Clinical Presentation of Medial Rotation and Anterior Tilt of the Scapula Following Traumatic Brachial Plexus Injury: Considering the Role of Serratus Anterior in Stabilization within the Posterior Shoulder Girdle and Kinetic Rehabilitation Techniques
William J Cobb*
Keele University, School of Medicine/ Health and Rehabilitation, UK
Submission: December 12, 2017; Published: January 16, 2018
*Corresponding author: William J Cobb, Keele University, School of Medicine/ Health and Rehabilitation, Staffordshire, UK, Email: kineticrehab@mail.com
How to cite this article: William J Cobb. Clinical Presentation of Medial Rotation and Anterior Tilt of the Scapula Following Traumatic Brachial Plexus Injury: Considering the Role of Serratus Anterior in Stabilization within the Posterior Shoulder Girdle and Kinetic Rehabilitation Techniques. Open Access J Surg. 2018; 7(3): 555715.DOI:10.19080/OAJS.2018.07.555715
Introduction
The importance of early detection and stabilization of the compromised shoulder girdle is an area that has been highlighted and investigated from an array of medical professional fields. Due to the shoulder girdle being the most mobile of all joints in the human body, it is considered as one of the most unstable [1] . Functional stability of the shoulder may vary dependent upon factors such as age, gender and indeed ethnicity [2]. The maintenance of the humeral head alignment within the glenoid fossa during shoulder motion has been shown to be absolutely pivotal for what is classically described as the "normal functional range of movement" to occur.
There are arrays of factors that can limit, reduce or stop functional ranges of movement within the joint. This can include physical injury to the anatomic area, neurological involvement or osteological change [3]. The purpose of this work is to look at the mechanics of the posterior shoulder girdle whilst considering the role of serratus anterior in stabilization within posterior shoulder girdle control, and in turn to consider how kinetic therapy can be implemented to stabilize unrefined movements. The following clinical case report was compiled during part of masters in neuro- musculoskeletal rehabilitation at Keele University School of Medicine/ Health and Rehabilitation.
The actual case study is taken from the author whilst working clinically with in an emergency department in Oxfordshire, United Kingdom. The clinical case study will be used as a discussion point for the consideration of Kinetic Control (KC) treatment strategies for patients with similar injures, whilst integrating current literature and clinical trials within shoulder girdle stabilization methodology.
Clinical Case Study
The initial patient contact came via an incident in which patient X was involved in a traffic incident which resulted in emergency department triage. Upon Immediate post-trauma clinical examination: it was noted that Patient X, A 35 year old male whom had presented following a fall from his motorbike during an incident involving another vehicle (Bike VS Car) showed right scapula medial rotation with anterior tilt. It was also noted that upon initial examination, that the patient had extremely limited flexion to the two and a half digits on the radial aspect of the hand with partial reduction in flexion to the digits on the ulnar aspect.
In addition to these initial findings, it was also found that the patient had sensory deficits to all of the digits of the right hand and around the region of the scapula. Chronologically, the patient was seen again 6 months later in the neuroscience pain team department. It had transpired that the patient whom presented to the emergency department 6 months earlier was referred to the neuroscience pain team due to ongoing movement and pain issues. Further clinical examination revealed that the patient reported complaints of shooting pains radiating up and down the upper and lower areas of the right arm.
It was also seen that the scapula was in acute medial rotation with the anterior tilt being prominent upon posterior shoulder girdle examination. There was also an asymmetry between the right and left spines of the scapula. This had become more prominent with the patient reporting increased sensory deficits and decreased functional range of movement during the 6 month period post trauma.
Osteology of the Shoulder Girdle
An understanding of the osteology of the scapula and the corresponding bony conjoins, is very important for the clinician as it allows one to consider the overlaying anatomical architecture in relation to specific bony landmarks. The Shoulder girdle, is often times referred to as the conjoint relationship of the scapula and clavicle whereas the Shoulder joint (glen humeral joint), is often referred to through the conjoint of the scapula and humours. The bones that make up the shoulder girdle include the, Scapula, Clavicle, Sternum and Humerus [4].

The important joints that make up the shoulder girdle include the, Rib cage joints, Glenohumeral (GH joint), Sternoclavicular (SC joint), Acromioclavicular (AC joint) and the Scapulothoracic joint. The Scapulothoracic Joint is not a joint in the pure sense of the word, as the scapula and thorax do not have a point of fixation (the scapula and thorax are not directly attached), but are connected indirectly by the clavicle and several muscles. However, the scapula does in fact move over the rib cage of the thorax, providing motion and flexibility [5-7].
The author's image bellow depicts the osteology of the scapula from the anterior and posterior viewpoint. The acromion along with the coracoid process are immediately identifiable via palpation and indeed can give great insight into the angle and relation of the glenoid fossa and humeral head alignment which is of great clinical significance when considering the processes of unrefined movement/s [3] (Figures 1-3).

Functionality and Joint Structure of the Shoulder Girdle
The Sternoclavicular (SC) Joint is formed from the union of the medial aspect of the clavicle with the sternum. The (SC) joint provides the only direct attachment of the upper extremity to the axial skeleton and is a Synovial joint-saddle joint with concave and convex surfaces on each of the joint's articular surfaces which functionally allows the clavicle to move in all three planes [5-7]. Most pertinent literature aggress that all movements of the shoulder girdle originate at the (SC) joint. This is very clinically important as a fused (SC) joint would significantly limit movement of the clavicle and scapula, and in turn the entire shoulder.
The normal functional ranges of the (SC) joint include: Elevation and Depression of the (SC) joint, Protraction and Retraction of the (SC) joint and Axial Rotation of the clavicle. The Sternoclavicular (SC) Joint Supporting Structures include the Sternoclavicular Ligament which connects the clavicle to the manubrium, the Inter-Clavicular Ligament, which Spans the jugular notch, connecting the superior medial aspects of the clavicles, the Costo-Clavicular Ligament which bounds the Clavicle to the costal cartilage of first rib. Protectively, the joint Capsule surrounds the entire (SC) joint with the Articular Disk acting as shock absorber between the clavicle and sternum [7].
The Acromioclavicular (AC) Joint is formed by the articulation of the acromion process of the scapula with the lateral end of the clavicle. The (AC) joint is a Synovial plane shaped joint which allows motion in all 3 planes: Upward and downward rotation, rotation in the horizontal plane and rotation in the sagittal plane. The motions of the (AC) joint allow the scapula to maintain firm contact with the posterior thorax. The supporting structures of the (AC) joint include the: Acromioclavicular Ligament which Joins the clavicle to the acromion and prevents dislocations of the scapula, the Coracoclavicular Ligament which connects the corocoid process of the scapula to the clavicle, the Coracoacromial Ligament which Connects the coracoid process to the acromion process and is in turn attached on both ends to the same bone thus creating a roof that protects the head of the humerus [5]. The Scapulothoracic Joint is formed by the junction between the anterior aspect of the scapula and the posterior thorax. The Movements are: Elevation and depression, Protraction and retraction, Upward and downward rotation and Scapular tilt [6-8].
Anatomy and Physiology of the Shoulder Girdle
The muscles of the shoulder and upper limb can be divided into four groups for ease of functional control and anatomical comprehension. The first group of muscles is responsible for the stabilization and position of the pectoral girdle. The second group of muscles is responsible for the movement of the arm. The third group of muscles is responsible for the movement of the forearm. The fourth and final group is responsible for the muscles that move the wrists, hands, and fingers. Anatomically, the pectoral girdle, (shoulder girdle), consists of the lateral ends of the clavicle and scapula, along with the proximal end of the humerus, and the muscles covering these three bones to stabilize the shoulder joint. Structurally and functionally speaking, the shoulder girdle creates a base from which the head of the humerus, in its ball-and-socket joint with the glenoid fossa of the scapula, can move the arm in multiple directions.
This relationship between the elements of the shoulder girdle is finely aligned and indeed require counteracting muscle tone in order to maintain stability. The important point within functional movement is the relationship of agonist and antagonist muscle groups and how opposition works ultimately to perform unity within function [4]. Although the topic of discussion is that of the posterior shoulder girdle, it is imperative that the muscles that position the Pectoral Girdle are considered as these are the counteracting force upon which range of motion is ultimately dictated. The Muscles that position the pectoral girdle are located either on the anterior thorax or on the posterior thorax.
The muscles that form the anterior group include the subclavius, pectoralis minor, and serratus anterior. The muscles that form the posterior group include the trapezius, rhomboid major, and rhomboid minor. When the rhomboids are contracted, the scapula moves medially, which can raise the shoulder and upper limb posteriorly. The three prime movers of the anterior thorax are the Subclavius, Pectoralis minor and Serratus anterior [4,8]. The first prime mover is the subclavius which originates at the First rib and inserts in the Inferior surface of clavicle. It is innervated by the subclavian nerve, which arises from the point of junction of the fifth and sixth cervical nerves (upper trunk of the brachial plexus).
The action is that of Stabilization of the clavicle during movement by depressing upon it [4,8]. The second prime mover is the Pectoralis minor which originates at the anterior surfaces of certain ribs (2-4 or 3-5) and inserts at the Coracoid process of scapula. It is innervated by the medial and lateral pectoral nerves (C6-Th1), branches of the brachial plexus. The action is that of Rotation of the shoulder anteriorly (throwing motion) and assistance with inhalation [4,8]. The third prime mover is the Serratus anterior which originates at the muscle slips from certain ribs (1-8 or 1-9) and inserts at the anterior surface of vertebral border of scapula.
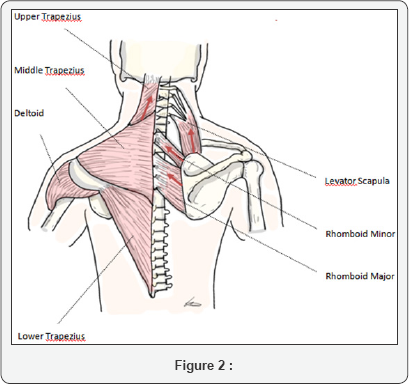
It is innervated by the long thoracic nerve (Nerve of Bell) as seen and discussed clinically in (Bells palsy). The long thoracic nerve, which is a branch of the brachial plexus travels inferiorly on the surface of the serratus muscle and acts, is the movement of the arm from the side of body to the front of the body whilst also assisting with inhalation [4,8]. The three prime movers of the posterior thorax are that of the Trapezius, Rhomboid major and Rhomboid minor. The first prime mover is the trapezius, which originates at the Skull; Vertebral Column and inserts at the Acromion and Spine of Scapula; Clavicle. It is innervated by the accessory nerve.
Sensation, including pain and the sense of joint position (proprioception), travel via the ventral rami of the third (C3) and fourth (C4) cervical nerves. Its action is that of elevation of the shoulders (shrugging); pulling of the shoulder blades together and tilting of the head backwards [4,8]. The second prime mover is the rhomboid major which originates at the thoracic vertebrae (T2-T5) and inserts at the medial border of scapula. It is innervated, as is the rhomboid minor, by the ventral primary ramus via the dorsal scapular nerve (C5). Its action is that of scapula stabilization during pectoral girdle movement [4,8].
The third prime mover is the rhomboid minor which originates at the cervical and thoracic vertebrae (C7 and T1) and inserts at the medial border of the scapula. It is innervated by the ventral primary ramus via the dorsal scapular nerve (C5). Its action is that of scapula stabilization during pectoral girdle movement [4,8].
Clinical Correlate
When considering the anatomical architecture of the shoulder girdle, the clinician can consider normal and abnormal relationships of certain important joints via bony landmark palpation. Upon clinical examination of the scapula, the symmetry between that of the left and right spine of scapula should be noted for interpretation of the uncontrolled movement [9]. Asymmetry within the region may be due to things like poor posture resulting in over or under use of the counteracting flexor or extensor groups, Other factors that may affect the girdle may be down to neuronal issues or other underlying pathologies such as carcinoma, which may manifest in displacement of the structure caused by muscle grouping dysfunction or neuronal control [9,10].
Clinical Examination of the Scapulas
When examining the scapula from the posterior aspect on the patient, the spine should be able to be palpated from the medial border making a slight incline to the acromion that should in normal posture be superior and anterior in relation to the breadth of the spine [10]. The direction stability and support of the scapula in relation to serratus anterior is most important in clinical exam, as this ultimately will define structural and neuronal integrity of the shoulder girdle as a whole. Serratus anterior has three insertion areas on the scapula, serratus anterior-superior, serratus anterior-intermediate and serratus anterior-inferior.
The serratus anterior-superior is inserted near the superior angle of the scapula. The serratus anterior-intermediate is inserted along the medial border of the scapula and the serratus anterior-inferior is inserted near the inferior angle of the scapula [4,8,11]. The scapula is pulled forward around the thorax for ante version of the arm by the three parts of serratus. The inferior and superior parts act together to keep the scapula pressed against the thorax with assistance of the rhomboids. The inferior part of serratus can pull the lower end of the scapula laterally and forward and thus rotates the scapula to make elevation of the arm possible. All three parts also assist in respiration when the shoulder is fixed [4,8,11].
Clinical Research
Maikutlo et al. [12] looked at the effect of thoracic posture on scapular movement patterns, active range of motion (ROM) in scapular plane abduction, and isometric scapular plane abduction muscle force. The Study Design and Method was a repeated measures design in which 34 healthy subjects (mean age, 30.2yrs). Were positioned and stabilized while sitting in both erect and slouched trunk postures. A three-dimensional electromechanical digitizer was used to measure thoracic flexion and scapular position and orientation in three planes.
Measurements were taken with the arm (1) at the side,(2) abducted to horizontal in the scapular plane, and (3) at maximum scapular plane abduction. In each posture, isometric abduction muscle force was measured with the arm at the side and abducted to horizontal in the scapular plane. Results showed that in the slouched posture, the scapula was significantly more elevated in the interval between 0 to 90° abduction. In the interval between 90° and maximum abduction, the slouched posture resulted in significantly less scapular posterior tilting. There was significantly less active shoulder abduction ROM in the slouched posture (mean difference = 23.6° ± 10.7°).
Muscle force was not different between slouched and erect postures with the arm at the side, but with the arm horizontal, muscle force was decreased 16.2% in the slouched position. The Conclusion from the research suggested that the Thoracic Spine position significantly affects scapular kinematics during scapular plane abduction, and that the slouched posture is associated with decreased muscle force.
The Role of Serratus Anterior in Scapula Attachment within the Shoulder Girdle from the Posterior Aspect in Relation to the Primary Stabilizers of the Scapula
As can be seen in the authors diagram bellow, the scapula has three primary midline support structures, namely the levator Scapula, Rhomboid Minor and the Rhomboid Major. Damage to any one of these three important anatomical structures, will result in an over-action/over-tension on the remaining muscle/s. The result of neuronal or physical damage to any one or group of supporting muscles will clinically manifest in an abnormal posture/movement pattern ultimately altering form and range of movement [7-9].
The clinician with a good comprehension of the supporting structures of the shoulder girdle should be able to deduce the ill functioning group or groups and in turn test for appropriate functional movement patterns using the principles of Kinetic Testing (KC). The degree to which the patient can or indeed cannot perform chosen movement tasks provides the clinician with the appropriate information to consider specific muscle targeting strategies. The role of serratus anterior differs from the aforementioned muscles, as it essentially pins the scapula to the posterior lateral thoracic wall whilst emanating its muscle fiber projections anterior-laterally. Serratus is in essence the counteraction upon the primary scapula stabilizers.
The levator Scapulae originates from the posterior tubercle of the transverse process of the cervical vertebrae one to four and inserts into the medial border of the scapula thus extending from the superior angle to the junction of the spine and medial border of the scapula. Anatomically, the levator scapulae can lie deep to the sternocleid omastoideus at its origin, deep or adjacent to the splenius capitis at its origin and mid-portion, and deep to the trapezius in its lower portion [13].
The Actions of the levator scapulae when the spine is fixed, is that of a levator of the scapulae, elevating the scapula and rotating its inferior angle medially. The levator scapulae often work in combination with other muscles like the Rhomboids and Pectoralis minor to rotate down [13]. Elevation or rotation of one shoulder at a time requires muscles to stabilize the cervical spine and keep it immobile and thus prevents flexing or rotating. Elevating both shoulders at once with equal amounts of pull on both side of the cervical spinal origins, counteracts these forces exerted by the stabilizing muscle groups. When both shoulders are elevated at once, downward rotation is prevented by the cocontraction of other muscles that elevate the spine such as the upper fibers of the trapezius, which is an upward rotator [13-15].
When the shoulder is in a fixed position, the levator scapula rotates to the same side and flexes the cervical spine laterally. However, when both shoulders are fixed, a simultaneous cocontraction of both levator scapulae muscles in equal amounts does not produce lateral flexion or rotation, and may produce straight flexion or extension of the cervical spine [13-15]. A levator scapula is supplied by two or three branches of the fourth and fifth cervical nerves, and frequently by a branch from the dorsal scapular nerve [4].
The rhomboid minor arises from the inferior border of the nuchal ligament, from the spinous processes of the seventh cervical and first thoracic vertebrae, and from the intervening supraspinous ligaments. It is inserted into a small area of the medial border of the scapula at the level of the scapular spine. Its Actions together with the rhomboid major, the rhomboid minor is that of retraction of the scapula when the trapezius is contracted [16,17]. The rhomboid major and minor act as an antagonist to the trapezius. The rhomboid major and minors action upon the scapula is that they elevate the medial border of the scapula medially and upward, working in tandem with the levator scapulae muscle to rotate the scapulae downward.
Whilst other shoulder muscles are active, the rhomboid major and minor stabilize the scapula. This is an important clinical point, as destabilization of the scapula in functional muscle group testing may indicate that these important stabilizers are unrefined or not functioning normally [17-19]. The Innervations comes from the dorsal scapular nerve, with most of its fibers derived from the C5 nerve root and only minor contribution from C4 or C6 [4]. The rhomboid major arises from the spinous processes of the thoracic vertebrae T2 to T5 as well as the supraspinous ligament. It inserts on the medial border of the scapula, from about the level of the scapular spine to the scapula's inferior angle.
The rhomboid major is considered a superficial back muscle. It is deep to the trapezius, and is located directly inferior to the rhomboid minor. As the word rhomboid suggests, the rhomboid major is diamond-shaped. The major in its name indicates that it is the larger of the two rhomboids [4].
The Role of Serratus Anterior in Scapula Attachment within the Shoulder Girdle
As can be seen in the authors diagram bellow, the role of serratus anterior in anterior-lateral stabilization and angular arrangement is pivotal. The serratus acts somewhat like an elastic band pinning the inferior border of the scapula to the thoracic cage. More precisely, the serratus anterior envelopes the lateral border of the thoracic cage which is clinically very significant as the serratus anterior bounds the posterior aspect of the scapula to form an envelope bounding the scapula to the thoracic girdle at the lateral point of the mid axillary line thus stopping the posterior tug of the levator scapula, rhomboid major and rhomboid minor.
Without the action of the serratus, the shoulder girdle would be grossly displaced with the counteracting posterior muscle groups heaving the shoulder girdle into a posterior displacement or classically manifesting in the Bells dysfunction movement pattern [18-20]. As with many upper extremity injuries in the region of the brachial plexus, the movement pattern/ unrefined movement pattern, will ultimately paint a detailed image of the underlying neuronal involvement. The clinician involved in strategizing movement rehabilitation must ensure that a detailed analysis of the various potential functional or nonfunctional muscle group/s has been adequately considered.
The greater the consideration of specific motor and or sensory deficits will ultimately dictate the corrective Kinetic Control strategies. For example, the "Motor" impairment of the "Long Thoracic Nerve", will ultimately show movement patters pertaining to the Bell pattern, this may or may not include sensory deficits which will in turn give specificities of the nature / mechanism of the injury "Motor or Sensory or Mixed" [18-20].
Relating the Clinical Significance of the Case Study to General Kinetic Evaluation and Treatment
The clinician examining and managing the patient with neuro-musculoskeletal injuries must be aware of the mechanisms of injuries and how in turn this will clinically manifest upon examination. The greater the structural and functional understanding of human movement, the greater the chance of diagnostic and implementive strategy planning from a Kinetic Control standpoint [9,10]. The anatomic and physiologic comprehension of movement patterns will undoubtedly inform the clinician of how and what structural functional changes may or indeed may not be expected in patients with neuro- musculoskeletal issues and in turn allow for appropriate therapy planning. The importance of cause and effect are prominent when considering the aforementioned clinical case study.
The motor and indeed latter sensory deficits shown in the limited flexion to the two and a half digits on the radial aspect of the hand with the addition of partial reduction in flexion to the digits on the ulnar aspect shows radial and ulnar nerve involvement. The displacement of the scapula and the acute tilt refers to the involvement of the long thoracic nerve (Nerve of Bell). It is of no real surprise due to the close anatomical configuration of the brachial plexus that such an array of symptoms are formed in such mechanisms of injury. From an anatomic and physiologic perspective, the clinician using Kinetic Control methodologies must have an excellent comprehension of agonistic and antagonistic muscle groups and how in turn they act upon each other. For example, where flexors are grossly overactive for prolonged periods, the extensor group will become elongated and less physiologically active. If left for long periods of time, prolonged over-action of an agonist flexor or extensor group will not only effect the opposing muscle, but may eventually alter the underlying osteological architecture thus making Kinetic Movement rehabilitation much less likely to have pronounced effect.
Once underlying osteological architecture is compromised, the rehabilitative potentials from a Kinetic standpoint become less effective. The important point to address in Kinetic therapy is the early detection and implementation of movement retraining and rehabilitation strategies [9,10]. The clinical case study as mentioned in this paper looks at a 6 month period of movement dysfunction. Ideally, Patient X would have received early interventional movement therapy in order to attempt to address the muscle/s de-innervations. Early intervention would not only allow a greater understanding of the patient's functional deficits and needs but also would allow the reduction of osteological architectural degeneration.
Although patient X is a younger male, the risk factor increases greatly with the progression of age as seen in the hypnotic and lordotic postures as seen with progressing age. In summation, the implementation of Kinetic Control Therapy must be done in a timely and concise manner considering the best movement re-training strategies built upon an excellent anatomical and physiological understanding of the afflicted area. Progression of abnormal movement patterns will ultimately alter osteological architecture if left unmanaged thereby making effective Kinetic Therapy less likely. This being said, it is not unreasonable to address such problems with an array of integrative medical treatments that may or may not include osteological manipulations which could be used alongside kinetic rehabilitation strategies.
References
- Hyde TE, Gengenbach MS (2007) Conservative Management of Sports Injuries. Jones and Bartlett Publishing, Canada.
- Williams GR, Ramsey ML, Wiesel BB (2015) Operative Techniques in Shoulder and Elbow Surgery. Lippincott Williams and Wilkins, USA, pp. 461.
- Paul Tornetta (2015) Operative Techniques in Orthopaedic Trauma Surgery. Lippincott Williams and Wilkins, USA.
- Hamill J, Kathleen M (2003) Knutzen Biomechanical Basis of Human Movement. Lippincott Williams and Wilkins, USA.
- Rockwood CA (2009) The Shoulder. Fourth Edition, Saunders Elsevier, USA.
- Whiting WC, Zernicke RF (2008) Biomechanics of Musculoskeletal Injury. Library of Congress Publishing, USA.
- Snell R (1995) Clinical Anatomy for Medical Students (5th edn), River woods IL. Lippincott Williams and Wilkins, USA.
- Ellis H, Mahadevan V (2010) Clinical Anatomy: Applied anatomy for students and junior doctors. (13th edn), Wiley Blackwell, UK, pp. 500.
- Comer ford M, Mottram S (2012) Kinetic Control: The Management of Uncontrolled Movement. Churchill Livingstone, UK.
- Winter DA (2009) Biomechanics and Motor Control of Human Movement. John Wiley & Sons, Canada.
- Moses KP, Banks JC, Nava PB, Peterson D (2005) Atlas of Clinical Gross Anatomy. Elsevier Mosby, USA.
- Kebaetse M, McClure P, Pratt NA (1999) Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil 80(8): 945-950.
- Susanne Klein Vogelbach (1990) Functional Kinetics: Observing, Analyzing, and Teaching Human Movement. Springer Publishing, Berlin, Europe.
- Behnke Robert S (2012) Kinetic Anatomy 3rd Edition. Library of Congress Publishing, USA.
- Andrea Fusco, Andrea Foglia, Frank Musarra (2008) The Shoulder in Sport: Management, Rehabilitation and Prevention. Churchill Livingstone, Canada.
- Simons DG, Travell JG, Lois S. Simons (1999) Travell & Simons Myofascial Pain and Dysfunction: Upper half of body. Williams and Willkins Publishing, USA.
- Tubbs RS, Shoja MM, Loukas M (2016) Bergman's Comprehensive Encyclopedia of Human Anatomic Variation. Library of Congress Publishing, USA.
- Kibler WB, Sciascia AD (2017) Disorders of the Scapula and Their Role in Shoulder Injury: A Clinical Guide to Evaluation and Management. Springer Publishing, USA.
- Frontera WR, Silver JK, Rizzo TD (2015) Essentials of Physical Medicine and Rehabilitation. Elsevier Saunders, USA.
- Skirven TM, Osterman AL, Fedorczyk J, Amadio PC (2011) Rehabilitation of the Hand and Upper Extremity. Elsevier Mosby, USA.






























