Outcome of Repair of Small Para umbilical Hernias by Onlay Mesh Hernioplasty under Local Anesthesia
Mohammad Kamran CH*
Department of Neuropsychiatry, Malaysia
Submission: April 02, 2018; Published: April 24, 2018
*Corresponding author: Mohammad Kamran CH, Department of Surgery, Allama Iqbal Medical College, Pakistan, Tel: 092-0333 4234231; Email: chmkamran@gmail.com
How to cite this article: Mohammad K CH. Outcome of Repair of Small Para umbilical Hernias by Onlay Mesh Hernioplasty under Local Anesthesia . Open Access J Surg. 2018; 8(5): 555749.DOI:10.19080/OAJS.2018.08.555749
Abstract
Introduction: Repair of paraumbilical hernia by mesh Hernioplasty is a common surgical procedure done worldwide. The ideal site for mesh reinforcement is still debatable and many studies are in progress to show the equally effective outcomes of onlay and sublay mesh reinforcement. Moreover mesh reinforcement under local anesthesia makes the procedure safer and less complicated.
Objective: The present study was to evaluate the outcome of repair of paraumblical hernia by onlay mesh under local anesthesia in terms of repair, pain and complications.
Data collection and analysis: A prospective non-randomized clinical trial done. Sample size was 500 patients (350 females and 150 males) age ranging from 25 to 75 years. Patients having small paraumbilical hernia of 0.5-4cm abdominal wall defects, which were repaired by onlay, mesh reinforcement using prosthetic prolene mesh under local anesthesia. Outcome was measured in terms repair, pain at incision site at 6 and 12 hours and complications. Data was entered and analyzed in SPSS ver: 21.0 and outcome was presented as frequency and percentages.
Results: Out of 500 patients, 120 patients (95 females and 25 males) had chronic liver disease and ascites. 35 had oozing of serous discharge from the hernia. Females included multiparous 93%, primiparous 6% and nulliparous 1% were most affected (70% females & 30% males). Mean age of the patients were 43+11.01 years (p<0.05). Post-operative pain measures on VAS were 2+0.45 at 12 hours.1.6% (08) patients developed Seroma and 1.0% (05) had wound infections.
Conclusion: Onlay mesh reinforcement under local anaesthesia was found to be safer, cost effective, associated with minimum chance of post-operative complications and early return to normal life.
Keywords: Onlay mesh reinforcement; Prolene mesh; Paraumbilical hernia; Ascites; Nulliparous
Introduction
Umbilical and para-umbilical hernia is becoming a relatively common surgical issue. Studies have shown the rising trend in UK [1] i.e. from 5% to 14% as well as in Turkey [2]. Abnormal protrusion of abdominal contents, mesenteric fat, intestines through a weaker area in the anterior abdominal wall closes to umbilicus is called paraumbilical Hernia. Weak spot may result due to defect in the anterior abdominal muscles, rectus sheath or ligaments. The defect may be congenital or acquired [3]. Hernial contents squeeze through the weak spot in the form of protruding hernia sac. Its common complications are strangulation or intestinal obstruction. Commonly women are more prone to develop para umbilical hernias as compared to males. Patients usually present with a visible lump around navel. They approach the surgeons when pain starts and surgical repair is required.
This condition usually becomes painful contents are trapped in the hernial sac leading to palpable lump requiring surgical intervention. Surgical treatment may involve various methods which follow some common basic strategies [4,5]. Basic strategy involved is inversion of hernia sac contents back to the cavity they normally belong then weak spot can be stitched (herniorraphy) or reinforced (Hernioplasty) and hernia is repaired. Most commonly employed surgical intervention involves the closure of weak spot along with insertion of mesh to reinforcement the defective area (Hernioplasty) hence the recurrence chance is minimized. Mesh placement may be done onlay (on anterior rectus sheath) or sublay (below rectus muscles on to the posterior rectus sheath) [6]. Onlay mesh is considered to be a tension free method for repair of abdominal wall defects.
Literature review revealed that several studies declared the onlay mesh reinforcement technique as the best option and this is the most commonly performed technique worldwide. Several studies have compared onlay mesh reinforcement with sublay technique and rated the second one as a poor technique [7]. However the ideal site for mesh reinforcement is still debatable and many studies are in progress to show the equally effective outcomes of onlay and sublay mesh reinforcement and reach an acceptable conclusion [8]. Though its incidence has been increased since the last two decades (1991- 2010, there still seems to be a lack of attention given to this issue in research fields and literature [9].
However it is the need of time to probe in to the problem and find out the most appropriate para umbilical hernia repair options. Keeping above in view, the present study was also planned to explore the effectiveness and failure rate of onlay mesh under local anaesthesia to reinforce the defect causing paraumbilical hernia.
Objective
The objective of the study was to determine the outcome of onlay mesh reinforcement for repair of paraumbilical hernia under local anaesthesia.
Methodology
Present study was carried in the Department of General Surgery Jinnah Hospital Lahore as well as in private hospitals of Lahore from 2000 to 2016. It was a prospective non-randomized clinical trial. Total of 500 patients (350 females and 150 males) age ranging from 25 to 75 years were operated. Patients were randomly selected having small paraumbilical hernia of 0.54cm abdominal wall defects and requiring surgical intervention. Their written consent was taken. Before surgery thorough preoperative evaluation with the help of urinalysis, blood complete picture (CP) and abdominal ultrasound was done. Patients with chronic liver disease (CLD) were also investigated for coagulation profile and arrangement of fresh frozen plasma (FFP) transfusion was made before the start of surgery. Every patient received prophylactic intravenous antibiotic at the time of local anaesthesia infiltration in the operation theatre. Area to be operated was cleaned with antiseptics and intravenous line was maintained with Ringer lactate infusion.
0.5% lignocaine (10ml) with 50mg Bupivacaine (10ml) was used for infiltration anaesthesia. 130ml normal saline was added to these two ampoules of lignocaine and of Bupivacaine (10ml each). Hence total volume of infiltrate was 150ml. Then 0.5ml of adrenaline 1/1000 was also added and the total adrenaline concentration was 1/400,000 in 150ml which was safe and did not affect vital signs like pulse and blood pressure. Adrenaline led to minimum bleeding when incision was given. Most of the time 70 to 100ml of local anaesthetic solution was sufficient to carry painless surgery.
Local anaesthesia infiltration was started from the site of incision, area around the umbilicus and below the site of incision. Syringe (10cc) with 27G needle was used for infiltration purpose. The infiltration was done at a slow rate because rapid infiltration may lead to acute pain. No Sedative was added except a single intramuscular dose of nalbuphine 20mg, a centrally acting opioid analgesic. Material used for reinforcement was synthetic material prolene mesh (Ethicon made) which is a derivative from polypropylene. The procedure comprised of open access to abdominal cavity, squeezing back the contents of the hernial sac (sometimes sacs were opened too) and defect was closed with proline No. 1 before mesh placement.
The prolene mesh was placed over the rectus sheath defect overlapping 4cm from each side in such a way that it completely covers the prevailing defect. Umbilicus was attached with the sheath and normal shape of umbilicus restored. Whereas in most of the patients with CLD, umbilicus had to be removed (umbilectomy) because in ascites the skin overlying the paraumbilical hernia and around umbilicus was of poor quality thus hampering the proper closure of wound. Finally the skin was closed with subcuticular type Vicryl 4/0 sutures so no outpatient visit was required for removal of stitches.
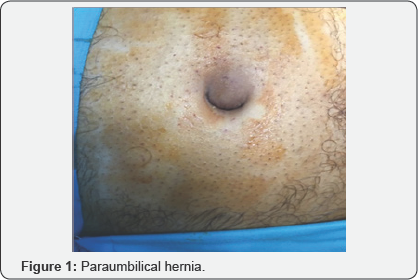
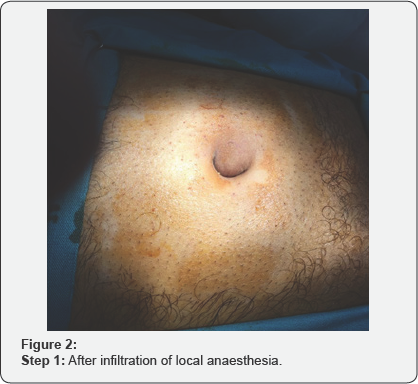
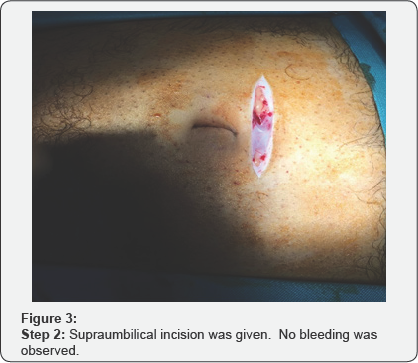
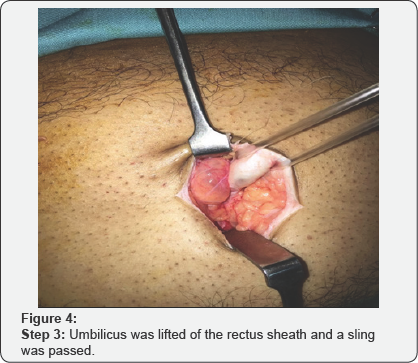
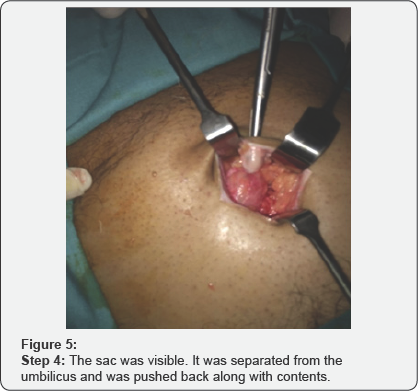



Various steps of the surgical procedures are being shown in (Figure 1-8). For the repair of defects less than 2cm, no suction drain was required. Whereas postoperatively Redivac drain was put in 30% (155 out of 500 patients), which was removed on 3rd to 5th day. The whole Anesthetist remained in the theater throughout the length of procedure. During surgery, patients were comfortable and hemodynamically stable with all vital signs within normal range. All the surgeries completed in 40min (+/- 15min). During this time, no further medication was required or added. All patients were given appropriate antibiotics for five days after the surgery.
Results

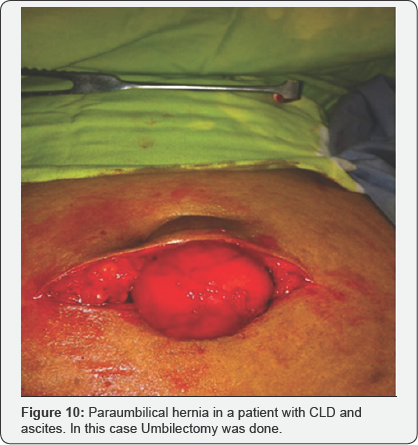
Five hundred patients were included in the study out of which 120 patients (95 females and 25 males) presented with chronic liver disease and ascites creating pressure in abdomen leading to hernia shown in (Figure 9 & 10). 35 patients with ascites showed oozing of thin serous discharge from the hernial site. In the sample, 93% females were multiparous, 6% were primiparous and 1% nulliparous due to some primary infertility related issue. Statistical analysis revealed that paraumbilical hernia was more commonly seen in females (70% females & 30% males) and mean age of developing this condition was 43+11.01 years (p < 0.05).
Post-operative pain scale was zero i.e. no pain at all, for the initial 6-8 hours and even afterwards scale did not exceed 3 (barely noticeable) i.e. 2 +/- 0.45 at 12 hours for which patients were advised to take tablet paracetamol and naproxen orally. Most of the operated patients did not develop any post-operative complication and were satisfied of the selected surgical procedure. However 1.6% (08) patients developed Seroma which was managed by simple aspiration and 1.0% (05) patients developed wound infection which responded to appropriate antibiotics prescribed after culture and sensitivity test. None of the patients needed mesh removal to control the infection.
Discussion
Paraumbilical hernia is very frequently encountered surgical issue affecting females at a higher rate as compared to males and our study also supported this trend. Multiparous elderly females were found to be the most frequent victims of this condition [10]. Literature review revealed that for the past few years the trend for mesh reinforcement hernioplasty is increasing as compared with non-mesh based repair [8]. A randomized clinical trial and 64 months post-operative follow up also revealed that there are less chances of recurrence if hernia repair is done with mesh (~1%) as compared to repair with sutures (~11%) [5]. However the best site for inserting the materials for mesh reinforcement has not been convincingly established till date [11].
Best site for reinforcement would be the one which is simple, least painful, causes minimum discomfort during and after the procedure, has minimum chances of recurrence and least vulnerable to infections [12]. Early methods employed for hernia repair like suturing, manipulation of anatomical structures led to high tension on tissues surrounding the site leading to high rate of recurrence [13,14]. We used conventionally woven polypropylene (prolene) mesh for tension free repair of paraumbilical hernia. Prolene is a synthetic non absorbable material composed of crystalline stereo isomers of polypropylene unsaturated bonds. It possesses greater tensile strength, passes smoothly from the tissues to be repaired and induces minimum antigenic foreign body response. Moreover it doesn't adhere to the surrounding tissues [15].
Onlay mesh was inserted above the rectus sheet to provide additional support to weaker area and repair the small paraumbilical hernias. Interestingly the recovery process in operated patients was rapid, pain scale was 0-1 as muscles were not pulled together or stitched under tension. Patients returned to normal activity within 3-4 days and resumed their jobs and even recreational activities within 4-6 days. One month follow up confirmed the success of onlay mesh as there was no recurrence. Studies have proved that if polypropylene mesh was inserted intraperitoneally, most of the time it led to complications during and after the surgery [16]. Another study selected sublay mesh plasty to treat various types of hernia including paraumbilical and found this technique a better option with minimum chances to develop infection [17].
Whereas in present study the mesh was placed above rectus sheath (onlay) with negligible numbers of complications of seroma and wound infection on follow up. Prolene mesh is the most commonly applied prosthetic mesh and we also used this mesh for open onlay repair. As prolene mesh induced less tissue rejection response, showed minimum shrinkage thus better for onlay repair. As 120 patients presented with chronic liver disease and uncontrolled ascites being the most common threat for recurrence. Studies have shown that more than 20% patients with ascites develop paraumbilical hernia and hernia sac contains ascitic fluid in addition to abdominal cavity contents like peritoneum, omentum and intestines.
In these patients Hernioplasty is difficult and mostly "wait and see" policy is followed [18]. Fortunately during one month post-operative follow up no recurrence was observed. Hence it can be safely claimed that early elective onlay mesh reinforcement can be planned to avoid emergency hernia repair due to any complication like strangulation enhancing morbidity and mortality in theses patient. However ascites control should be strictly taken as a part of post-operative care. Moreover as the surgery was performed under local anaesthesia so patients started physical activities much earlier after surgery, minimum stay in the hospital and did not develop any complication related to general anaesthesia or spinal anaesthesia like urinary retention-a common hazard of old age surgeries [19].
Conclusion
Onlay mesh reinforcement under local anaesthesia can safely be used as a superior procedure to repair paraumbilical hernia as it was found to be cost effective, painless, quick and easy technique, with minimum chance of post-operative infection and thus recurrence. This study evidently overcomes the reluctance of surgeons to use onlay mesh reinforcement as a first choice to treat and repair small paraumbilical hernias.
References
- Dabbas N, Adams K, Pearson K, Royle G (2001) Frequency of abdominal wall hernias: is classical teaching out of date? JRSM Short Rep 2(1): 5.
- Seker G, Kulacoglu H, Oztuna D, Topgul K, Akyol C, et al. (2014) Changes in the frequencies of abdominal wall hernias and the preferences for their repair: a multicenter national study from Turkey. Int Surg 99(5): 534-542.
- Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, et al. (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4): 407-414.
- Velasco M, Garcia Urena M, Hidalgo M, Vega M, Carnero F (1999) Current concepts on adult umblical hernia. Hernia 3(4): 233-239.
- Arroyo A, Garcia P, Perez F, Andreu J, Candela F (2001) Randomized clinical trial comparing suture and mesh repair of umblical hernia in adults. Br J Surg 88(10): 1321-1323.
- Bowley D, Kingsnorth A (2000) Umblical hernia, Mayo or mesh? Hernia 4(4): 195-196.
- Wright BE, Beckerman J, Cohen M, Cumming JK, Rodriguez JL (2002) Is laparoscopic umblical hernia repair with mesh a reasonable alternative to conventional repair? Am J Surg 184(6): 505-508.
- Kulacoglu H, Oztuna D (2011) Growth and trends in publications about abdominal wall hernias and the impact of a specific journal on herniology: a bibliometric analysis. Hernia 15(6): 615-628.
- Rutkow IM (1998) Epidemiologic, economic and sociologic aspects of hernia surgery in the United States in the 1990s. Surg Clin North Am 78(6): 941-951.
- Kulacoglu H, Yazicioglu D, Ozyaylali I (2012) Prosthetic repair of umblical hernias in adults with local anesthesia in a day case setting: a comprehensive report from a specialized hernia center. Hernia 16(2): 163-170.
- Salameh JR (2008) primary and unusual abdominal wall hernias. Surg Clin North Am 88(1): 45-60.
- Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, et al. (2004) long term follow up of a randomized controlled trail of suture versus mesh repair of incisional hernia. Ann Surg 240(4): 578-583.
- Martis JJ, Rajeshwara KV, Shridhar MK, Janardhanan D, Sudarshan S (2011) Strangulated Richters umblical hernia- A Case Report. Indian J Surg 73(6): 455-457.
- Kurzer M, Belsham PA, Kark AE (2004) Tension free mesh repair of umblical hernias as a day case using local anesthesia. Hernia 8(2): 104107.
- Mackenzie D (1973) The history of sutures. Med Hist 17(2): 158-168.
- Godara R, Garg P, Raj H, Singla SL (2006) Comparative evaluation of sublay versus onlay meshplasty in ventral hernias. Internal Journal Surgery 5(1): 187-192.
- Halm JA, de Wall LL, Steyerberg EW, Jeekel J, Lange JF (2007) intra peritoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg 31(2): 423-429.
- Buffone A, Costanzo M, Basile G, Terranova L, Papa V, et al. (2012) Spontaneous rupture of an umbilical hernia in a cirrhotic patient with ascites; a case report and review of the literature. Ann Ital Chir e- publish 1-4.
- Afridi SP, Siddiqui RA, Rajput A (2015) complications of onlay and sublay mesh plasty in ventral abdominal hernia repair. Journal of Surgery Pakistan 20(2): 48-51.






























