Ileosigmoid Knotting, Rare Cause of Intestinal Obstruction and Gangrene
Jowhara Al-Qahtani, Ahmed Faidah, Mohammed Yousif, Mohamed A Kurer, Syed Muhammad Ali*
Department of Surgery, Hamad Medical Corporation, Qatar
Submission: November 22, 2017; Published: December 15, 2017
*Corresponding author: Dr Syed Muhammad Ali, Department of Surgery, Hamad Medical Corporation, P O Box 3050, Doha, Qatar, Email: ali_2051@hotmail.com,SAli35@hamad.qa
How to cite this article: Jowhara Al-Qahtani, Ahmed Faidah, Mohammed Yousif, Mohamed A Kurer, Syed Muhammad Ali, Ileosigmoid Knotting, Rare Cause of Intestinal Obstruction and Gangrene. Open Access J Surg. 2017; 7(3): 555712. DOI: 10.19080/OAJS.2017.07.555712.
Abstract
Ileo-sigmoid knotting is a rare life threatening condition which presents as, and causes, bowel obstruction. It is defined as wrapping of the ileum around the sigmoid colon. It is difficult to diagnose preoperatively due to its rarity. It has high mortality; hence, immediate surgical intervention is a mandatory. We describe here a young man who presented with sudden onset abdominal pain and distention. Patient's workup showed elevated white cell count and lactic acid. CT (Computerized Tomography) scan showed bowel ischemia. Upon surgical exploration patient had ileo-sigmoid knotting (ISK). Gangrenous bowel was resected and primary anastomosis was done.
Keywords: Ileo-sigmoid knotting; Intestinal obstruction
Introduction
Ileosigmoid knotting (ISK) is a double loop intestinal obstruction, combination of ileal and sigmoid volvulus. It is a rare condition mostly found in African patients. It was populated by Shephered in [1]. Most common presentation is acute abdominal pain, distension and tenderness; other symptoms include nausea, vomiting, and partial or absolute constipation. Patients could present with sepsis and peritonitis. The most important signs are diffuse abdominal distention and tenderness. It is difficult to diagnose clinically and radio logically. Differential diagnosis could include sigmoid volvulus and it is of extreme importance to rule this diagnosis out as endoscopic reduction is contraindicated in ISK [2].
Case
A 32-year-old, previously healthy, Tanzanian male presented to the emergency department of Hamad General Hospital in Qatar with generalized colicky abdominal pain, vomiting and absolute constipation for one day. He denied any previous abdominal surgeries. On examination, he was alert, oriented and not in distress. His vitals were within normal range. His abdomen was distended with generalized tenderness and mild guarding. No masses were felt and his bowel sounds were normal. Digital rectal examination was normal. His Labs showed white cell count of 21.8 x103/uL, and Lactic Acid of 7.9 m mol/L, and normal renal functions. Patient was given intravenous fluids and antibiotics, nasogastric tube was inserted. CT scan abdomen revealed mal-rotation with mid gut volvulus with whirlpool appearance of superior mesenteric vessels in mesentery, with a picture suggestive of sigmoid volvulus. The patient was taken to operating theatre for an exploratory laparotomy (Figure 1 & 2).
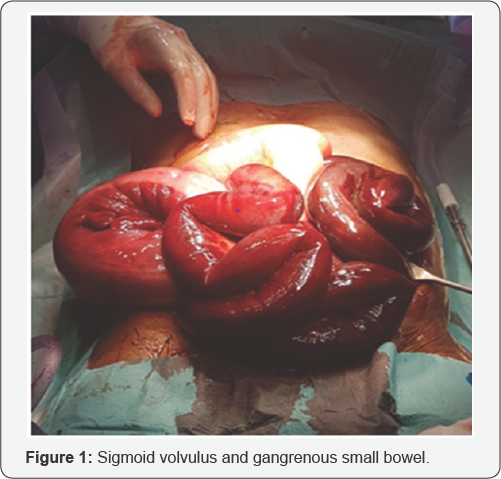

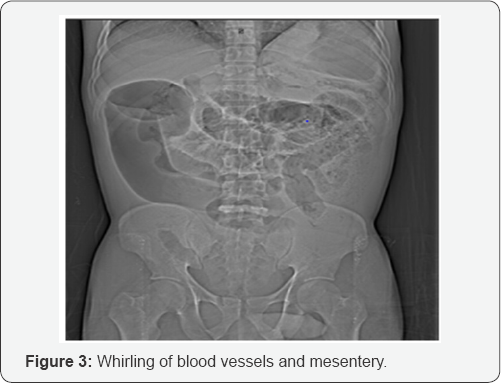

Upon opening the abdomen, hemorrhagic fluid was aspirated. We found gangrenous small bowel and sigmoid interloped together (Figure 3 & 4). Patient had redundant and narrow mesentery of the small bowel knotting itself firmly around the redundant and ischemic sigmoid colon. Several attempts to undo the knot were unsuccessful. Therefore, we elected to resect the already ischemic sigmoid colon. This unraveled the twisted small bowel mesentery revealing the full extent of the gangrenous small bowel. 230 cm of small bowel was resected along with the sigmoid colon. The remaining proximal small bowel was measured to be 200 cm. As the patient was acidotic (7.24) and hypothermic (35.6 C) damage control surgery was done and abdomen was left open.
The patient was transferred to the surgical intensive care unit where he was kept intubated and was stabilized. He had a significant clinical improvement with a return of his laboratory parameters to near normal levels over 24 hours. Therefore, patient was taken into the operating theatre for primary anastomosis and closure of the abdominal cavity. The remnant small bowel was anastomosed to the caecum side to side and the remaining two ends of the sigmoid were sufficiently redundant to allow side-to-side anastomosis. Thorough warm saline washout and abdominal closure was done.
The patient was transferred back to the SICU and was extubated the following day. Patient had uneventful stay in the ICU and oral feeding was commenced on day 3 which he tolerated well. The abdominal drain was removed on day 4. On day 6 the patient was discharged. He was seen in the outpatients' clinic two weeks after his discharge from the hospital. He was asymptomatic and his laparotomy incision has healed completely. Histopathology revealed bowel ischemia.
Discussion
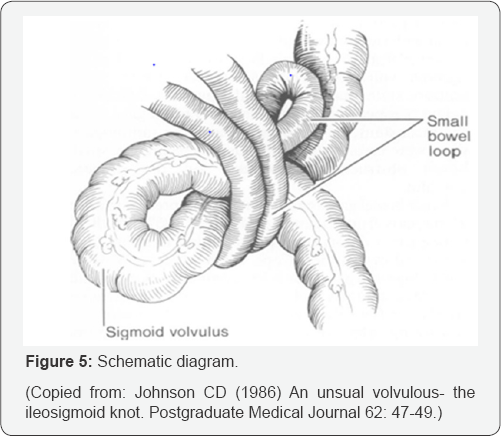
Ileosigmoid knotting (IKS) was first described in 1845 By Parker [2]. It is considered as compound volvulus where the ileum mesentery wraps around the sigmoid colon as shown in Figure 5. It is a rare disease and causes intestinal obstruction [2]. The incidence of IKS is not well established however, it generally occurs in areas with high incidence of sigmoid volvulus [1]. It is common in Turkey especially in Eastern Anatolia, in Asia, and in African population where the current patient is from. Literature search showed more than 280 reported cases. It is common in male (80 %) in their fourth decade [3], in the late pregnancy period in females, and among Muslims who eat a single daily meal during Ramadan, fasting month [1]. The main etiology is unknown, however; three factors are found to responsible for IKS: long small bowel mesentery, free and mobile small bowel, and a redundant sigmoid colon with narrow pedicle.
In addition, high bulk diet in the presence of an empty small bowel [2] predisposes patients to ISK that what may explain the higher incidence in Muslims in Ramadan. As the bulk diet moves down the proximal jejunum it increases the small bowel peristalsis, causing the heavier parts of jejunum to fall to left lower quadrant, while the empty long parts of Jejunum and Ileum twists around the narrowed based redundant sigmoid [4]. Other secondary causes are previous surgery causing adhesions, late pregnancy, trans-mesenteric herniation, Meckel diverticulum with a band, ileocecal intussusceptions, and floating cecum [2].
The first classification of ISK was described by Alver [5] who classified IKS into 4 types based on the active and passive component (ileum vs sigmoid). Those types were further subcategorized into A and B in based on the direction of torsion (clockwise and anticlockwise respectively). The torsion is also subcategorized to degree of torsion 180, 270, 360, 360 x 2. In type I, the ileum is actively wrapped around the sigmoid. In type II, the redundant sigmoid colon is wrapped around the ileum. In type III, the ileocecal segment is wrapped around the sigmoid [5]. The fourth type which is indeterminate is when the active segment couldn't be identified [1]. The most common type is type I and type A (clockwise) which our patient had.
It is difficult to diagnose IKS preoperatively. Diagnostic modality of choice is CT scan which will show dilated sigmoid shadow and multiple air fluid levels in the small intestine [2]. Also another CT feature is whirl sign created by the twisted intestine and sigmoid mesocolon in ileosigmoid knot, medial deviation of the cecum, and descending colon, and radial distribution of the intestine and mesenteric vasculature [6,7]. CT scan is not always used to establish the diagnosis as most patients are critically ill and rushed to operating rooms.
A triad has been proposed and includes 1- clinical picture of small bowel obstruction, 2- radiographic evidence of predominately large bowel obstruction, and 3- inability to insert a sigmoidoscope. Initial management includes adequate resuscitation, electrolytes replacement, and antibiotics covering gram negative microbes [2]. However, this shouldn't delay exploration of the patient. IKS compromises the blood supply to bowel and causing gangrene of small or large bowel and perforation. More than 75 % of IKS cases, the bowels was gangrenous, and up to 60 % the small bowel and sigmoid were affected [4].
The surgical choice of treatment is based on two factors the condition of the patient and most importantly bowel viability [8]. The objective of surgical treatment is release the knot, resect the gangrenous bowel segment, restore intestinal continuity, and prevent recurrence [8]. Atamanalp proposed a new Classification of ISK that will contribute to the treatment and prognosis of ISK. The classification consist of 6 classes and is based on age whether above or below 60 years, associated diseases, presence of shock and presence of bowel gangrene. Classification showed that the higher the class (C6- patients with gangrene in both segments), the higher the mortality, and increases the chance of creating stoma [8].
When bowel is gangrenous one can't untwist the knot as it is in risk of rupture and spillage of its toxic content, hence resection is required [9]. If the patient is stable, primary anastomosis can be considered, but if the patient is unstable then damage control resection of bowel or stoma creation is indicated. Detrosion of bowel can be done in selected patients with viable bowel, with a definitive procedure to prevent recurrence for example sigmoidpexy or sigmoid resection [8]. In this case the patient’s abdomen was left open for 24hrs as patient physiological parameters didn't allow for immediate primary anastomosis.
IKS has poor prognosis high mortality up to 48 % [2] and can reach to 100 %. The cause of death is shock and multiorgan failure [10]. Factors causing this high mortality are shock, peritonitis, presence of gangrenous bowel, age, and co morbidities [1]. Mortality is high when there is bowel gangrene 25.9 % [1] and higher with double segments gangrene (ileum and sigmoid) [5,8].
Conclusion
IKS is a rare disease causing double close loop bowel obstruction. It is most commonly found in areas with high rate of sigmoid volvulus. IKS mostly presents as abdominal pain and distention. It is a surgical emergency and has high mortality. Main surgical treatment is resection of gangrenous bowel and restoration of intestinal continuity either at initial operation or in second look surgery.
References
- Atamanalp SS, Oren D, Bajoglu M, Yildirgan MI, Balik AA, et al. (2004) Ileosigmoid knotting: outcome in 63 patients. Dis Colon Rectum 47(6): 906-910.
- Machado NO (2009) Ileosigmoid knotting: a case report and literature review of 280 cases. Ann Saudi Med 29(5): 402-406.
- Shepherd JJ (1967) Ninety-two cases of ileosigmoid knotting in Uganda. Br J Surg 54(6): 561-566.
- Ooko PB, Saruni S, Oloo M, Topazian HM, White R (2016) Ileo-Sigmoid Knotting: A review of 61 cases in Kenya. Pan Afr Med J 23: 198.
- Alver O, Oren D, Tireli M, Kayabaji B, Akdemir D (1993) Ileosigmoid knotting in Turkey. Review of 68 cases. Dis Colon Rectum 36(12): 1139-1147.
- Baheti AD, Patel D, Hira P, Babu D (2011) Ileosigmid knot: a case report. Indian J Radiol Imaging 21(2): 147-149.
- Lee SH, Park YH, Won YS (2000) The ileosigmoid knot: CT findings. AJR Am J Roentgenol 174(3): 685-687.
- Atamnalp SS, Ozturki G, Aydinli B, Yildirgan I, Basoglu M, Et al. (2009) A New Classification for Ileosigmoid Knotting. Turk J Med Sci 39(4): 541-545.
- Mallick IH, Winslet MC (2004) Ileosigmoid knotting. Colorectal Dis 6(4): 220-225.
- Adili W, Mutua JM, Nanabhai BM (2014) The ileosigmoid knot: A case report. The annals of African surgery. 11(2): 44-46.






























