Case Report: Non-Traumatic Diaphragmatic Hernia in Adult
Sushila Ladumor1*and Adham Darweesh2
1Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, Doha, Qatar, Assistant Professor in Clinical Radiology, Weil Cornel Medical College, Qatar (WCMC-Q)
2Senior Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH,Doha, Qatar, Assistant Professor in Clinical Radiology, Weil Cornel Medical College, Qatar (WCMC-Q)
Submission: September 23, 2017; Published: October 02, 2017
*Corresponding author: Sushila Ladumor B, Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, Doha, Qatar, Assistant Professor in Clinical Radiology, Weil Cornel Medical College, Doha, Qatar (WCMC-Q), Email: drsbladumor@yhaoo.com
How to cite this article: Sushila L, Adham D. Case Report: Non-Traumatic Diaphragmatic Hernia in Adult. Open Access J Surg. 2017; 6(2): 555682. DOI: 10.19080/OAJS.2017.06.555682
Abstract
Congenital diaphragmatic hernia is a major malformation occasionally found in newborns and babies. Congenital diaphragmatic hernia is defined by the presence of an orifice/defect in the diaphragm, more often to the left and posterolateral that allows herniation of abdominal contents into the thorax. Diaphragmatic hernias are common, and many times incidental, proper diagnosis of both benign and life-threatening manifestations of diaphragmatic hernias is very important to guide appropriate treatment and management. Congenital fetal diaphragmatic hernias, traumatic diaphragmatic rupture, and large symptomatic Bochdalek, Morgagni, and hiatal hernias are typically repaired surgically, while eventration, diaphragmatic slips, and small diaphragmatic hernias do not require intervention or imaging follow-up but should be properly diagnosed to avoid confusion with other diagnoses that require additional attention presenting here unusual case of adult left diaphragmatic hernia with no history of trauma and no previous exam.
Keywords: Right-sided diaphragmatic hernia; Adult; Computed Tomography; MRI; Diaphragmatic defect; Plain X-ray films; Surgery
Clinical History
32 year old male with no chronic medical illness presented to Emergency Department with 3 day history of progressive epigastric pain, colicky, non-radiating and severe in nature, no relieving or exacerbating factors associated with vomiting and constipation of 4 days, not passing flatus for 4 days. He denies any cough, shortness of breath or chest pain. He denies any snoring at night, daytime sleepiness. He denies any family history of diaphragmatic hernia, trauma in the past. No history of smoking or Alcohol use. He had similar symptoms before four month that resolved spontaneously, at that time he was diagnosed with diaphragmatic hernia, suspected from frontal erect X-ray of chest and abdomen and evident on CT chest done at that time. Patient advised surgery at the time of first presentation, but patient refused for surgery and discharged against medical advice.
X-ray Chest and Abdomen erect projection recommended at time of first presentation
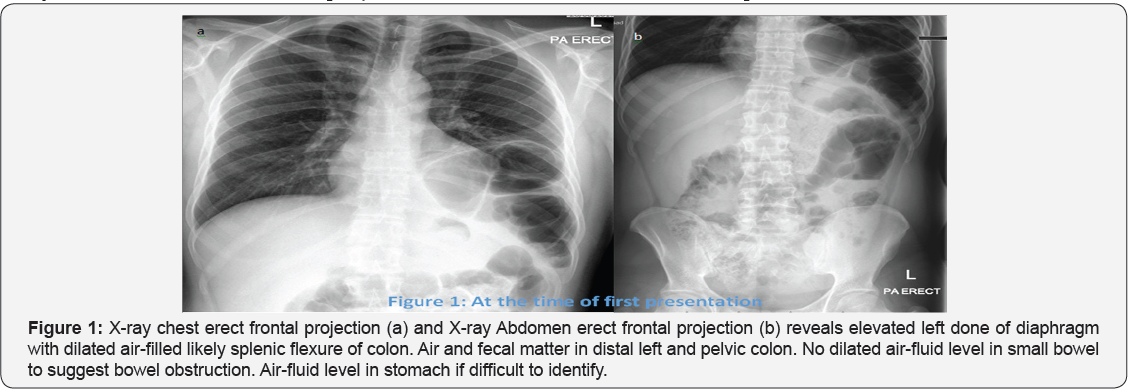
Impression of Figure 1: Above described findings representing differential diagnosis of left diaphragmatic eventration or left diaphragmatic hernia.
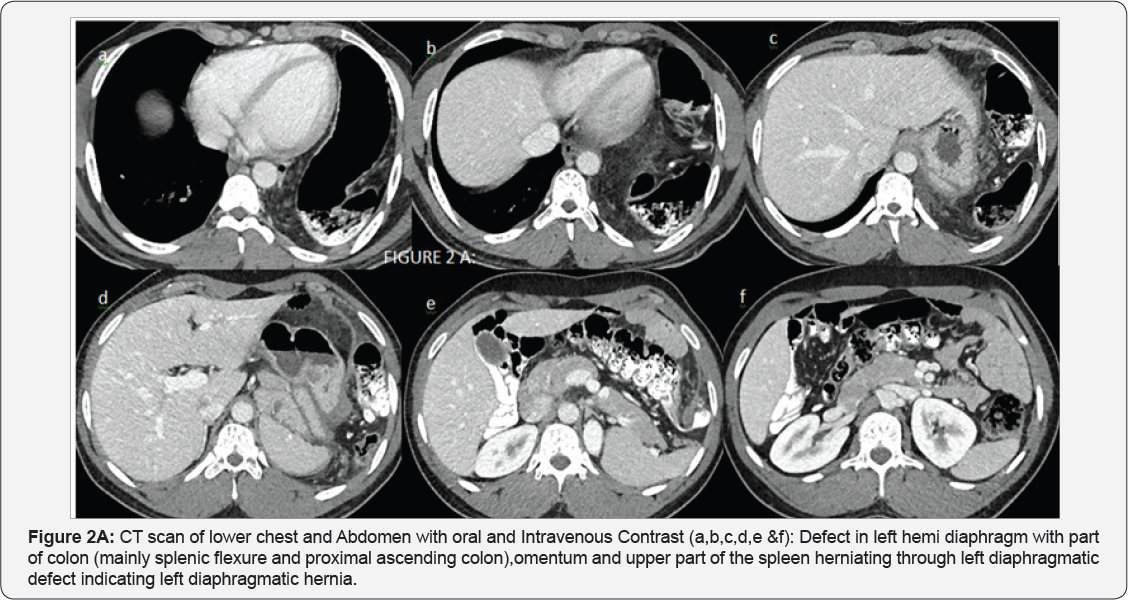
CT SCAN with Oral and IV contrast recommended for further work-up and characterization at time of first presentation after X-ray:
Impression of Figure 2A & 2B: Left diaphragmatic hernia containingpart of colon (mainly splenic flexure and proximal ascending colon),omentumand upper part of the spleen. No signs of acute bowel obstruction. No ascites. No free air.
Surgery was done after second presentation as patient refused surgery and went home against medical advice.
Surgeons Note: Indication for Surgery known left diaphragmatic hernia. Preoperative Diagnosis: Left diaphragmatic hernia with laparoscopic reduction and repair


A. Findings at surgery: About 5 cm hernia defect at the posterolateral left diaphragmatic dome that is containing part of the omentum and the lower pole of the spleen and the splenic flexure of the colon.Repair was done and organs reduced (Figure 3).
B. Follow-up X-ray chest after one month of surgery.
Discussion
Congenital diaphragmatic hernia (CDH) is an idiopathic human malformation that usually presents in the newborn period. Diaphragmatic hernia in the absence of trauma is very rare in adults. The literature describes less than a dozen such cases of right-sided diaphragmatic hernia. The hernial contents were the stomach, spleen, pancreas, large bowel, small bowel, omentum and rarely kidney and part of pancreas all structures have only been documented in left-sided diaphragmatic hernias. Diaphragmatic hernias are defined as either congenital or acquired defects in the diaphragm.
Demographics and etiology
a. Congenital
There are two main types of congenital diaphragmatic hernia (CDH)s which are uncommon yet distinct entities that usually occur on the left side (80%) of the diaphragm [1-4]:
Traumatic diaphragmatic rupture through either penetrating injury (65%) or blunt trauma (35%) (3)
a) Hiatus hernia
b) Iatrogenic
Depending on the location and size of the defect retroperitoneal or intra-abdominal organs and tissues can prolapse into thoracic cavity due to the negative intra-thoracic pressure 1.
Anatomy of Diaphragm
The diaphragm has a central tendon and a peripheral muscular component. The central tendon arises from the septum transversum, while the muscular component arises from the pleuroperitoneal membrane. Anteriorly, the diaphragm attaches to the posterior margins of the lower sternum and xiphoid process. The lateral or costal parts attach to the inner margins of the 6th through 12th ribs. Posteriorly, the lumbar part attaches to the medial and lateral arcuate ligaments. The right crus is attached to the first, second, and third lumbar vertebrae, while the left crus is attached to the first and second lumbar vertebrae. The fibrous margin of the right and left crura forms the median arcuate ligament.
Diaphragmatic Defects
Congenital diaphragmatic hernia (CDH) is a well described condition that occurs in about 1 in 5000 live births. The condition is usually sporadic, though association with various genetic syndromes has been reported. CDH consists of herniation of bowel, and occasionally solid organs, into the chest, usually through the Foramen of Bochdalek, a potential weak spot in the posterolateral diaphragm. 80% of CDH occur on the left side, as the liver provides a relative barrier on the right. A number of cases have now been diagnosed in utero using screening ultrasound, but infants typically present shortly after birth with respiratory distress. The major clinical problem is pulmonary hypoplasia, a result of the lung having failed to develop in utero as the thoracic cavity is filled by abdominal contents. Treatment is surgical, with the prognosis typically dependent on the degree of lung abnormality. Infants who present less than 6 hours after birth experience a 70% mortality, with much better survival if presentation occurs 12-24 hours after delivery [1].
These congenital diaphragmatic defects have also been described in the adult population, and the widespread use CT scanning has led to the recognition that these hernias are not uncommon and are often asymptomatic. In one series, 0.2% of over 13,000 patients undergoing CT examinations for other reasons were found to have hernias through the Foramen of Bochdalek. Most contained only omental fat, but small and large bowel and solid organs can be present. A much less common form of hernia may occur thru the Foramen of Morgagni, another potential defect in the diaphragm in the anteriomedial portion, near the heart. These account for only about 2% of CDH in the newborn period, but may present as paracardiac masses in the adult. With modern CT giving reconstruction facility amazingly help to diagnose these condition correctly as well as associated other anomaly or pathology and helping surgeons greatly [1].
Diaphragmatic injury may occur due to both penetrating and blunt traumas. The frequency with which either of these mechanisms leads to diaphragmatic injury varies according to the geographic location. The incidence of post-traumatic blunt diaphragmatic injury varies from 0.16 to 5%. Very few cases of delayed presentation of CDH in asymptomatic adults are described in the literature [4].
Imaging Findings on CT
CT scan with sagittal and coronal reconstructionis the modality of choice in adults as well as pediatric patients whenever there is clinical or radiological suspicion of diaphragmatic injury [2]. The various significant signs which have been described in diaphragmatic defect/ rupture are as follows:
a) Diaphragm discontinuity
b) Segmental non-recognition of diaphragm
c) "Dangling diaphragm" sign
d) "Dependent viscera" sign
e) Intrathoracic herniation of abdominal contents
f) "Collar sign"
g) Elevated abdominal organs
h) Thickened diaphragm
i) Thoracic fluid abutting intra-abdominal viscera
j) Hypoattenuated hemidiaphragm and associated fractured ribs in case of trauma.
4.4.1 Role of MRI: MR imaging may be used in more stable patients or where the CT examinations are equivocal. All the CT signs of diaphragmatic injury apply to MR also. MR imaging additionally provides superb soft-tissue resolution and demonstrates the diaphragm as a thin sheet of muscle separating the thoracic and abdominal cavities. It has low signal intensity relative to that of other skeletal muscles with all MR (T1 and T2 weighted sequences) imaging sequences [2].
Diagnostic Pitfalls
The main diagnostic pitfalls are many and include anatomic variants, congenital and acquired abnormalities. There are a few confusing factors that may prevent normal visualization of the diaphragm:
a) Portions of the diaphragm may abut structures of similar attenuation like liver and spleen normally
b) Few segments of the diaphragm may be parallel to the normal axial planes that are used in CT
c) Normal variants like diaphragmatic humps and areas of apparent discontinuity where the diaphragm inserts on the costal margins
d) Localized thinning (eventration) with maintenance of diaphragmatic continuity.
Management: Management of hernia includes reducing the abdominal contents and repairing the defect through a laparotomy or thoracotomy. Successful laparoscopic and thoracoscopic repairs of hernias have both been described. Right-sided defects are usually dealt with by a thoracic or thoracoabdominal approach because of the presence of the liver. For left-sided hernias some authors suggest a transthoracic approach while others advise a transperitoneal approach. The indications for repair of congenital diaphragmatic hernia are the same as those to treat any hernia, and should take into account the patient's overall medical condition. The outcome of adult patients suffering from hernia depends on the type of clinical presentation. Delay in the diagnosis of any hernia can result in significant morbidity.
Conclusion
In summary, intense knowledge of all CT signs of diaphragmatic injury is essential in reaching the diagnosis of diaphragmatic rupture and identifying its complications so that the patient can get proper treatment. Presence of a single sign should alert the radiologist to search for the diaphragm more closely and presence of two or more signs increases the probability of traumatic diaphragmatic hernia along with detailed clinical history and previous investigation if available.
References
- Leigh S Shuman (2015) Diaphragmatic Hernias.
- Ravinder Kaur, Anuj Prabhakar, Suman Kochhar, Usha Dalal (2015] Blunt traumatic diaphragmatic hernia: Pictorial review of CT signs. 25(3): 226-232.
- Mullins ME, Stein J, Saini SS (2001) Prevalence of incidental Bochdalek's hernia in a large adult population. AJR Am J Roentgenol 177(2): 363366.
- Enrica Bianchi, Paola Mancini, Stefania De Vito, Elena Pompili, Samanta Taurone, et al. (2015) Congenital asymptomatic diaphragmatic hernias in adults: a case series.






























