Concurrent Salter-Harris Type II Proximal Tibia Fractures Associated with Vitamin D Insufficiency
John T Ruth2*, José Arturo Pacheco Nûñez1 and Joseph E Sheppard2
1National Autonomous University of Honduras School of Medicine Tegucigalpa, Honduras
2Banner University Medical Center, Department of Orthopedic Surgery, Arizona
Received: January 23, 2018; Published: February 02, 2018
*Corresponding author: John T Ruth, Banner University Medical Center, Department of Orthopedic Surgery P.O. Box 245064, Tucson, Tel: 857245064; Fax: 520.626.2668, Email: jruth@ortho.arizona.edu
How to cite this article: John T Ruth, José Arturo Pacheco Nunez, Joseph E Sheppard. Concurrent Salter-Harris Type II Proximal Tibia Fractures Associated with Vitamin D Insufficiency. Open Access J Surg. 2018; 7(5): 555721. DOI:10.19080/OAJS.2018.07.555721.
Abstract
Background: Proximal tibia epiphysis fractures account for 1.8 to 3% of physical injuries, 0.6% of long bones fractures in children, and 30% of partial growth plate arrest. African American children with vitamin D insufficiency (defined as serum 25OHD below than 30ng/mL) have decreased bone mineral density compared to children sufficient vitamin D levels.
Case Description: This case presents the diagnosis, treatment, and outcome of simultaneous bilateral Salter-Harris type II fractures of the proximal tibia, with concomitant fracture of the tibia tubercle in a 14-year-old African American male with insufficiency of vitamin D while running forward.
Literature Review: Bilateral Salter-Harris type II fractures have only been published by Potenza et al. [1] occurring with minor trauma. Although Schilling et al concluded that vitamin D deficiency (serum 25OHD below 20ng/mL) was unlikely to contribute to fractures in young children, data supporting an association of vitamin D deficiency and forearm fracture in African American children was reported by Ryan et al. [2], as well as hypovitaminosis D and upper extremity fractures in James et al. [3].
Clinical Relevance: Health care practitioners should carefully evaluate injuries to the proximal tibia epiphysis in late adolescence to detect missed fractures lines on radiographs. A better understanding of the anatomy of the proximal leg in children and an appreciation of the advantages and disadvantages of the available treatment modalities will aid in determining the best technique required for treatment. Health care practitioners should consider vitamin D screening in African American teenagers in order to reduce the morbidity in at-risk patients.
Introduction
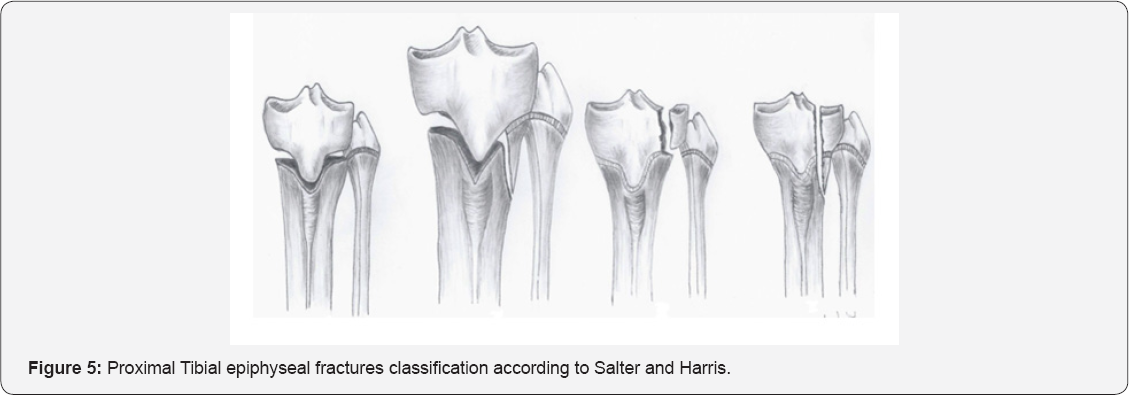
Physical tibia fractures constitute 15% of epiphyseal injuries. They are the third most common fractures that affect the growth plate, following hand phalanx and distal radius fractures. These fractures predominantly occur in overweight, fast-growing males between 8-15 years of age [4-6]. Protective factors for the proximal tibia epiphysis appear to be the epiphyseal plate's irregular shape and the surrounding soft tissue (fibular head ligaments, patellar tendon, insertion of semitendinous and medial collateral ligaments into the proximal metaphysis) [7-10]. The most commonly used classification system is that of Salter- Harris [11], being type II 37% of all proximal tibia fractures in children [1,12], resulting from severe hypertension and valgus strain due to excessive external force [9,12].
A particular flexion-type injury is described as a combination of a Salter-Harris type II fracture of the proximal tibia physis associated with a tubercle avulsion [4]. It results from vulnerability during ossification for tensile forces of the quadriceps muscle on the anterior portion of the tibia growth plate, as this begins to close asymmetrically from posterior to anterior, transmitting the impact by the patellar tendon on the tibia tubercle [4, 11,13-16,]. Simultaneous bilateral Salter-Harris type II fractures are extremely rare and only case reports about them have been published [1]; as it also are a combined fractures of the proximal tibia physis and tibia tubercle [17,13].
Although diagnosis and treatment have previously been well described [14,18,19], there have been no studies of the predisposing weakness of the growth plate that leads to simultaneous fractures without a direct trauma. Vitamin D plays an important role in the bone matrix mineralization of the growth plate cartilage through the regulation of mineral homeostasis [20]. It participates in bone mass recruitment along with a variety of factors, ranging from genetic determinants to nutritional influences [21]. It is noted to increase during times of growth spurt [20].
Certain diseases like endocrine imbalance make the epiphyseal plate more vulnerable to injury and predisposed epiphyseal separation [9]. Although the role of vitamin D in bilateral upper tibia Salter-Harris type II remains unknown, the measurement of vitamin D is becoming more common in physical assessment [20] and may be beneficial in the initial workup of patients with upper tibia Salter-Harris fractures. Treatment of hypovitaminosis D may facilitate postoperative healing in teenage children owing to the fact that the per pubertal adolescent period experiences an increased nutritional and metabolic demand that is secondary to the increased growth during the developmental period [20].
The association between vitamin D insufficiency and a traumatic proximal tibia fracture remains unclear and, to our knowledge, has not been previously reported. The purpose of this report is to raise awareness on the screening of vitamin D insufficiency in African American adolescents, which is one of the most prevalent deficiencies among this pediatric population, as recent studies has highlighted the importance of the effects of vitamin D on adolescent growth [3,22-25] and may be a risk factor for epiphyseal fractures without adequate trauma. This report presents a case of an overweight 14-year-old African- American boy who presented with simultaneous, bilateral, Salter-Harris type II fractures of the proximal tibia with posterior displacement of the epiphysis with a concomitant unilateral avulsion of the tibia tubercle, occurring without a direct trauma, and vitamin D insufficiency.
Case History
A 14-year-old African American boy, with a body mass index of 28 kg/m 2 was playing dodge-ball, felt a "pop" in his bilateral knees while running forward and then fell to the ground in a flexed position. Physical examination was significant for swelling of both knees and extreme tenderness over the joint line. Laboratory findings were significant for a 25-hydroxy-vitamin D value of 22ng/ml. His radiographs revealed both right and leftsided displaced and angulated mildly comminuted Salter-Harris type II fracture involving the proximal tibia, with medial and posterior displacement and angulations of the distal fragments; and fragmentation of the tibia tubercle accompanying the right side (Figure 1A & 1B). After close reduction (Figure 2A & 2B), patient was carried to the operating unit, where the left leg, initially most displaced, was treated first.




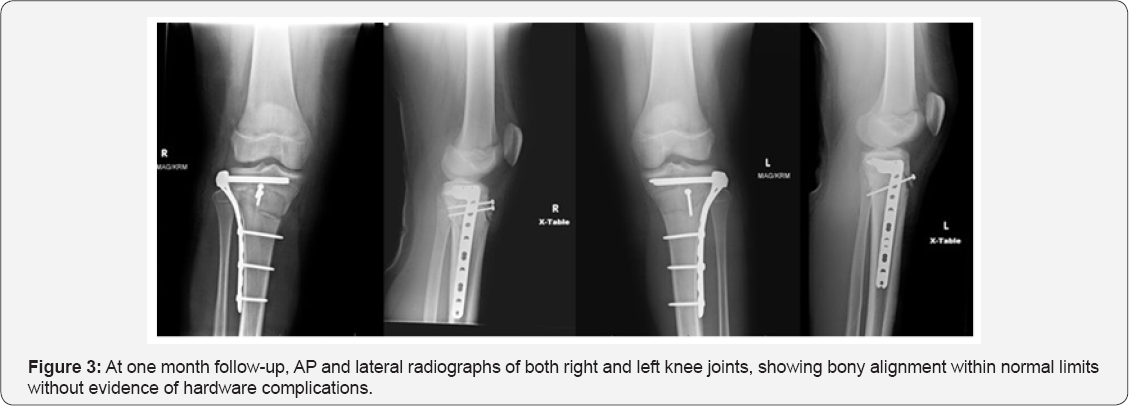
A lateral tibia peri-articular locking plate, locking screws and bi-cortical screws were placed in the proximal fragment parallel to the joint surface reducing it to the proximal tibia. Same procedure was performed in the right side, to addition of the placement of percutaneous lag screws across the tibia tubercle apophysis. At one month follow-up radiographs showed bony alignment within normal limits without evidence of hardware complications (Figure 3). He was seen for one postoperative visit and then lost to follow-up. Was brought back in by his parents seven months later, had not been ambulating and had been using a wheelchair since his injury. Radiographs were taken and showed healed, well anatomically reduced bilateral tibia plateau fractures (Figure 4A & 4B).


Discussion
Proximal tibia epiphysis fractures are rare, accounting for <2% of lower extremity epiphyseal injuries [7,16]. Proximal tibia growth plate fractures are infrequent, with most resulting in anterior, anterolateral, and anteromedial epiphyseal displacement relative to the metaphysis. Rarely, these injuries are caused by rapid knee flexion against the contracting quadriceps during landing. This infrequently results in a Salter- Harris type II injury, an injury that traverses the physis before exiting obliquely across a corner of the metaphysis and the most common proximal epiphyseal injury (Figure 5) [9,26].
Less often, tibia tubercle injuries occur: these are nearly all described in boys aged 15 to 16 years of age with a BMI >28 and caused either by violent contraction of the quadriceps muscle (such as while jumping) or acute passive knee flexion against a contracted quadriceps muscle (while starting or landing a jump) [13,16]. Tubercle injuries present with soft tissue swelling and tenderness directly over the tubercle [14].
The normal epiphyseal plate consists of resting and proliferating cells surrounded by cartilaginous matrix; this gives strength to the epiphyseal plate, particularly resistance to shear forces. Certain diseases, such as hormonal imbalances (Kraus et al. [18]), render the epiphyseal plate more vulnerable to injury, thereby predisposing to epiphysiolysis [9]. In rats, Idelevich et al. [21] showed that calcitriol treatment augments proliferation and directly stimulates growth plate chondrocyte maturation, which later undergoes replacement with primary spongiosa [9, 21].
Although the detrimental effects of vitamin D deficiency on bone growth have been recognized for over a century, the effects of suboptimal vitamin D levels on growth plates have not been fully characterized. Vitamin D plays an important role in bone mineral density (BMD) development [20,27,28] and muscle strength; insufficiency is defined as a 25-hydroxy- vitamin D level of 21 to 29ng/mL according to an Institute of Medicine 2011 report [29]. It influences skeletal integrity by maintaining calcium homeostasis in growth plate chondrocytes matrix mineralization [21,30,31] and aids in the prevention of fractures [30,31]. Sevenler et al. [32] demonstrated in mice that the growth plate mechanical response to shear loading at the micro scale is disrupted by dietary insufficiency of vitamin D. This effect combined with known changes in columnar growth rates induced by vitamin D deficiency, may be an important mechanism contributing to growth plate disorganization and weakness [32] and a predisposing factor to fractures with minor or no trauma. Williams et al. [33] reported an animal model in which the lateral region of the bovine proximal tibia physis was stronger and has a greater tangent modulus than the medial and central regions, which could explain the medial displacement of the proximal fragments in both tibias. Vitamin D insufficiency is more prevalent among African Americans adolescents [23,24], they are more likely than white adolescents to be overweight or obese In addition, darker skin pigmentation is a risk factor for vitamin D deficiency [2,22,24,25].
Ryan et al reported that both lower BMD and vitamin D deficiency (≤20ng/ml) increase the odds of forearm fracture in African American children [2]. In a study of 181 children with upper extremity fractures, James et al found that 41% had insufficient vitamin D levels, and among these children, African American children were more likely to have insufficient or deficient vitamin D levels [3]. Previous reports have noted bilateral Salter-Harris type II occurring either consecutively by Ozokyay et al. [22] with previous osteochondrosis of the anterior tibia apophysis by Merloz et al. [22] or simultaneously resulting from landing from a high jump by Potenza et al. [22]. There are no combined bilateral fractures of the proximal tibia physis and tibia tubercle reported, the few instances reported on the literature have been unilateral [13].
The treatment of proximal tibia physeal fractures follows the general principles of other Salter-Harris physeal fractures [11,34]. A common theme throughout the literature is the difficulty in maintaining the reduction with cast alone, especially with posterior displacement of the tibia [35]. Generally, the results have been satisfactory, although in a study by Shelton et al. [12] type II displaced fractures treated by close reduction and immobilization all suffered from growth discrepancy [12]. In order to prevent angulatory and longitudinal deformities open reduction and internal fixation is recommended. Fracture of the tibia without concomitant fractures of the fibula, as seen in this case, can lead to various malangulation [36].
To prevent the valgus deformity, well performed reduction has to be done, and this has to be accomplished by not leaving interfragmentary medial space [37-40]. In our case the proximal tibia physeal injuries presented with posterior displacement of the epiphysis. There is no clinical and radio graphical history of previous trauma, no Osgood-Schlatter disease, and no landing nor attempting to jump as mechanism of injury. These simultaneous fractures resulted while running, with no direct trauma, suggesting an associate deficit at physeal closure predisposing to the combined bilateral physeal/apophyseal injuries, raising the index of suspicion for bone weakness which makes this case unique.
Because there is a high prevalence of vitamin D insufficiency among African American children and known associated risks of fracture and decreased BMD one may conclude that in deficiency states upper tibia physeal flexion-avulsion injuries may also occur. Although only one patient is described here we suggest considering the possibility that children presenting with a traumatic epiphyseal fractures might have an underlying disorder. Additional research studies analyzing the relationship between upper tibia Salter-Harris fractures and hypovitaminosis D are necessary to infer any causative relationship, and to warrant the use of 25-hydroxyvitamin D level as a screening tool to predict risk of physeal fractures in African American children. The outcome of the patient reported here at 8-months follow- up was excellent, with no malunion or nonunion, no angular deformity, and no leg discrepancy.
References
- Potenza V, Caterini R, Maglione P, Bisicchia S, Farsetti P (2011) Simultaneous Bilateral Flexion-Type Salter-Harris II Fractures of the Proximal Tibia: A Case Report and Review of the Literature. Open Orthop J 5: 315-318.
- Ryan LM, Teach SJ, Singer SA, Wood R, Freishtat R, et al. (2012) Bone Mineral Density and Vitamin D Status Among African American Children With Forearm Fractures. Pediatrics 130(3): e553-e560.
- James J, Massey PA, Hollister AM, Greber EM (2013) Prevalence of Hypovitaminosis D among Children with Upper extremity fractures. J Pediatr Orthop 33(2): 159-162.
- Blanks RH, Lester DK, Shaw BA (1994) Flexion-type Salter II fracture of the proximal tibia. Proposed mechanism of injury and two case studies. Clin Orthop Relat Res (301): 256-259.
- Burkhart SS, Peterson HA (1979) Fractures of the proximal tibia epiphysis. J Bone Joint Surg Am 61(7): 996-1002.
- Peterson CA, Peterson HA (1972) Analysis of the incidence of injuries to the epiphyseal growth plate. J Trauma 12(4): 275-281.
- Mihran O, Tachdjian JAH (2002) Tachdjian's Pediatric Orthopedics from the Texas Scottish Rite Hospital for Children. 3rd edn. Elsevier, Philadelphia, USA.
- Poulsen TD, Skak SV, Jensen TT (1989) Epiphyseal fractures of the proximal tibia. Injury 20(2): 111-113.
- Salter RB, Harris WB (1963) Injuries Involving the Epiphyseal Plate. J Bone Joint Surg Am 45(3): 587-622.
- Vrettakos AN, Evaggelidis DC, Kyrkos MJ, Tsatsos AV, Nenopoulos A, et al. (2012) Lower limb deformity following proximal tibia physeal injury: long-term follow-up. J Orthop Traumatol 13(1): 7-11.
- Zionts LE (2002) Fractures around the knee in children. J Am Acad Orthop Surg 10(5): 345-355.
- Shelton WR, Canale ST (1979) Fractures of the tibia through the proximal tibia epiphyseal cartilage. J Bone Joint Surg Am 61(2): 167173.
- Inoue G, Kuboyama K, Shido T (1991) Avulsion fractures of the proximal tibia epiphysis. Br J Sp Med 25(1): 52-56.
- Mubarak SJ, Kim JR, Edmonds EW, Pring ME, Bastrom TP (2009) Classification of proximal tibia fractures in children. J Child Orthop 3(3): 191-197.
- Omar M, Petri M, Ettinger M, Decker S, Krettek C, et al. (2013) Simultaneous Bilateral Transitional Fractures of the Proximal Tibia after Minor Sports Trauma. Case Reports in Orthopedics 2013: 5.
- Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ (1994) Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop 14(4): 423-430.
- Donahue JP, Brennan JF, Barron OA (2003) Combined physeal/ apophyseal fracture of the proximal tibia with anterior angulation from an indirect force: report of 2 cases. Am J Orthop (Belle Mead NJ) 32(12): 604-607.
- Kraus R, Berthold LD, Heiss C, Lässig M (2009) Consecutive bilateral proximal tibia fractures after minor sports trauma. Eur J Pediatr Surg 19: 41-43.
- Wozasek GE, Moser KD, Hailer H, Capousek M (1991) Trauma involving the proximal tibia epiphysis. Arc Orthop Trauma Surg 110(6): 301-306.
- Skelley NW, Papp DF, Lee RJ, Sargent MC (2010) Slipped Capital Femoral Epiphysis with Severe Vitamin D Deficiency. Orthopedics 33(12): 921.
- Idelevich A, Kerschnitzki M, Shahar R, Monsonego Ornan E (2011) 1,25(OH)2D3 Alters Growth Plate Maturation and Bone Architecture in Young Rats with Normal Renal Function. PLoS ONE 6(6): e20772.
- Gordon CM, DePeter KC, Feldman HA, Grace E, Emans J (2004) Prevalence of Vitamin D Deficiency among Healthy Adolescents. Arch Pediatr Adolesc Med 158(6): 531-537.
- Harris SS (2006) Vitamin D and African Americans. J Nutr 136(4): 1126-1129.
- Talwar SA, Swedler J, Yeh J, Pollack S, Aloia JF (2007) Vitamin-D nutrition and bone mass in adolescent black girls. J Natl Med Assoc 99(6): 650-657.
- Williams R, Novick M, Lehman E (2014) Prevalence of Hypovitaminosis and its association with comorbidities of childhood obesity. Perm J 18(4): 32-39.
- Rhemrev SJ, Sleeboom C, Ekkelkamp S (2000) Epiphyseal fractures of the proximal tibia. Injury 31(3): 131-134.
- Ceroni D, Anderson de la Llana R, Martin X, Lamah L, De Coulon G, et al. (2012) Prevalence of vitamin D insufficiency in Swiss teenagers with appendicular fractures: a prospective study of 100 cases. J Child Orthop 6(6): 497-503.
- Thacher TD, Clarke BL (2011) Vitamin D insufficiency. Mayo Clin Proc 86(1): 50-60.
- Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, et al. (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 96(1): 53-58.
- Bonen DK, Schmid TM (1991) Elevated Extracellular Calcium Concentrations Induce Type X Collagen Synthesis in Chondrocyte Cultures. J Cell Biol 115(4): 1171-1178.
- Steele B, Serota A, Helfet DL, Peterson M, Lyman S, et al. (2008) Vitamin D deficiency: a common occurrence in both highand low-energy fractures. HSS J 4(2): 143-148.
- Sevenler D, Buckley MR, Kim G, van der Meulen MCH, Cohen I, et al. (2013) Spatial periodicity in growth plate shear mechanical properties is disrupted by vitamin D deficiency. J Biomech 46(10): 1597-1603.
- Williams JL, Do PT, Eick JD, Schmidt TL (2001) Tensile properties of the physis vary with anatomic location, thickness, strain rate and age. J Orthop Res 19(6): 1043-1048.
- Emanuel J, Rich M, Gilula LA (1989) Imaging rounds #97. Salter II fracture of the proximal tibia. Orthop Rev 18(1): 137-138, 141-143.
- Clement ND, Goswami A (2009) Salter-Harris II injury of the proximal tibia epiphysis with both vascular compromise and compartment syndrome: a case report. J Orthop Surg Res 4: 23.
- Krieg JC (2003) Proximal tibia fractures: current treatment, results, and problems. Injury 34 Suppl 1: A2-10.
- Herring JA (2002) Tachdjian's pediatric orthopaedics. (3ri edn) Saunders, Philadelphia, USA, pp. 2344-2351.
- Patari SK, Lee FY, Behrens FF (2001) Coronal split fracture of the proximal tibia epiphysis through a partially closed physis: a new fracture pattern. J Pediatric Orthop 21(4): 451-455.
- Poulsen TD, Skak SV, Jensen TT (1989) Epiphyseal fractures of the proximal tibia. Injury 20(2): 111-113.
- Robert M, Khouri N, Carlioz H, Alain JL (1987) Fractures of the proximal tibia metaphysis in children: review of a series of 25 cases. J Pediatr Orthop 7(4): 444-449.






























