomy: A report of three cases. Clin Orthop 83: 184-189.
- Gore DR (1981) Recurrent dislocation of the hip in a child with Down’s syndrome. A case report J Bone Joint Surg 63A: 823-825.
- Gore DR (1999) Recurrent dislocation of the hip in a child with Down’s syndrome: A 20-year follow up. J South Orthop Assoc 8: 67-71.
- Kirkos JM, Kyriakos AP, Margaritis JK, Kapetanos GA (2005) Multidirectional habitual bilateral hip dislocation in a patient with Down syndrome. Clin Orthop 435: 263-266.
- Berghof R, Carstens C (1992) Hip joint problems in patients with Down’s syndrome. Z Orthop Ihre Grenzgeb 130(2): 136-141.
- Bettuzzi C, Magnani M, Lampasi M, Donzelli O (2008) Instability and dislocation of the hip in Down syndrome: report of two cases and proposition of a diagnostic protocol. Minerva Pediatr 60(6): 1445-1450.
- Beguiristain JL, Barriga A, Gent RA (2001) Femoral anteversion osteotomy for the treatment of hip dislocation in Down syndrome: long term evolution. J Pediatr Orthop B 10: 85-88.
- Hensley DC, Schofield GW (1969) Recurrent dislocation of the hip: A case report. J Bone Joint Surg 51A: 573-577.






























