Young Female with Large Cervical Mass
Sushila Ladumor B1*, Adham Darweesh2 and Hiba Esmayil3
1Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, Doha, Qatar, Assistant Professor in Clinical Radiology, Weil Cornel Medical College, Qatar
2Senior Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, Doha, Qatar, Assistant Professor in Clinical Radiology, Weil Cornel Medical College, Qatar
3R1 Radiology Resident, Hamad Medical Corporation, HGH, Clinical Imaging, Qatar
Submission: September 01, 2017; Published: September 11, 2017
*Corresponding author: Sushila Ladumor B, Consultant Radiologist, Clinical Imaging Department, Hamad Medical Corporation, HGH, Doha, Qatar, Assistant Professor in Clinical Radiology, Weil Cornel Medical College, Doha, Qatar (WCMC-Q), E-mail: drsbladumor@yahoo.com
How to cite this article: Sushila L B, Adham D, Hiba E. Young Female with Large Cervical Mass. Open Access J Surg. 2017; 5(5): 555674. DOI: 10.19080/OAJS.2017.05.555674
Abstract
Carcinoma of the cervix is a malignancy arising from the cervix and is considered the third most common gynecologic malignancy (after endometrial and ovarian) and is one of the most common malignancies seen by gynecologic radiologists. The occurrence of invasive cervical cancer is higher in low-income countries due to lack of screening programs. In developed countries, the incidence of invasive cervical cancer decreased after implementation of the Papanicolaou smear test (PAPS Smear) [1]; indeed, in the United States, cervix uteri cancer represents only 0.8% of all new cancer cases. It affects mostly women of reproductive age; 14.0% of patients diagnosed with cervical cancer are between 20 and 34 and 25.9% between 35 and 44 years of age [2].
Keywords: Cervical cancer; Ultrasound; Computed tomography; Positron emission tomography/ computed tomography; Magnetic resonance imaging; Diffusion Restriction; ADC Apparent diffusion coefficient); Tumor staging; FIGO; Metastasis; Hydro nephrosis; Histopathology
Clinical History
38 years old female, para 1, normal delivery before 4yrs with regular cycles, missed one cycle before presentation came with history of inter menstrual bleeding, vaginal spotting for 2 days at the beginning and end of next month (Month of presentation) associated with watery vaginal discharge, offensive, not itchy. H/O weight loss more than 20 kg in 6 months patient was seen last week in Primary Health care Centre and pelvic scan done, showing uterine fibroid and large left adnexal mass, referred to main Hospital for further evaluation and work-up.
Local Examination
a) Abdomen: soft, non-tender, no masses felt
b) Speculum exam: There was watery vaginal discharge, foul smelling, large cervical mass seen (papilloma like), friable, bleeding to touch, cervical os couldn’t be visualized part of this tissue taken for histopathology, pap smear could not be taken.
c) Per Vaginal Exam: Appears as large left adnexal mass felt, not tender.
Imaging Findings
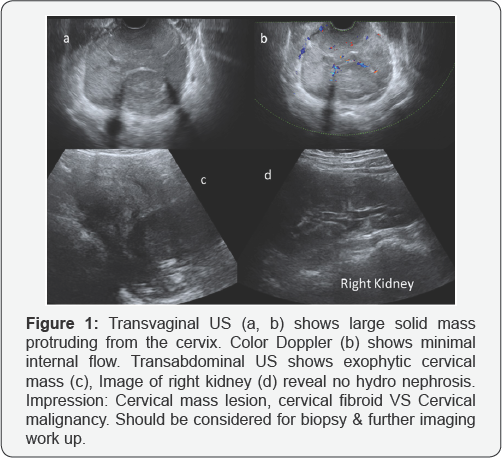
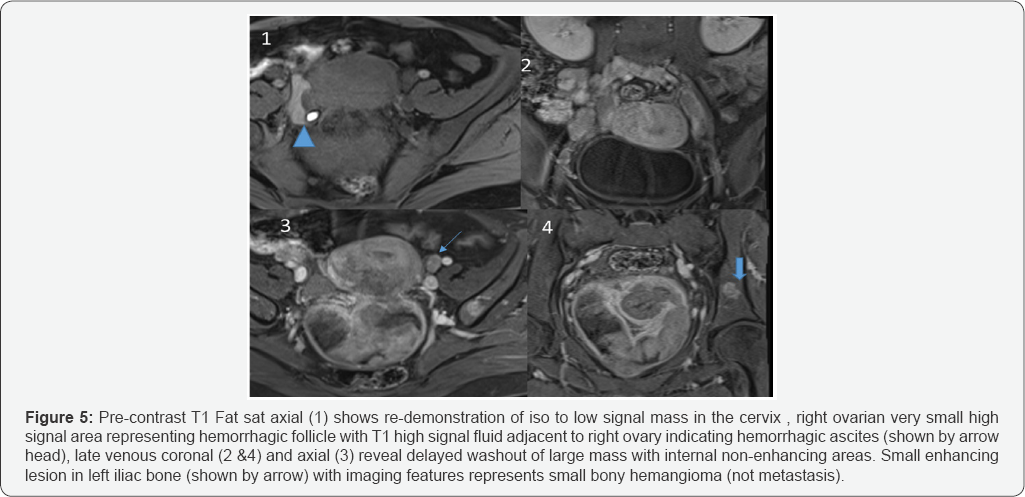
Initial US (Trans Vaginal and Transabdominal US) done show large cervical mass with some vascularity on color Doppler. Further work up recommended for better characterization of large cervical mass (Figures 1-5).
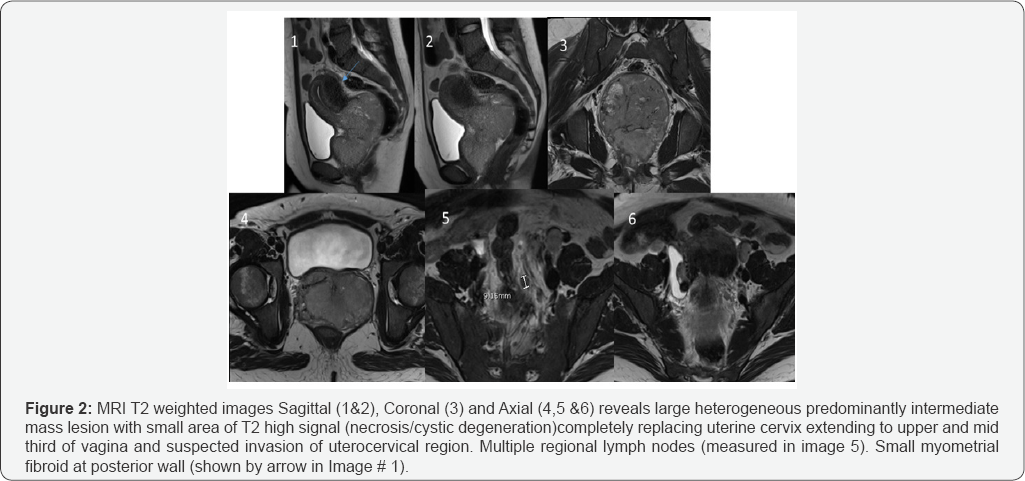
a) MRI: Detailed Report.
b) Tumor: Large exophytic polypoidal cervical mass measuring 9.4 x 6.4 x 11 cm with protrusion into vaginal fornices and upper and lower third vagina. The mass demonstrates intermediate T2 signal relative to myometrium, restriction diffusion and early heterogeneous enhancement and delayed washout. Multiple areas of signal voids are noted suggesting calcifications.
c) Parametria: Stretched cervical stroma showing intact dark T2 fibrous lining appears intact.
d) Vagina: tumor seen extending to lower vagina without disruption of the vaginal wall.
e) Pelvic wall: No pelvic wall involvement.
f) Lower uterine segment: Suspected involvement.
g) Bladder and Rectum: intact wall. The rectum is compressed by large cervical mass
h) Lymph nodes: enlarged intermediate T2 external lymph nodes with maximum dimension measures 35 mm on the right side and 32 mm on left side. Few small internal iliac and presacral lymph nodes largest measures 9 mm measured along left internal iliac chain. Small lymph node in the distal aortocaval region measures about 6.5 x 13 mm.
i) Ancillary findings: Mild pelvic free fluid showing hyper intense T1 signal likely of thick content with possibility of malignant ascites
j) Uterus: endometrial thickness of 1.8 mm. Posterior sub serosal leiomyoma measuring 6 x 3 x 3.5 cm. No extension into lower uterine segment
k) Ovaries: Right ovary measures about 2.6 x 1 x 2 cm showing two bright T1 follicles likely represent endometriotic deposits. Superior displacement of left ovaries otherwise within normal.
l) Osseous structures: signal changes along bilateral sacro-iliac joints likely degenerative changes. Partially ill- defined intramedullary lesion at left iliac bone measuring 12.5 x 10 mm demonstrated no restricted diffusion, intracellular fat in opposed phase sequence and showing early and persistent delayed contrast enhancement, likely benign (hemangioma).
Diagnosis
a) Large exophytic cervical mass, with Imaging features representing cervical cancer, Stage IIIA, N1. Possibility of metastatic external iliac nodes. Mild ascites with thick content could represent malignant ascites. For tissue diagnosis.
b) Posterior uterine leiomyoma. Right ovarian endometriosis.
Histopathology Report
A. Specimen Source
i. Cervical mass
ii. Cervical mass biopsy
B. Diagnosis
i. Cervical Mass, Biopsy: High grade carcinoma, mixed type of clear cell carcinoma and Non-keratinizing squamous cell carcinoma, favor cervical primary.
ii. Cervical mass biopsy: Nonviable infarct necrosis.
Epidemiology
It typically presents in younger women with the average age of onset at around 45 years.
Risk factors
I. Human papillomavirus (HPV) 16 and 18 infections: for most types except for clear cell carcinoma of the cervix and mesonephric carcinoma of the cervix
II. Multiple sexual partners or a male partner with multiple previous or current sexual partners
III. Young age at first intercourse
IV. High parity
V. Immunosuppression
VI. Certain HLA subtypes
VII. Oral contraceptives
VIII. Nicotine/smoking (except for cervical adenocarcinoma 26)
Clinical presentation
Presenting symptoms include:
a) Vaginal bleeding
b) Vaginal discharge
c) Subclinical with an abnormality detected on Pap smear screening
Histological types
The main histological types are:
a. Squamous cell carcinoma of the cervix: accounts for the vast majority (80-90%) of cases and is associated with exposure to human papillomavirus (HPV)
b. Adenocarcinoma of the cervix: rarer (5-20%) and can have several subtypes which include 11,20 clear cell carcinoma of the cervix.
c. Endometroid carcinoma of the cervix: ~7% of adenocarcinomas 21
d. Mucinous carcinoma of the cervix
e. Adenoma malignum: ~3% of adenocarcinomas
f. serous carcinoma of the cervix
g. Mesonephric carcinoma of the cervix: ~3% of adenocarcinomas 23
h. Neuroendocrine tumors of the cervix
i. Small cell carcinoma of the cervix: rare (0.5-6%) 18,22
Location
Cervical squamous cell carcinoma arises from the squamocolumnar junction while adenocarcinomas arise from the endocervix. This is situated on the ectocervix in younger patients though regresses into the endocervical canal with age. Hence cervical tumors tend to be exophytic in younger patients and endophytic with advancing age.
Radiographic features
General features: In order to be radiographically visible, tumors must be at least stage Ib or above. MRI is the imaging modality of choice to depict the primary tumor and assess local extent. Distant metastatic disease is better assessed with CT or PET, whatever available. Although the FIGO staging system is clinically based, the revised 2009 FIGO staging encourages imaging as an adjunct to clinical staging. MRI can help patients to the best treatment as option for primary surgery or combined chemotherapy and radiotherapy. Tumors stage IIa and below are treated with surgery.
Imaging Appearance
A. Ultrasound
a. Hypoechoic, heterogeneous mass involving the cervix
b. May show increased vascularity on color Doppler
c. Mainly cervical cancer is staged clinically, ultrasound can be a useful adjunct by showing
d. Size (<4 cm or >4 cm)
e. Parametrial invasion
f. Tumor invasion into the vagina ( High resolution Transvaginal Ultrasound)
g. Tumor invasion into adjacent organs
h. Hydro nephrosis (Abdominal Ultrasound): implies stage IIIB tumor.
B. CT
CT, in general, is not choice of investigation for evaluation of the primary tumor, but it is very important in assessment of advanced disease. It is performed primarily to assess regional and distant adenopathy, but also has roles in defining advanced disease, monitoring distant metastasis and planning the placement of radiation ports. On CT, the primary tumor can be hypo enhancing or isoenhancing to normal cervical stroma (~50% 19).
C. PET-CT
PET-CT in combination with pelvic MRI is usually used as an imaging strategy in helping stage cervical carcinoma.
D. MRI
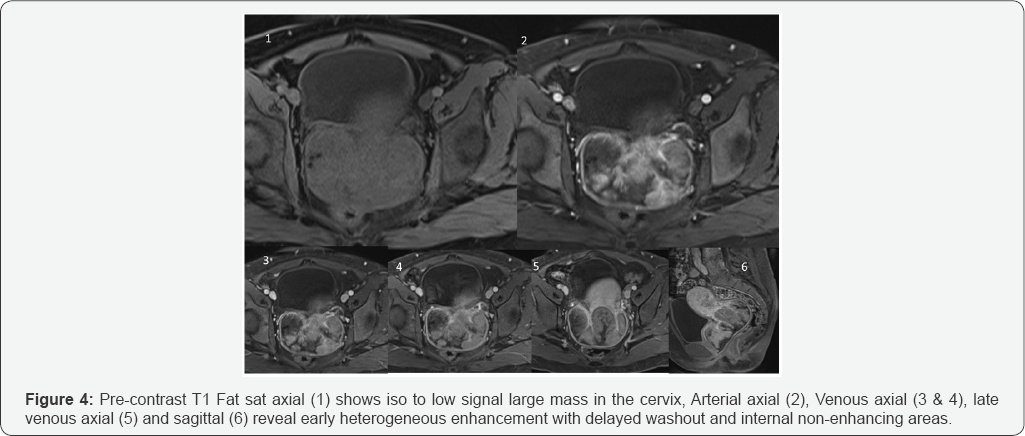
A dedicated contrast enhanced MRI protocol is used for accurate diagnosis and staging. The normal cervical stroma demonstrates T1 and T2 low signal yield intrinsic contrast for the T2 high signal cervical tumor.
Usual Signal Characteristic of Cervical Malignancy
a. T1 Weighted sequence: Usually isointense compared with pelvic muscles
b. T2 Weighted sequence: Usually hyper intense in relation to the low signal of the cervical stroma, hyper intensity is thought to be present regardless of histological subtype 1
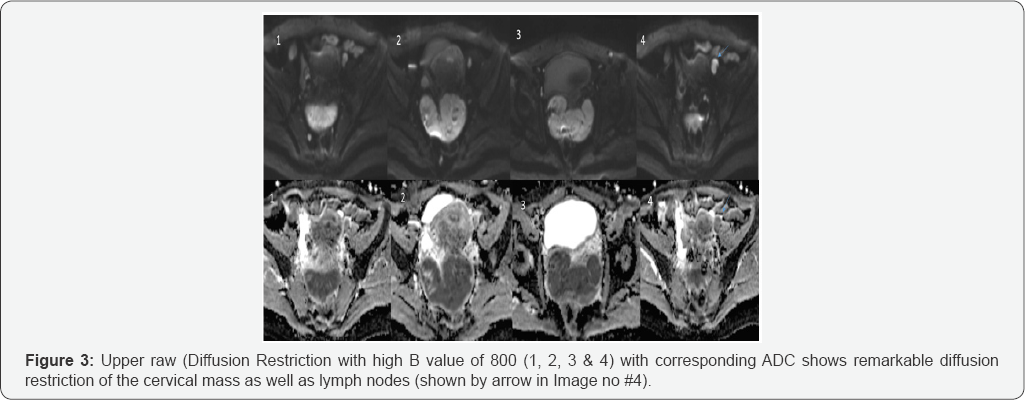
c. Diffusion Weighted sequence Mostly significant Diffusion Restriction which appears low signal in ADC
d. T1 C+ (Gadolinium)
Contrast is not routinely used in some institute, though it may be helpful to demonstrate small tumors. On contrast- enhanced fat sat T1-weighted images, tumorshows early arterial enhancement relative to the low signal of the cervical stroma which demonstrates relative washout in delayed post-contrast images (Typical imaging features are seen frequently in small lesion than larger lesion).
E. Staging
Revised FIGO staging of cervical carcinoma 2009
a) Stage 0: cervical intraepithelial neoplasia (HSIL or CIN III)
b) Stage I: confined to cervix
c) Stage I a: invasive carcinoma only diagnosed by microscopy.
d) Ia1: stromal invasion <3 mm in depth and <7 mm in extension (micro invasive)
e) Ia2: stromal invasion >3 mm depth and not >5 mm and extension <7 mm
f) Stage Ib: clinically visible lesions limited to the cervix or pre-clinical cancers >stage 1a
g) Ib1: clinically visible tumor <4 cm in greatest dimension
h) Ib2: clinically visible tumor >4 cm in greatest dimension
i) Stage II: beyond cervix though not to the pelvic sidewall or lower third of the vagina.
j) Stage IIa: involves upper 2/3rd of vagina without parametrial invasion k) Stage IIa1: clinically visible tumour <4 cm in greatest dimension
l) Stage IIa2: clinically visible tumour >4 cm in greatest dimension
m) Stage IIb: with parametrial invasion
n) Stage III
o) Stage IIIa: tumour involves the lower third of the vagina with no extension to pelvic sidewall
p) stage IIIb: extension to pelvic side wall or causing obstructive uropathy, MR imaging findings that are suggestive of pelvic sidewall involvement include tumour within 3 mm of or abutment of the internal obturator, levator ani, and pyriform muscles and the iliac vessel 6
q) Stage IV: extension beyond true pelvis or biopsy proven to involve the mucosa of the bladder or the rectum
r) Stage IVa: extension beyond true pelvis or rectal/ bladder invasion
s) Stage IVb: distant organ spread
Treatment and prognosis is affected by many factors which include
a) Tumor stage
b) Volume of the primary mass
c) Histologic grade
Five-year survival rates vary between 92% for stage I disease and 17% for stage IV disease. One of the very important roles of the radiologist is to help in determine staging, as this may lead to appropriate management pathway either with surgery or chemo-radiotherapy. At the time of writing stage IIa vs. IIb is considered as an important separator in deciding whether a case is operable or not.
Differential diagnosis
For a mass involving the cervix consider:
a. Cervical polyp
b. Cervical leiomyoma
c. Invasion of the cervix from
d. Primary uterine malignancy
e. Vaginal cancer
f. Cervical lymphoma
g. Adenoma malignum: often considered a subtype of mucinous carcinoma of the cervix
h. Metastases to the cervix
i. Cervical ectopic pregnancy: consider with women of childbearing age with a high βHCG
j. Practical points: MRI T2WI to assess parametrial invasion (stage 2b) is crucial to determine if the patient is candidate for surgery or not
Discussion
Squamous cell carcinoma of cervix is one of the most common gynecological malignancies [1]. Carcinoma of cervix can involve the uterine corpus by direct extension or through parametrium by lymphatic invasion to the uterine wall [1,2]. Most cervical squamous cell carcinomas grow at the SCJ. In younger women, the SCJ is located outside the external uterine os, and the tumor tends to grow outward (exophytic growth pattern) (in this case) In contrast, in elderly patients, the SCJ is located within the cervical canal. In these patients, cervical cancer tends to grow inward along the cervical canal (endophytic growth pattern). Reserve cells at the SCJ have been watched with interest as an origin site of cervical adenocarcinoma. Therefore, most cervical adenocarcinomas would also arise in the SCJ.
MR imaging can provide highly accurate information on the exact extent of tumors because of its best contrast resolution. Cervical cancers shows high signal masses on T2-weighted images regardless of histopathologic type. Mostly significant Diffusion Restriction which appears low signal in ADC. (Diffusion weighted imaging (DWI) is a form of MR imaging based upon measuring the random Brownian motion of water molecules within a voxel of tissue. The relationship between histology and diffusion is complex; however, in general, highly cellular tissues or those with cellular swelling exhibit lower diffusion coefficients, and thus diffusion is particularly useful in tumor characterization as well as in diagnosing cerebral ischemia.
A much safer and more accurate way of referring to diffusion restriction is to remember that we are referring to actual ADC values, and to use wording such as "the region demonstrates abnormally low ADC values (abnormal diffusion restriction)" or even "high signal on isotropic images (DWI) is confirmed by ADC maps to represent abnormal restricted diffusion "as seen in our case.) The usefulness of dynamic contrast material- enhanced studies in diagnosing parametrial invasion and predicting radio sensitivity has been reported [3-5], although sagittal T1-weighted and T2-weighted images and oblique axial T2-weighted images obtained perpendicular to the uterine axis are sufficient for staging in most cases [6]. MR urography and contrast enhanced computed tomography (CT) or PET CT are also important in diagnosing hydro nephrosis associated with cancer invasion, paraaortic lymph node metastases, or other distant metastases in lung, solid organs and bones.
In general, staging of cervical carcinoma with MR imaging is based on the classification system of the International Federation of Gynecology and Obstetrics (FIGO) [7]. Thus, stage Ia is defined as a micro invasive tumor that cannot be demonstrated at MR imaging. Stage Ib is defined as a clinically invasive tumor, although it is confined to the cervix and does not invade/ extend the vagina or parametrium. In stage Ib, the tumor is completely surrounded by hypo intense cervical stroma on axial T2-weighted images [8-10]. Stage IIa is defined as a tumor that invades the upper two-thirds of the vagina without parametrial invasion. Segmental disruption of the hypo intense vaginal wall is demonstrated on T2-weighted images [8-10]. When the tumor invades beyond the uterus with parametrial invasion without reaching the pelvic wall, it is defined as stage IIb. At MR imaging, triangular protrusion of the tumor through the disrupted hypo intense ring of cervical stroma is seen [8-10].
In stage IIIa, vaginal involvement reaches the lower third of the vaginal canal without extending to the pelvic wall. Occasionally, the anterior vaginal wall is partly disrupted and the tumor infiltrates the bladder wall but not the vesical mucosa. When the tumor extends to the pelvic wall or causes hydro nephrosis, it is defined as stage IIIb. At MR imaging, the tumor obliterates the entire cardinal ligament and extends to the pelvic muscles. Hydro nephrosis caused by tumor invasion of the ureter is also classified as stage IIIb. MR urography can clearly demonstrate hydro nephrosis caused by tumor extension.
If the tumor invades the vesical or rectal mucosa, it is classified as stage IVa. Segmental disruption of the hypo intense vesical or rectal wall or a segmental thickened rectal wall is seen at MR imaging [8-10]. Once any distant metastases occur, the stage is defined as IVb. Although pelvic lymph node metastases do not change the International Federation of Gynecology and Obstetrics stage, paraaortic or inguinal lymph node metastases are classified as stage IVb. Cervical cancer occasionally causes carcinomatous lymphangitis of the lung or hematogenous hepatic metastases. CT plays a major role in diagnosing such advanced disease.
MR imaging is also useful for evaluation of the postoperative state [11]. Conization is usually performed as a radical surgery for carcinoma in situ or micro invasive carcinomas or as a diagnostic procedure in cases suspected to be invasive cervical carcinoma. Conization may be used either for diagnostic purposes as part of a biopsy, or for therapeutic purposes to remove pre-cancerous cells. Otherwise, abdominal radical hysterectomy is a standard surgery for stage Ib and IIa disease. Diagnosis of local recurrence after surgery or radiation therapy can also be achieved with MR imaging.
Chemo radiation is the optimal treatment for advanced cervical cancer (> IIB); in these patients, surgery provides no additional survival benefit, while it exposes the patients to the surgical risk and delays radiation therapy. In a significant number of patients treated with surgery, more advanced disease requiring adjuvant chemoradiation is found on final surgicopathological examination; interestingly, it has been shown that surgical treatment followed by chemoradiation, increases significantly the morbidity of these patients. Therefore, the ability to distinguish early (operable) from advanced (non- operable) cervical cancer is crucial. The FIGO staging system has several limitations which may lead to under- or overestimation of the extent of disease at diagnosis, adversely affecting patient optimal care.
Conclusion
Imaging studies provide more information than clinical examination for the evaluation of patients with cervical cancer and their results may be used by clinicians to make appropriate therapeutic decisions in multidisciplinary meeting. MRI is the preferred imaging modality for the initial staging of uterine cervical cancer and its use may increment the clinical prognostic value. MRI is particularly helpful in evaluating patients with cervical cancer who are candidates for trachelectomy (A trachelectomy is a surgical procedure used to treat eligible women with early stage cervical cancer who wish to preserve their fertility and ability to carry a child. There are two types of trachelectomy: a radical trachelectomy and a simple trachelectomy with upper vaginectomy, both of which remove pelvic lymph nodes) or for predicting tumor origin in patients with bulky uterine masses of indeterminate histology [12].
In patients with clinical evidence of tumor relapse, the combination of MRI and PET/CT data may reliably evaluate both local and distant spread of the disease, optimizing the therapeutic management of these patients. Functional imaging techniques, like DWI, appear to be promising cancer biomarkers for predicting therapeutic outcome but further studies and imaging protocol standardization are needed to support clinical implementation.
References
- Gungor T, Altinkaya SO, Ozat M, Akbay S, Mollamahmutoglu L (2011) Unusual form of superficial spreading squamous cell carcinoma ofcervix involving the endometrium, bilateral tubes and ovaries: A case report with literature review. Arch Gynecol Obstet 283: 323-327.
- Agashe SR, Kulkarni MP, Momin YA, Sulhyan KR (2007) Superficial extension of squamous cell carcinoma in situ of cervix involving endometrium, bilateral fallopian tubes and ovaries: A case report. Indian J Pathol Microbiol 50: 375-377.
- Yamashita Y, Takahashi M, Sawada T, Miyazaki K, Okamura H (1992) Carcinoma of the cervix: dynamic MR imaging. Radiology 182: 643648.
- Feldmann HJ, Sievers K, Fuller J, Molls M, Lohr E (1993) Evaluation of tumor blood perfusion by dynamic MRI and CT in patients undergoing thermoradiotherapy. Eur J Radiol 16: 224-229.
- Hawighorst H, Knapstein PG, Weikel W (1997) Angiogenesis of uterine cervical carcinoma: characterization by pharmacokinetic magnetic resonance parameters and histological microvessel density with correlation to lymphatic involvement. Cancer Res 57: 4777-4786.
- Shiraiwa M, Joja I, Asakawa T (1999) Cervical carcinoma: efficacy of thin-section oblique axial T2-weighted images for evaluating parametrial invasion. Abdom Imaging 24: 514-519.
- Benedet JL, Bender H, Jones H, Ngan HYS, Pecorelli S (2000) FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. Int J Gynecol Obstet 70: 209-262.
- Sironi S, Belloni C, Taccagni GL (1991) Carcinoma of the cervix: value of MR imaging in detecting parametrial involvement. AJR Am J Roentgenol 156: 753-756.
- Togashi K, Nishimura K, Sagoh T (1989) Carcinoma of the cervix: staging with MR imaging. Radiology 171: 245-251.
- Togashi K, Morikawa K, Kataoka ML, Konishi J (1998) Cervical cancer. J Magn Reson Imaging 8: 391-397.
- Macgregor JE, Campbell MK, Mann EM, Swanson KY (1994) Screening for cervical intraepithelial neoplasia in north east Scotland shows fall in incidence and mortality from invasive cancer with concomitant rise in preinvasive disease. BMJ 308: 1407-1411.
- (2015) SEER Data: Surveillance, Epidemiology and End Results.





























