Complicated Case of Ogilvie’s Syndrome Following Caesarean Section
Pradeep Jayaram1, Syed Muhammad Ali2*, Ahmed Abdul Jalil2, Najah Ali2
1Sidra Medical and Research Centre, Qatar
2Hamad Medical Corporation, Qatar
Submission: June 26, 2017; Published: July 05, 2017
*Corresponding author: Syed Muhammad Ali, Department of Surgery, Hamad Medical corporation, PO Box 3050, Doha, Qatar, Tel: +97466010468; Email: ali_2051@hotmail.com;sAli35@hamad.qa
How to cite this article: Pradeep J, Syed M A, Ahmed A J, Najah A. Complicated Case of Ogilvie’s Syndrome Following Caesarean Section. Open Access J Surg. 2017; 4(5): 555649. DOI: 10.19080/OAJS.2017.04.555649
Abstract
This is a rare case of Ogilvie’s Syndrome or Acute Colonic Pseudo-Obstruction (ACPO) in a 34 year old lady following uncomplicated caesarean section. Postoperatively she developed shortness of breath and abdominal distension. X-ray and CT imaging showed free gas in the abdomen, pockets of fluid collection, pulmonary embolism and pleural effusion. Laparotomy showed a large caecal perforation and a small ileal perforation completely walled off by omentum. A hemicolectomy with ileal resection was performed with interval closure of abdomen and end-end anastomosis. A literature search in PubMed showed 66 cases of postpartum Ogilvie’s syndrome reported, since 2002. Overall mortality with Ogilvie’s syndrome with caecal perforation has been reported to be 36-45%. It should be considered as differential diagnosis in women with abdominal distension and abdominal pain following caesarean section. Clinicians should be aware of this rare diagnosis and early recognition and multidisciplinary management are critical to minimize morbidity and mortality.
Keywords: Ogilvies’ Syndrome; Acute Colonic Pseudo-Obstruction; Intestinal Pseudo-Obstruction; Postpartum
Introduction
Ogilvie’s Syndrome or Acute Colonic Pseudo-Obstruction (ACPO) is a rare condition characterized by massive dilatation of the colon in the absence of mechanical obstruction. It was first described by William Heneage Ogilvie in 1948 [1]. It is usually associated with major surgery or medical conditions such as trauma, burns, pelvic and orthopedic surgery, caesarean section, pregnancy and sepsis [2]. The importance and life threatening nature of Ogilvie’s syndrome in postpartum period was underlined by 2000-2002 triennium UK confidential enquiry report into maternal deaths, which reported four deaths due to this condition [3]. The exact incidence and the etiopathogenesis are not clear. It is rare among young patients and when it occurs, caesarean section is the commonest predisposing factor [2]. About 10% of all the cases are related Obstetrics and Gynaecological procedures. One report suggested incidence postpartum Ogilvie’s syndrome to be of 1:1500 deliveries [4]. Acute intestinal dilatation, if not treated, may lead to perforation and fecal peritonitis, and consequent morbidity and high risk of mortality.
Case Report
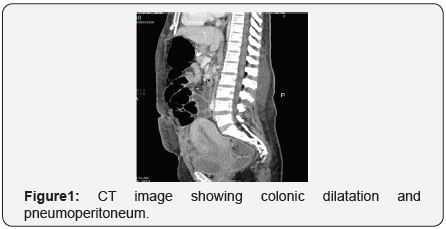
A 34 year old primigravida at 39 weeks of gestation underwent caesarean section for failure to progress. The Caesarean section was performed under spinal anesthesia and procedure was uncomplicated. Postoperatively she passed flatus and opened her bowel. On the fourth postoperative day she complained of shortness of breath and abdominal pain and distension. A CTPA (Computed Tomography, Pulmonary Artery) confirmed pulmonary embolism and abdominal x-ray showed free gas under diaphragm (Figure 1). Her finding of free air in –ray was attributed to recent Caesarean section. Her Hb was 7.5, WCC 9, CRP 148 and potassium was 2.7. Anticoagulant treatment was started. Next day her abdominal distension increased and she remained pyrexial, tachypneic and tachycardic. She also had continuous diarrhea. Further CT imaging showed significant pneumoperitoneum, pockets of fluid collection in the peritoneal cavity, but, no contrast leak was noted. Significant pleural effusion with atelectasis was also seen.
Her INR was elevated to 4 and stool culture showed campylobacter jejuni. Although, bowel perforation was suspected, as there was no contrast leak and patient was high risk for surgery a conservative approach was taken by the multidisciplinary team. She was transferred to ICU and conservative management continued with anticoagulants, antibiotics, potassium replacement, Nasogastric tube. Pleural and ascitic tap from abdominal collection under ultrasound guidance were performed for symptomatic relief. The ascitic fluid did not show any fecal contamination or blood, and cultures were negative. However, over one week patient did not show any signs of improvement and abdominal distension gradually increased. In view of these findings, a Diagnostic laparoscopy, followed by laparotomy was performed which showed a necrotic ascending colon, large caecal perforation (Figure 2) and a small ileal perforation completely sealed off by omentum.
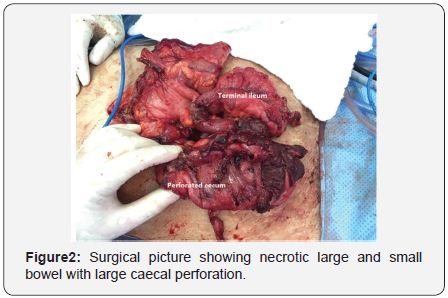
A right hemicolectomy followed by an interval of 48 hours, end-end anastomosis and closure of the abdomen was performed. Postoperative period was complicated by bleeding form anastomotic site which was managed by colonoscopic clipping of anastomotic bleeder. Patient recovered and was discharged home after 3 weeks, however she was readmitted with signs of peritonitis after 4 weeks. She underwent further laparotomy, which showed another perforation in the anastomotic site (sutured primarily) and new perforation in the ileum proximal to ileocolic anastmosis that was brought out as stoma. She recovered well and left our hospital in good general condition. Histopathology did not show any pathology apart from non-specific inflammation, ischemic and necrotic changes.
Discussion
A literature search in Pubmed, Embase and hand search of references showed 66 cases of postpartum Ogilvie’s syndrome reported, including 6 cases following vaginal delivery, since 2000- 2002 triennium confidential enquiries into maternal deaths in UK. Sixty (90%) women had caesarean section; otherwise no specific causative risk factors could be identified. Twenty eight (42%) patients had overt perforations or impending perforations with ischemic wall and serosal tears. Twenty three (82%) percent of the perforations were in the caecum and remaining were in ascending colon. Small intestinal perforations also have been reported. Fifty four percent recovered with conservative management including nil by mouth, NG tube, erythromycin, Neostigmine or colonoscopic decompression. Remaining 46% of patients required laparotomy and surgical management.
Overall mortality in patients diagnosed with Ogilvie’s syndrome and caecal perforation have been reported to be 43- 50% [5]. However, our review of recent literature specific to postpartum condition shows low mortality rates. This could be partially because our patient group is younger and usually have less comorbidity. It may partly be due to better knowledge and overall improvements in medical care. Never the less, Ogilvie’s syndrome should be considered as medical emergency and should be promptly managed with multidisciplinary input to avoid morbidity [6].
Abdominal pain and distension are the commonest symptoms. It can start as early as 24 hours or could be delayed for few days. Peritoneal signs will be absent if there is no or sealed off perforation, as was the case with our patient. It should be differentiated from simple ileus. Erect abdominal x-ray will show dilated caecum and colon and free air if there is perforation. Computed tomography also show same findings and also useful in ruling out mechanical obstruction or other coexisting pathologies [7,8]. Leaking of contrast may not be seen in impending perforations or if the perforation is sealed off completely. Therefore clinicians should not rely only on these investigations if there is suspicion of perforation.
Evidence based guidelines for management of Ogilvie’s syndrome was published by American Society for Gastro intestinal Endoscopy in 2002 [9]. According to this, in the absence of perforation a conservative management could be tried for 24-48 hours and reversible causes should be treated. If no improvement or the caecum is more than 12 cms or remains dilated for more than 3 days, IV Neostgmine is recommended. Colonoscopic decompression should be performed if there is no improvement. Surgical management should be considered if there is no improvement or suspected perforation or if there is progressive dilatation and persistence of symptoms. ACPO should be considered as differential diagnosis in women with abdominal distension and abdominal pain following Caesarean section. Prompt imaging should be arranged to look for dilatation of the caecum and presence of free gas and any evidence of mechanical obstruction. Early recognition and multidisciplinary management are critical to minimize morbidity and mortality.
Contribution of Authors
Pradeep Jayaram took the initiative, did the literature search and prepared the manuscript and was responsible for the concept and content. Syed Ali and Jalil were responsible for the surgical and postoperative report and contributed in structuring final report. Najah Ali contributed in preparing manuscript and final review of the article.
Presentation
This case report has been submitted for oral/poster presentation at Royal college of Obstetrician and Gynecologist World Congress in Cape Town, 2017.
References
- Ogilvie WH (1948) Large-intestine colic due to sympathetic deprivation.Br Med J 2: 671-673.
- Vanek VW, Al-Salti M (1986) Acute pseudo-obstruction of the colon (Ogilvie’s syndrome). An analysis of 400 cases. Dis Colon Rectum 29(3): 203-210.
- Lewis G (2004) The Confidential Enquiry into Maternal and Child Health (CEMACH). Why mothers Die, 2000-2002. The Sixth Report on Confidential Enquries into Maternal Deaths in United Kingdom. RCOG Press, London, UK.
- Reeves M, Frizelle F, Wakeman C, Parker C (2015) Acute colonic pseudo-obstruction in pregnancy. ANZ J Surg 85(10): 728-733.
- Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL (2002) Acute colonic pseudo-obstruction. Gastrointest Endosc 56(6): 789-792.
- Jain A, Vargas HD (2012) Advances and challenges in the management of acute colonic pseudo-obstruction (ogilvie syndrome). Clin Colon Rectal Surg 25(1): 37-45.
- Saunders MD (2007) Acute colonic pseudo-obstruction. Best Pract Res Clin Gastroenterol 21(4): 671-87.
- Reece EA, Petrie RH (1982) Colonic pseudo-obstruction following obstetrical surgery. A review. Diagn Gynecol Obstet 4(4): 275-280.
- Durai R (2009) Colonic pseudo-obstruction. Singapore Med J 50(3):237-244.






























