Hemorrhoidal Disease and Iliac Vein Stenosis A New Etiologic And Therapeutic Approach Preliminary Results
Guilleuma Juan1* and Jimenez A2
1Consultant Vascular Surgery, Hospital Virgen de La Paloma, Spain
2Consultant Cardiovascular Surgery, Hospital Virgen de La Paloma, Spain
Submission: August 15, 2017; Published: August 21, 2017
*Corresponding author: Juan Guilleuma, Paseo del Hontanar 1, casa 9 28223 Pozuelo de Alarcon, Madrid, Spain, Tel: +34619229304; Email: juanguilleuma@telefoinica.net
How to cite this article: Guilleuma J Jimenez A. Hemorrhoidal Disease and Iliac Vein Stenosis A New Etiologic And Therapeutic Approach Preliminary Results. Open Access J Surg. 2017; 5(3): 555663. DOI: 10.19080/OAJS.2017.05.555663
Abstract
Aim: To evaluate the anatomic correlation between hemorrhoidal pathology with stenotic or occlusive iliac vein disease and to demonstrate the efficacy and safety of iliac vein stenting by IVUS evaluation and clinical enhancement of symptomatic hemorrhoids after iliac vein stenting.
Material/Methods: Five patients with grade >1 hemorrhoids 1 male and 4 female patients with mean age 49.7 years (range 35-58) where included in the study. Three of them had associated manifestation of lower leg chronic venous insufficiency. Under local anesthesia patients were operated by both femoral veins using Seldinger technique. After phlebography, an intravenous ultrasound (IVUS) imaging was performed. When vessel luminal area stenosis greater than 30% was detected, stent angioplasty of iliac vein was performed. All patients were discharged following the procedure on platelet anti- aggregant treatment.
Results: Uni or bi lateral iliac venous system obstructive pathology was found in all of the patients, detected by IVUS. All lesions were successfully treated by wallstent stent deployment. Mean number of stents per patient was 2,2 (range 2-3). No perioperative complications developed except transitory abdominal pain. There was a 12 months follow-up completion and hemorrhoidal symptoms relief was present in all patients.
Conclusion: Hemorrhoids present a very close association with stenotic lesions of iliac veins. Additionally these venous obstructions are involved in hemorrhoidal etiology, as demonstrated by clinical enhancement after endovascular treatment with iliac stenting.
Keywords: Hemorrhoid- Intravascular ultrasound- Iliac vein stent-endovascular surgery
Abbreviations: pts : Patients; IVUS: Intravascular Ultrasound; IVIS: Iliac Vein Insufficiency Syndrome
Introduction
Hemorrhoids are a very common anorectal condition defined as the enlargement and distal displacement of the normal hemorrhoidal venous plexi. The pathophysiology of hemorrhoidal development is poorly understood. Although an inflammatory reaction and vascular hyperplasia [1,2] may be evident in hemorrhoids, these could be more a consequence than a primary cause of this disease. Classically it was assumed that hemorrhoids were associated with increased hydrostatic pressure in the portal venous system [3], but this hypothesis does not correlate with clinical findings. Today, the theory of sliding anal canal lining is widely accepted [4]. This proposes that hemorrhoids develop when the supporting tissues of the anal cushions disintegrate or deteriorate.
Our hypothesis postulates that hemorrhoids are caused by primary venous hypertension and the pathological changes of the surrounding connective tissues are a consequence of this sustained hypertension. This supposition is supported by classical anatomical descriptions remarking that middle and inferior hemorrhoidal plexi drain to the internal iliac veins, but the superior plexus is a tributary of the portal system. Thus, iliocaval chronic occlusive lesions could be involved in hemorrhoid development and progression. The venous iliocaval system has been studied by several imaging techniques including phlebography, angio-CT scan and magnetic resonance. Currently intravascular ultrasound (IVUS) is the most sensitive method to detect iliac vein stenosis as well as its length with adequate accuracy. Although endovascular techniques have been used since early 90´s [5], to treat iliocaval stenotic lesions, none of them have been focused in solving hemorrhoids as a primary target. The goal of this study is to review our initial results and discuss the evolution and endovascular treatment indications for hemorrhoidal pathology according to our experience.
Material and Methods
During 2015, 5 consecutive patients (pts) with grade >1 hemorrhoids were admitted for endovascular treatment by detecting possible iliac vein obstructive lesions (cut-off point >30% stenosis). All pts. were diagnosed by clinical history and visual inspection. The main exclusion criteria were severe associated comorbidities and no acceptance of the need for invasive treatment. There were 4 female and 1male (median age 49.7years; range 35-58 years). All of them had hemorrhoids grade>1, either isolated or associated with clinical manifestations of chronic lower limbs venous insufficiency or pelvic congestive syndrome. Two pts. had a history of varicose vein surgery.
The initial imaging exploration in all patients consisted of color Doppler ultrasonography of the lower extremities and pelvis to identify any obstructive lesions and detect superficial and/or deep reflux and collateral pathways. Computed tomographic venography or magnetic resonance venography was performed in all pts trying to diagnose compressive iliac vein pathology, for instance a May-Thurner syndrome. No preoperative Iliocavography was performed.
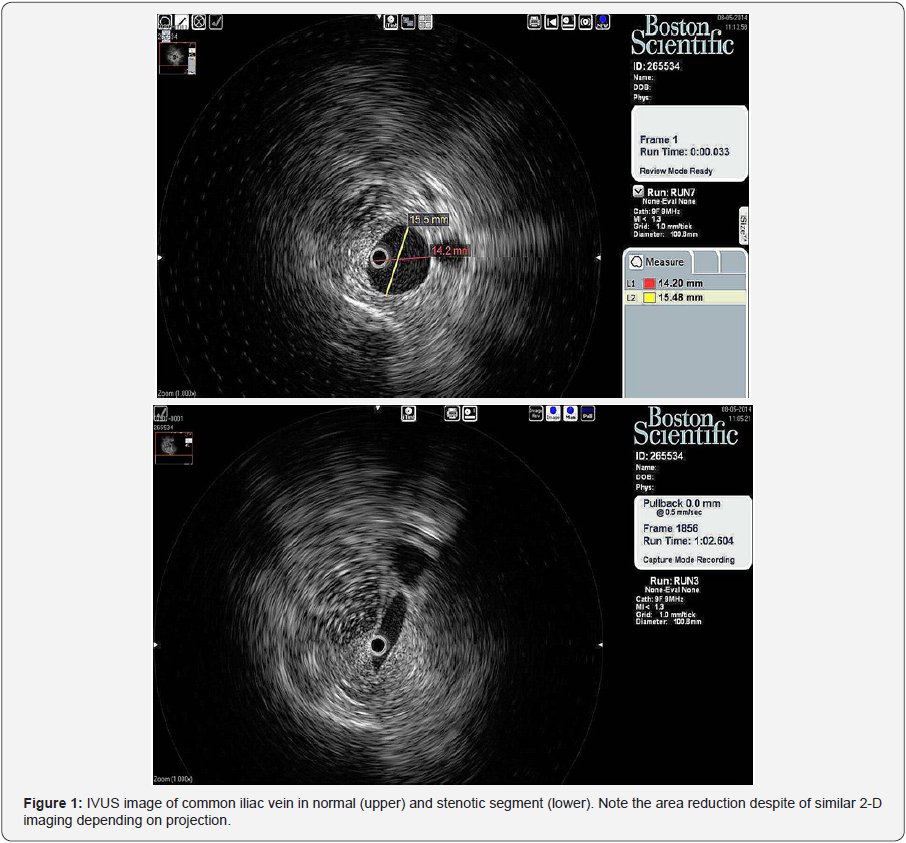
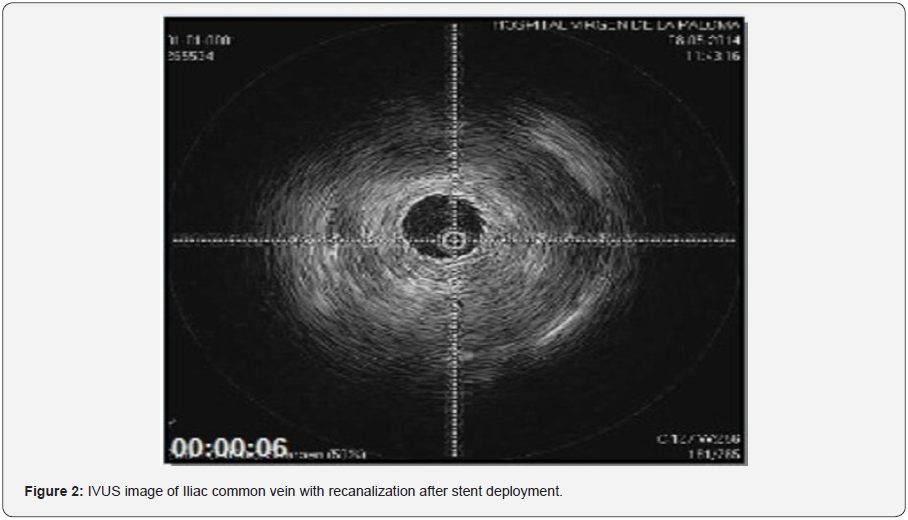
Prior to operation the pts were consent for treatment and explained all pros and cons of the procedure in accordance with the hospital preoperative regulations compliant with the Spanish regulations. All procedures were performed in the operating room under local anesthesia plus sedation. Percutaneous access was performed through the common femoral veins in all patients by Seldinger technique with 11F sheaths. After catheterization of the lesion and intraoperative bilateral iliocavography an IVUS probe (Atlantis™ SR Pro Imaging Catheter, Boston Scientific, Minneapolis, Minn)was inserted and connected to an iLab™ Ultrasound Imaging System (Boston Scientific, Minneapolis, Minn) allowing us an in depth exploration of both iliac venous systems and their pathways (Figures 1 & 2).
For lesions more than 30% area of stenosis in the vein lumen, the length of the lesion was marked. Direct deployment of a self-expanding metallic stents (Wallstent, Boston Scientific, Minneapolis, Minn) was performed, followed by balloon angioplasty when necessary (XXL Esophageal, Boston Scientific, Minneapolis, Minn). Completion IVUS was then performed and sheaths were retrieved before direct smooth compression. Patients were kept bed rest for 4 additional hours. The postoperative treatment included i.v. analgesics; and eventually discharged the same day of operation on antiplatelet drugs (clopidogrel 75 mg o.d.). Follow-up was scheduled at 1, 3, 6, and 12 postoperative months. Clinical examination and duplex scanning were performed on every visit. The primary endpoint was to evaluate the anatomic correlation between hemorrhoidal pathology with stenotic or occlusive iliac vein disease and the secondary endpoints were to demonstrate the efficacy and safety of iliac vein stenting by IVUS morphologic evaluation and clinical enhancement of symptomatic piles after iliac vein stenting.
Results
Bilateral iliac lesions were found in all pts. There were no complete occlusions but stenoses affecting the common iliac veins. Primary external compression (including May-Thurner syndrome) was found in all pts. No perioperative death or pulmonary embolism occurred. All stenoses were successfully treated. Overall, 10 venous segments were treated, all in the common iliac veins. The technical success rate was 100%. Eleven stents (18-22 mm in diameter and 40-90 mm long) were used all in the common iliac veins. In all cases, the stent proximal end was deployed beyond the iliocaval junction, and one common iliac vein was treated with two stents. The mean number of stents per patient was 2.2 (2-3). The mean length of stented vein segments was 58 mm (range 40-120 mm). No concomitant procedures were performed and no patients had early or midterm thrombosis.
Three patients (60%) developed severe back or abdominal pain immediate to stent deployment or balloon expansion, needing intravenous analgesia. All patiens had an uneventful postoperative recovery. The median hospital stay was 5 hours (range, 3-7 hours) and all patients were on antiplatelet drug therapy at discharge. The median follow-up was 8 months (range, 4-12 months) with no major or late mortality events reported. No late thrombosis has been documented.
Discussion
Classically, the approach to hemorrhoidal disease has been based on two main issues.
- The assumption that main hemorrhoidal veins drain to portal system, and
- The presence of degenerative changes in the supporting connective tissue within the anal cushion [6,7]. Actually all treatment modalities are focused basically on hemorrhoids themselves and not directed towards capital etiologic factors [8-12].
When we learned about the IVUS potential to detect previously unknown lesions in the iliac veins we began to think about relationship between other pelvic vein diseases and the iliac vein system.
Reviewing the anatomy of the hemorrhoidal plexi we found that the superior hemorrhoidal plexus drains to the portal vein system, but the inferior one drains to the iliac vein system and the medial one just connects to both of them. Additionally the medial hemorrhoidal veins all have unidirectional valves allowing flow to drain only from the superior to the inferior hemorrhoidal veins [13]. This fact can explain why hemorrhoids are not an important clinical fact in portal hypertension, and supports our assumption of common iliac vein stenosis as a critical issue on the physiopathology of hemorrhoids. With these two facts in mind we decided to perform a clinical/anatomic research in a group of patients with hemorrhoidal disease, by IVUS exploration of the iliac veins.
Our finding of a 100% anatomic correlation between hemorrhoidal disease and lesions in the common iliac vein supports our initial hypothesis, although further studies are needed to document our findings. We have considered a cut-off point of treatment of 30% area reduction in the iliac common vein. This could be controversial but based on Poiseuille´s and Bernouilli´s laws applied to the low-pressure venous system. In addition to this anatomical and physiopathologic basis, our clinical results support our initial assert. Every symptomatic patient treated became clinically asymptomatic. Once corrected all asymptomatic treated patients remain steady and stable. However we believe a longer sample and follow-up is needed.
Although our results support our initial idea, this does not mean that every patient with hemorrhoids will have iliac vein stenoses or that every iliac vein stenosis means the development of future hemorrhoids. Other local and genetic factors might influence the development of the disease. Even more these clinical and anatomical relationship between hemorrhoids and iliac vein stenosis, even with tiny stenosis, is highly surprising, and make us think about the complexity of the venous system pathophysiology, so many times disregarded, were it seems minor pressure gradients may have an important clinical response. Based on all this findings, it seems logical to look for new pathophysiological approach to hemorrhoidal disease and its treatment as well, focused on the iliac vein flow obstruction as etiologic issue, and not on the consequences: the hemorrhoids themselves. Despite of minimal antithrombotic treatment, there no were thrombosis events in follow-up. These results demonstrate that venous stent implantation is a safe technique, specially for stenotic lesions as result of extrinsic compression.
If our results are confirmed, the safety and simplicity of this interventional procedure let us to propose a changing approach on hemorrhoidal disease. From early stages is justified to perform an IVUS study and iliac vein stent placement to stop the progression of the disease. From our point of view this previous reflections open a new approach to understand the “world” of the inferior venous system. From our study and others in the literature is highly likely that sooner or later a new syndrome will be accepted: the Iliac Vein Insufficiency Syndrome (IVIS), encompassing different clinical manifestations as congestive pelvic syndrome, dyspaurenia, painful menses, hemorrhoids, lower legs varicosities and chronic venous insufficiency, as other studies have presumed [14-16].
This easy parallels if we review our knowledge about chronic venous insufficiency where different clinical manifestations such as varicosities, ulcers, orthostatic clinic, perforators insufficiency ..., all have a common etiology, which is a simple venous proximal reflux.
Conclusion
In our study hemorrhoids and iliac veins obstructive pathology are very close related probably due to hemorrhoidal plexi drainage impairment. This venous obstructive pathology could be a major paramount in hemorrhoid etiopatogenia. As seen in this article, iliac veins angioplasty and stenting is a safe and efficient minimally invasive technique for treatment of hemorrhoidal disease. Initial patency rates and symptom enhancing are excellent, and this technique does not preclude subsequent procedures. Further studies will be necessary in order to confirm these preliminary results.
References
- Morgado PJ, Suárez JA, Gómez LG, Morgado PJ (1988) Histoclinical basis for a new classification of hemorrhoidal disease. Dis Colon Rectum 31: 474-480.
- Aigner F, Gruber H, Conrad F, Eder J, Wedel T, et al. (2009) Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. Int J Colorectal Dis 24: 105-113.
- Lamont JT, Isselbacher KJ (1987) Diseases of the small and large intestine. In Harrison´s Principles of Internal Medicine, 11th edn, pag 1301.
- Thomson WH (1975) The nature of haemorrhoids. Br J Surg 62: 542-552.
- Juhan C, Hartung O, Alimi Y, Barthelemy P, Valerio N, et al. (2001) Treatment of nonmalignant obstructive iliocaval lesions by stent placement (mid-term results). Ann Vasc Surg 15: 227-232.
- Aigner F, Bodner G, Gruber H, Conrad F, Fritsch H, et al. (2006) The vascular nature of hemorrhoids. J Gastrointest Surg 10: 1044-1050.
- Kaidar-Person O, Person B, Wexner SD (2007) Hemorrhoidal disease: A comprehensive review. J Am Coll Surg 204: 102-117.
- Acheson AG, Scholefield JH (2008) Management of haemorrhoids. BMJ 336: 380-383.
- MacRae HM, McLeod RS (1995) Comparison of hemorrhoidal treatment modalities. A meta-analysis. Dis Colon Rectum 38: 687-694.
- (2004) American Gastroenterological Association medical position statement: Diagnosis and treatment of hemorrhoids. Gastroenterology 126: 1461-1462.
- Johanson JF (2002) Nonsurgical treatment of hemorrhoids. J Gastrointest Surg 6: 290-294.
- Sneider EB, Maykel JA (2010) Diagnosis and management of symptomatic hemorrhoids. Surg Clin North Am 90: 17-32.
- Testut L, Latarjet A (1977) Anatomia Humana. Tomo IV 519.
- Forauer AR, Gemmete JJ, Dasika NL, Cho KJ, Williams DM (2002) Intravascular ultrasound in the diagnosis and treatment of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol 13(5): 523-527.
- Alhalbouni S, Hingorani A, Shiferson A, Gopal K, Jung D (2012) Iliacfemoral venous stenting for lower extremity venous stasis symptoms. Ann Vasc Surg 26(2): 185-189.
- Dzieciuchowicz L, Krzyżański R, Kruszyna L, Krasinski Z, Gabriel M (2016) Prevalence of non-thrombotic Iliac Vein lesions in patients with unilateral primary varicose veins. Eur J Vasc Endovasc Surg 51(3): 429-433.






























