AV Malformation affecting Maxillofacial region: A Case Report
Nusrat Nazir1* and Altaf Hussain Chalkoo2
1Post Graduate student, Department Oral Medicine and Radiology, India
2Professor & HOD, Department Oral Medicine and Radiology, India
Received: January 22, 2018; Published: February 20, 2018
*Correspondence author: Nusrat Nazir, Post Graduate student, Department Oral Medicine and Radiology, India, Email: drnusratnaziroma@gmail.com
How to cite this article: Nusrat Nazir, Altaf Hussain Chalkoo. AV Malformation affecting Maxillofacial region: A Case Report. Open Access J Surg. 2018; 8(3): 555737. DOI: 10.19080/OAJS.2018.08.555737
Introduction
Vascular anomalies are a set of changes of blood vessels that could be associated, or not, to endothelial cells proliferation that results in a vascular hamartomatous growth [1]. Arteriovenous malformations (AVMs) are the result of errors of vascular development between the 4th and 6th weeks of gestation [2]. Failure to prune unwanted primitive communications between the arterial and venous systems may result in a malformation. Most of these lesions are obvious at birth while some are obvious during adolescence or adulthood.
It is believed that enlargement is the result of changes in pressure and flow, ectasia, shunting and collateral proliferation, rather than cellular proliferation. AVMs have a tendency to grow with the child and after the individual has attained full growth, AVMs remain stable throughout life. Some enlargement may occur in response to trauma or hormonal disturbances during puberty or pregnancy [3]. Treatment of AVMs can be difficult, as frequently, following an apparently successful extirpation, there is regrowth of the tumour to a size larger than its original size, often with supply by surgically inaccessible vessels [4].
Case Report
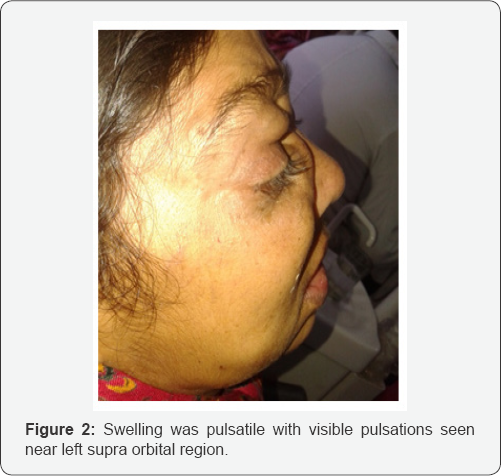
A 45 year old lady reported to the department of oral medicine and Radiology with chief compliant of diffuse swelling of face particularly around eyes since 6 years (Figure 1). The thickness of the lesion was variable. The overlying skin appeared normal over the swelling with no change in temperature or colour and was not associated with pain. Swelling was pulsatile with visible pulsations seen near left supra orbital region (Figure 2). No significant medical history was reported by patient and parents.Based on history provisional diagnosis of AV malformation was formulated and patient was advised one USG of the affected region.

On USG multiple bilateral dilated tortuous AV malformations were seen extending from supraorbital region to neck. Superior ophthalmic vein was dilated on left side. Bilateral proptosis was also present. Eyeballs appeared normal however anterior chamber capsule was thickened bilaterally. There was no evidence of internal hemorrhage. So finally lesion was diagnosed as AV malformation. Further patient was advised one MRI angiography but patient was not cooperative for that hence lost in follow up (Figure 1 &2).
Discussion
AVMs are the result of a failure of regression of the arteriovenous channels in the primitive retiform plexus [5]. They are composed of a central nidus with anomalous congenital shunts between the arterial and venous systems. These abnormal vascular channels may not canalize or conduct blood flow for many years. An enlargement is the result of dilatation of the adjacent arteries and veins (collateralization and recruitment) [6] rather than endothelial proliferation. Fast-flow vascular malformations usually become evident during childhood and puberty. Kohout et al. [7] in their study found that AVMs were present at birth in 59% of cases, in childhood 10% of cases, in adolescent 10% of cases, and in adulthood 21% of cases [8].
In the present case report, AVMs was present in late adulthood. AVMs grow synchronously with the growth of the child. Puberty and trauma are found to have triggered the rapid growth of the lesion leading to the manifestation of symptoms. Holt et al. [9] reported that trauma leading to the AVMs may be penetrating, blunt, postsurgical, or inflammatory [10]. The enlargement occurs due to the change in the pressure and flow within the malformation, ectasia, shunting, and collateral proliferation rather than cellular proliferation [11]. In the present case report, symptoms were triggered insidiously.
AVMs can be diagnosed with:
a. A Duplex or Doppler ultrasound uses sound waves to image your blood vessels and measure your blood-flow speed.
b. Computed tomography angiogram (CTA) uses a contrast agent (dye), which is injected into your vessels, to look for abnormalities. CT scans that do not use dye may also be taken of your head and neck.
c. Magnetic resonance angiography (MRA) combines an injected contrast agent (dye) with magnetic and radio waves to create 3-D cross-sections of the arteries in your neck and brain. An MRI (without dye) creates images of your head and neck.
d. In a catheter angiogram, the surgeon inserts a thin catheter through your groin and threads it into your carotid arteries; a contrast agent (dye) is injected to help clinicians visualize the arteries on X-rays.
Management of AVMs is most difficult due to the replacement of normal tissue by the diseased vessels and high- flow rate of recurrence. This management mainly consists of surgery, vascular embolization, or a combination of both. Surgical treatment consists of wide resection which is difficult and potentially hazardous due to significant blood loss during surgery [12].
References
- Jackson IT, Carreno R, Potparic Z, Hussain K (1993) Hemangiomas, vascular malformations, and lymphovenous malformations: classification and methods of treatment. Plast Reconstr Surg 91(7): 1216-1230.
- Kohout MP, Hansen M, Prebaz JJ, Mulliken JB (1998) Arterio venous malformation of the head and neck: natural history and management. Plast Reconstr Surg 102: 643-654.
- Jackson IT, Carreno R, Potparic Z, Hussain K (1993) Haemangiomas, vascular malformations and lympho-venous malformations: Classification and methods of treatment. Plast Reconstr Surg 91(7): 1216-1230.
- Leikensohn JR, Epstein LI, Vasconez LO (1981) Super-selective embolization and surgery of non-involuting haemangiomas and A-V malformations. Plast Reconstr Surg 68(2): 143-152.
- Kohout MP, Hansen M, Prebaz JJ, Mulliken JB (1998) Arterio venous malformation of the head and neck: natural history and management. Plast Reconstr Surg 102(3): 643-654.
- Holman E (1955) The physiology of an arterio-venous fistula. Am J Surg 89: 1101-1108.
- Marler JJ, Mulliken JB (2005) Current management of hemangiomas and vascular malformations. Clin Plast Surg 32(1): 99-116.
- Kohout MP, Hansen M, Pribaz JJ, Mulliken JB (1998) Arteriovenous malformations of the head and neck: Natural history and management. Plast Reconstr Surg 102(3): 643-654.
- Richter GT, Friedman AB (2012) Hemangiomas and vascular malformations: Current theory and management. Int J Pediatr 2012: 645678.
- Holt GR, Holt JE, Cortez EA, Thornton WR, Young WC (1980) Traumatic facial arteriovenous malformations. Laryngoscope 90(12): 2011-2020.
- Bhandari PS, Sadhotra LP, Bhargava P, Bath AS, Mukherjee MK, et al. (2008) Management strategy for facial arteriovenous malformations. Indian J Plast Surg 41(2): 183-189.
- Hassard AD, Byrne BD (1985) Arteriovenous malformations and vascular anatomy of the upper lip and soft palate. Laryngoscope 95(7 Pt 1): 829-832.






























