Rectusial Fascia: A New Entity of Laparoscopic Live Surgical Anatomy
Maulana Mohammed Ansari*
Department of Surgery, JN Medical College, Aligarh, India
Submission: April 07, 2017; Published: April 13, 2017
*Corresponding author: Maulana Mohammed Ansari, Department of Surgery, JN Medical College, Aligarh, India. Residence: B-27, Silver Oak Avenue, Street No. 4, Dhaurra Mafi, Aligarh, UP, India, Mobile:0091-9557449212 ; Email: mmansari.amu@gmail.com
How to cite this article: Ansari MM. Rectusial Fascia: A New Entity of Laparoscopic Live Surgical Anatomy. Open Access J Surg. 2017; 3(4): 555618. DOI: 10.19080/OAJS.2017.03.555618
Abstract
Introduction: During laparoscopic total extra-peritoneal pre peritoneal (TEPP) hernioplasty for inguinal hernia, posterior epimysium of rectus abdominis muscle was studied, and the novel observations hitherto unreported in literature are presented herein.
Materials and methods: A prospective study was conducted in adult patients of inguinal hernia who underwent Laparoscopic Total Extra-Peritoneal Pre-Peritoneal hernioplasty under the ethical clearance and informed consent. Standard 3-midline port technique was utilized. Initial access dissection in posterior rectus canal was performed with unhurried to-and-fro movements of the 0º 10-mm telescopic for careful observation of undersurface of rectus abdominis.
Results: A total of 68 hernioplasties (Unilateral 52, and Bilateral 8) was performed in 60 adult male patients with primary inguinal hernia. Mean age and BMI were 50.08±17.15 years (Range 18-80 years) and 22.58±2.03 kg/m2 (Range 19.5-31.2 Kg/m2) respectively. Epimysium on undersurface of rectus abdominis muscle was almost invariably found condensed and thickened in the form of a recognizable fascia under the excellent perspective and magnification of laparoscope, which was named as Rectusial Fascia. Rectusial fascia was found well-defined membranous/diaphanous in 88%, and it was thin/flimsy in 12%. Morphology of Rectusial fascia did not vary significantly with respect to age, BMI or occupation of individuals (p>0.05).
Conclusion: Rectusial fascia is a new entity of live surgical anatomy hitherto unreported in literature but, always appreciated by hernia surgeons during newer surgical approach of TEPP for laparoscopic inguinal hernioplasty. Usefulness of anatomic research in current laparoscopic era cannot be over emphasized because newer surgical approaches provide new vision of structures known for centuries.
Keywords: Rectusial fascia; Rectus abdominis muscle; Epimysium; Rectus abdominis fascia; Live surgical anatomy; Laparoscopic anatomy; TEPP anatomy; Inguino-abdominal anatomy; Hernia anatomy; Posterior rectus canal
Introduction
During training and teaching the procedure of the TEPP hernioplasty, it is always advised that the surgical plane should be created anterior to the posterior rectus sheath and all the same, the muscle fibers of the rectus abdominis should not be seen bare. If the muscle fibers of the rectus abdominis are seen bare in the operative field, the plane of dissection is said to be wrong. In other words, the operating laparoscopic hernia surgeon does recognize presence of a facial layer between the rectus abdominis muscle and the posterior rectus sheath regularly, and gives it a due importance with respect to the creation of the surgical plane, but he/she never bothers, nay dares, to name and describe it. This facial layer is really the posterior epimysium of the rectus abdominis muscle which has been disregarded up till now as an anatomic entity but which has recently assumed great surgical importance during the TEPP hernioplasty, and our observations are presented herein.
Materials and Methods
A prospective doctoral research for award of PhD in Surgery was designed and undertaken in the Department of Surgery, J. N. Medical College, AMU, Aligarh, UP, India-202002 from April 2010 to November 2015. The study was conducted in the adult patients (Homo sapiens) of inguinal hernia who underwent the Laparoscopic Total Extra-Peritoneal Pre-Peritoneal hernioplasty (TEPP) under the ethical clearance of our Institutional Ethics Committee and written informed consent of the patients. Inclusion criteria were patients with age equal to or more than 18 years, patients with uncomplicated fully reducible primary inguinal hernia and patients with ASA grade I – II (American Society of Anesthesiologists). Exclusion criteria were patients with age less than 18 years, patients with severe co-morbid disease (ASA grade III - V), patients with recurrent inguinal hernia, patients with complicated inguinal hernia (irreducible/ inflamed/ obstructed/ strangulated), patients with femoral hernia, patients with history of lower abdominal surgery, and patient’s refusal for laparoscopic repair.
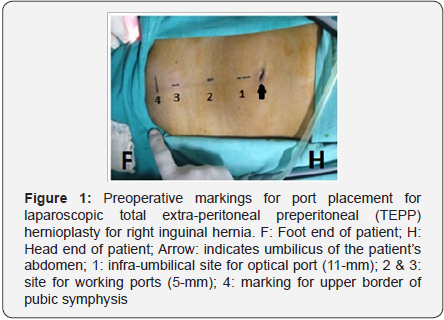
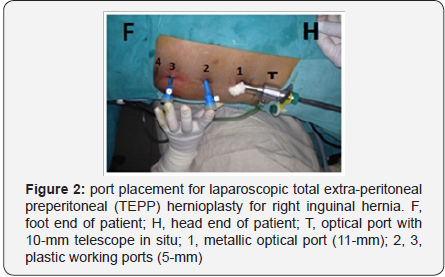
The standard 3-midline port technique of the laparoscopic TEPP hernioplasty was followed as reported earlier by the author [1] was followed. Initial access dissection in the posterior rectus canal through the infra-umbilical 11-mm optical port was carefully performed with unhurried gentle to-and-fro movements of the 0º 10-mm telescopic for proper visualization and observation of the under surface (posterior epimysium) of the rectus abdominis muscle that forms the anterior boundary of the posterior rectus canal. This was followed by placement of two 5-mm working ports in the midline lower down (Figures 1 & 2) for the definitive dissection in the preperitoneal plane of the retropubic and inguinal regions for mesh placement. SPSS version 21 was used for statistical analysis.
in the 60 patients. All patients were male (Groin hernia being uncommon in females, the three female patients with inguinal hernia presenting in the study period were not recruited for the laparoscopic hernia repair due to one or more exclusion criteria). Mean age of the patients (N=60) with inguinal hernia was 50.08±17.15 years (Range 18-80 years), and mean body mass index (BMI) was 22.58±2.03 kg/m2.
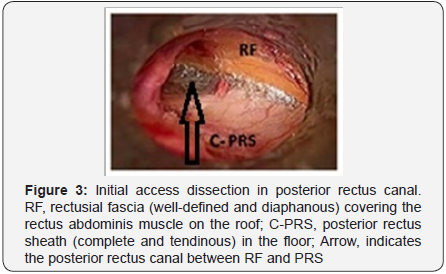
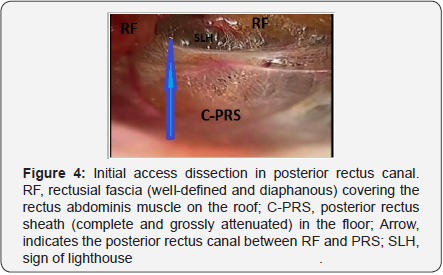
Upon entry into the posterior rectus canal and viewing with 0º 10-mm telescope (laparoscope) passed through the infra umbilical port, the canal was found always bounded anteriorly by a fascial structure covering the undersurface of the rectus abdominis muscle (and hence its fibers are not seen bare and the plane is said to be correct) and posteriorly by the posterior rectus sheath in the upper part and the transversalis fascia in the lower part if the posterior rectus sheath is incomplete. This fascial structure on the undersurface of the rectus abdominis muscle is hereafter called the ,‘Rectusial Fascia’ and abbreviated as the ‘RF or R-Fascia’ for the sake of further reference and discussion.
Results
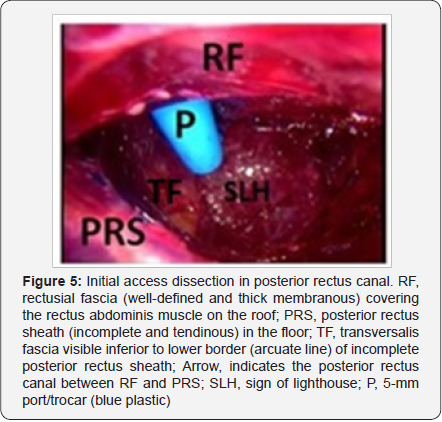
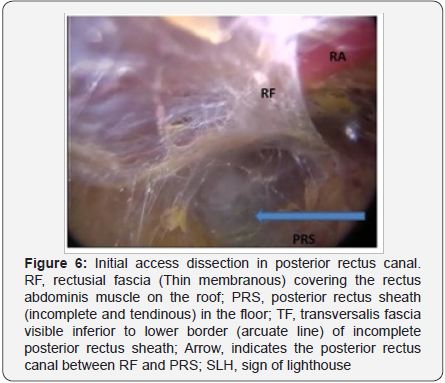
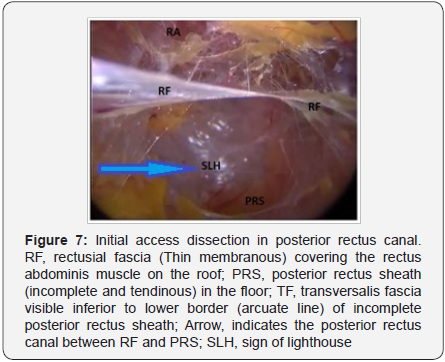
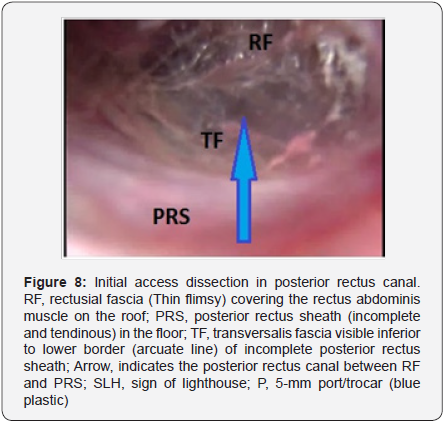
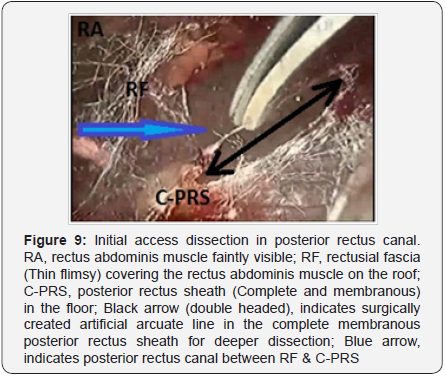
A total of 63 patients with the uncomplicated primary inguinal hernia were taken up for the TEPP hernioplasty. Three patients were excluded due to early conversion due to early peritoneal injury (1), early injury to deep inferior epigastric vessels (1), and early CO2 retention problem (1). Therefore, the present study included only 52 unilateral hernias (left side 35; right side17) and 8 bilateral hernias, and hence, the data analysis was carried for a total of 68 hernioplasty performed In the present study, this rectusial fascia was observed as a recognizable well-defined fascial structure in 60 out of 68 cases (88.24%) – thick diaphanous (Figure 3) & (Figure 4) in 47 cases (69.1%) and thick membranous (Figure 5) in 13 cases (19.1%); and it was thin in nature in 8 cases (11.76%) – thin membranous (Figure 6) & (Figure 7) in 3 cases (4.4%) and thin flimsy (Figure 8) & (Figure 9) in 5 cases (7.4%). In all cases, the deep inferior epi gastric vessels (DIEV) were found lying within this rectusial fascia on the undersurface of the rectus abdominis muscle. In patients with incomplete posterior rectus sheath (PRS), the DIEV was present within the rectusial fascia above the arcuate line. In patients with the complete PRS [1], the DIEV appeared to course within the rectusial fascia running upwards from just above the symphysis pubis.
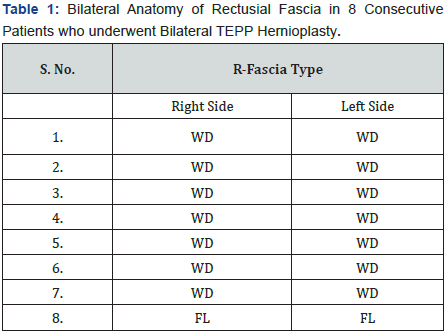
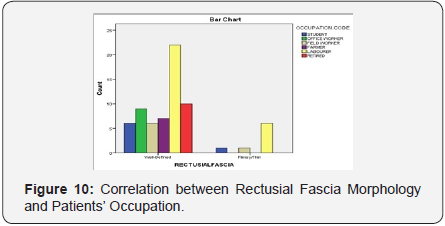
There was no significant de (p >0.05) between the mean age and BMI of the patients between the two groups (WD and FL) of the R-Fascia. Similarly, there was no significant correlation between the 2 subtypes of R-Fascia and the nature of patients’ work in the present study (Pearson Chi-Square Correlation, R = 6.071, df 5, Sig. 0.299, p >0.05) (Figure 10). In patients with the bilateral hernia (N=8), the anatomy of the rectusial fascia was mirror image on the two sides of the body all cases (WD vs. WD in 7; FL vs. FL in 1) (Table 1).
Discussion
It is ironical that during laparoscopic learning and training for TEPP, if the fibers of the rectus muscle are seen bare, the plane of dissection is said to be wrong, and the operating hernia surgeon is always advised to remain under a facial structure covering the undersurface of the rectus abdominis muscle, i.e., the laparoscopic hernia surgeons always consciously recognize this facial structure during the TEPP hernioplasty, but no study is reported in the surgical or anatomical literature on this nowimportant fascia, which is herein termed as the Rectusial Fascia by the author for further reference and discussion.
Rectus abdominis is a paired muscle of the anterior abdominal wall running vertically from the costal margins to the pelvic bones, one on each side of the lineal alba in the anterior midline. Superiorly, rectus abdominis usually arises from the 5th to 7th costal cartilages, and often from the anterior part of the 5th rib also [2,3]. Medial border of the rectus abuts and often fused with the Linea Alba. Inferiorly, rectus abdominis is inserted through two tendons. Smaller medial tendon decussates with the opposite one and inserts on the anterior surface of the symphysis pubis. Larger lateral tendon is inserted on the pubic crest and sometimes on the pectineal line also. Lateral border is usually visible on abdominal surface as a groove, running from the tip of the 9th costal cartilage to the pubic tubercle, which is called the linea semilunaris [2,3].
The two rectus muscles are in contact with each other above the pubic symphysis because inferiorly, the Linea Alba is very narrow and posterior rectus sheath is typically absent. The anterior rectus sheath is firmly attached to the rectus abdominis while the posterior rectus sheath is not [2-4]. Usually the muscle has three tendinous intersections: one at the xiphisternum, one at the umbilicus, and one between these two. However, one or two incomplete intersections are sometimes present below the umbilicus. The tendinous intersections blend inseparably with the anterior rectus sheath [5]. These intersections contain multiple perforators from the epi gastric vessels, which supply the overlying anterior rectus sheath, fascia and soft tissue [6]. The perforators are most dense in peri umbilical areas. As the intersections lie superficially in the muscle and do not penetrate to its posterior surface, the rectus is not adherent/ attached to the posterior rectus sheath, and therefore, it is possible to insert the telescope easily into this retro-muscular space, often called the posterior rectus canal, during the laparoscopic total extra peritoneal pre-peritoneal (TEPP) hernioplasty.
Deep inferior epigastric and superior epigastric vessels are the main vascular supply of the rectus [2,3]. It also receives small terminal branches of the lower 3 posterior inter costal arteries, sub costal artery, lumbar arteries and the deep circumflex artery, which anastomose with lateral branches of the epi gastric arteries. The deep inferior epigastric artery arises from the external iliac artery at the level of inguinal ligament and passes upwards and medially. It then slips over the arcuate line and runs within the variably thickened epimysium (Rectusial fascia) on the undersurface of the rectus abdominis muscle. The veins, usually two, accompany the artery and drain into the external iliac vein.
The epimysium is a fascia that covers the surface of a muscle, and depending on the muscle, it can be thin band or thick opaque [7]. The connective tissue fibres of the epimysium vary from areolar to thick bands of fibrous tissue [8]. Epimysium is thicker than the other elements (peri- and endomysium) of the intramuscular tissue, and it is formed by large-diameter collagen fibers [9]. Near the origin and insertion of the muscle, the epimysium thickens before it merges with the tendons and converges in the paratenon, while in the area of the muscle belly; it forms a thin layer [10,11]. During pre-peritoneal laparoscopy, the epimysium of the rectus abdominis is clearly seen in a similar fashion of variable proportions, and it usually forms a recognizable fascia, and the operating hernia surgeon is always advised to remain under this fascia during TEP approach, because if the fibres of the rectus muscle are seen, the plane of dissection is said to be incorrect. In the present laparoscopic study of live surgical anatomy, a clearly recognizable substantial Rectusial fascia was documented in all 68 cases of the TEPP hernioplasties performed successfully, and its nature varied from well-defined membranous/diaphanous (88%) to thin/flimsy (12%). The Rectusial fascia anatomy did not vary with respect to the age, weight/BMI or occupation of the patients.
In view of the facts that the groin hernia is of the commonest operations in general surgery and that the groin hernia occurs in both sexes albeit rarely in females, the present study has two limitations, viz., firstly, the sample size is rather small, and absence of female patients in the our study.
Conclusion
Rectusial fascia is a new entity of live surgical anatomy hitherto unreported in literature, but always appreciated by the hernia surgeons during the newer surgical approach of TEPP for laparoscopic inguinal hernioplasty. Morphology of the rectusial fascia varied from thick well-defined to thin flimsy independent of the age, BMI and occupation of the individuals. Presence of the Rectusial fascia observed regularly during the pre-peritoneal laparoscopy strongly supports the observation and recommendation of Avisse et al [12] that the newer surgical approaches provide ‘new vision of structures known for centuries’ and ‘so, anatomic research is still useful’.
References
- Ansari MM (2013) Effective Rectus Sheath Canal: Does It Affect TEP Approach for Inguinal Mesh Hernioplasty. J Exp Integr Med 3(1): 73- 76.
- Williams PL, Bannister L, Berry M, Collins P, Dyson M, et al. (1998) Gray’s Anatomy. 38th ed. London: Churchill Livingstone, pp. 551-559.
- Sinnatamby C (2000) Last’s anatomy, 10th edn, Churchill-Livingstone, Edinburg, USA, pp. 218-219.
- Mwachaka P, Odula P, Awori K, Kaisha W (2009) Variations in the Pattern of Formation of the Abdominis Rectus Muscle Sheath among Kenyans. Int J Morphol 27(4): 1025-1029.
- Sinnatamby CS (2011) Last’s Anatomy: Regional and Applied, (12th edn), Chapter 5, Edinburgh: Churchill-Livingstone-Elsevier, pp. 221- 325.
- Whetzel TP, Huang V (1996) The vascular anatomy of the tendinous intersections of the rectus abdominis muscle. Plast Reconstr Surg 98(1): 83-89.
- Rodriguez H, Espinoza-Navarro O, Silva I, Quiroz P, Arriaza C, et al. (2011) Histological Description of the Interaction Between Muscle Fibers and Connective Tissue of the Fascia of the Human Trapezius Muscle. Int J Morphol 29(1): 299-303.
- Rosen E, Bailey B, Quinn F, Ryan M (2002) Deep neck spaces and infections.
- Sakamoto Y (1996) Histological features of endomysium, perimysium and epimysium in rat lateral pterygoid muscle. J Morphol 227(1): 113- 119.
- Benjamin M (2009) The fascia of the limbs and back--a review. J Anat 214(1): 1-18.
- Marchuk C, Stecco C (2015) The role of connective tissue in the embryology of the musculoskeletal system: towards a paradigm shift. F1000Research 4: 635.
- Avisse C, Delattre JF, Flament JB (2000) The inguinofemoral area from a laparoscopic standpoint. History, anatomy, and surgical applications. Surg Clin North Am 80(1): 35-48.






























