Extraorbital Giant Cell Angiofibroma of the Right Inguinal Region: A Case Report
Badria MA Ali1, Mohammad Feras Shalabi2, Valentina Giaccaglia3 and Mohammad Azfar1*
1Department of General Surgery, Madinat Zayed Hospital, Madinat Zayed WR, UAE
2Department of General Surgery Unit, Sant’ Andrea Hospital, Sapienza University of Rome, Italy
Submission: December 12, 2016; Published: December 19, 2016
*Corresponding author: Mohammad Azfar, Consultant Surgeon, Department of General Surgery, Madinat Zayed Hospital, Post Box 50018, Madinat Zayed WR, Abu Dhabi, UAE.
How to cite this article: Badria M A, Mohammad F S, Valentina G, Mohammad A. Extraorbital Giant Cell Angiofibroma of the Right Inguinal Region: A Case Report. Open Access J Surg. 2016; 1(5): 555575. DOI: 10.19080/OAJS.2016.01.555575
Abstract
Giant cell angiofibroma (GCA) is a benign mesenchymal tumor originally described in the orbital region. More and more extraorbital GCA is being reported. Herein, we describe an extraorbital GCA in the right inguinal region clinically and radiologically mimicking irreducible inguinal hernia.
Keywords: Giant cell angiofibroma; Orbital; Extraorbital; Inguinal
Introduction
Giant cell angiofibroma (GCA) is a rare mesenchymal neoplasm, most commonly arising in the soft tissues near the orbit. Recently, several cases of extraorbital GCA have been reported, including submandibular, parascapular region and posterior mediastinum [1-3]. GCA is a distinctive tumor that was originally described in 1995 by Dei Tos et al. [1,4] who reported seven cases of this unusual tumor involving the soft tissue of the orbit. Until 2014 twenty six cases of extraorbital GCA were reported, out of which only three cases were of groin and inguinal region [5]. We have come across a case of an extraorbital GCA of right inguinal canal in a young patient of varicose vein of lower extremity.
Case Report
A 24-year-old male patient presented to surgical services for evaluation of varicose vein of left lower extremity of one year duration. He also complained of painless mass in right inguinal region, progressively increasing in size. Clinical examination of the patient was consistent with the diagnosis of irreducible right inguinal hernia. Ultrasound of scrotum and right inguinal region showed a homogenous mass of 8 x 4 cm extending till right scrotal neck, a picture likely of omental herniation. His general physical examination was unremarkable. His routine laboratories were also normal. On surgical exploration, soft tissue mass was found deep to external oblique muscle and anterior adherent to the spermatic cord. Further exploration of the inguinal canal did not reveal the presence of direct or indirect inguinal hernia.
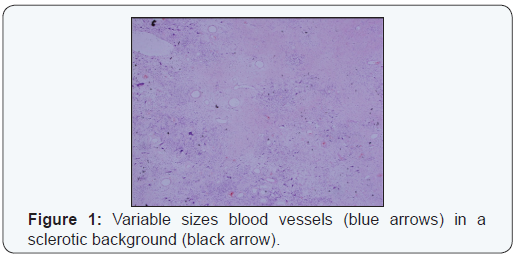
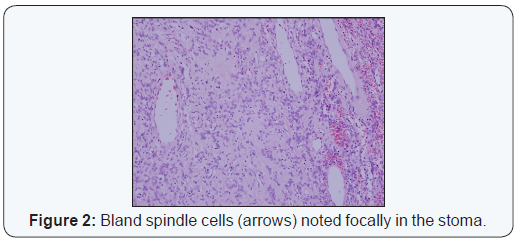
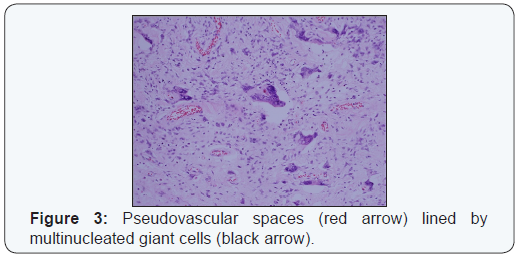
Histopathology of the excised specimen showed tumorous proliferation of variable cellularity with apparent well circumscription at the edge composed of spindle shaped and round cells intermingled in a collagenous, myxoid and sclerotic stroma associated with prominent medium and large sized vessels showing occasional perivascular hyalinization. Scattered multinucleated giant cells and pseudovascular spaces lined by multinucleated giant cells were also identified (Figures 1-3). Immunohistochemical stains for CD31, CD34, CD99, CD68, BCL 2, smooth muscle actin, desmin, S100 and CK AE1/AE3 were performed with adequate controls. The tumor was diffusely and strongly positive for CD34, BCL 2 and variably positive for CD99. CD68 showed weak occasional positivity. CD31, SMA, desmin, S100 and CK AE1/AE3 were negative. The combination of morphological and immunophenotypic findings are in favor of GCA. On his recent follow up, after 4 years, he is in perfect health without any evidence of local recurrence.
Discussion
Giant cell angiofibroma (GCA) was first described in 1995 by Dei Tos et al. [4,6] as a distinctive orbital tumor occurring in adult males. However, this tumor can occur in diverse extraorbital locations such as submandibular, parascapular, retroauricular, thigh, mediastinum, back scalp, retroperitoneum, vulva, hip, forearm, groin, parotid, neck, and oral cavity [7-10]. Interestingly the extra-orbital lesions predominantly affect women, corresponding to 66% of cases [6]. GCA is a benign mesenchymal slow growing lesion showing histological features intermediate between but distinct from solitary fibrous tumor and giant cell fibroblastoma [6]. GCA’s are well circumscribed variably encapsulated small lesions. Extraorbital tumors tend to be larger than orbital tumors. Hemorrhagic and cystic changes may be observed on cut sections [10]. Treatment of GCA consists of simple tumorectomy. Although benign in nature, it has the potential for local recurrence especially after incomplete resection [4,8].
Diagnosis of GCA is usually made after resection and immunohistochemical analysis. Histopathological characteristics of GCA includes the presence of homogenous irregularly organized proliferating cells that are round or oval in shape, collagenous and myxoid stromal region, richly vascularized tumor containing pseudovascular spaces in the presence of interstitial hemorrhage. The pseudovascular spaces are lined by multinucleated giant cells [5,7]. The immunohistochemical features of GCA includes positive staining for CD34, CD99, vimentin, variable BCL2 and negative staining for CD31, SMA, desmin, S100 and CK AE1/AE3. In the present case, positive staining for CD34 along with the presence of giant cells and pseudovascular spaces confirmed the diagnosis of GCA. Sonobe et al. [5] detected first abnormalities of chromosome 6 with a common pattern 6q13 together with other chromosomal abnormality in a typical case of GCA. Qian et al. [9] reported a case of GCA in the neck whose chromosome analysis showed karyotype with t (12;17) (q15;q23), del (18) (q21) in all 20 cells analysis. This being the second case of GCA with chromosomal aberration and first case of GCA with t (12;17) occurring as extraorbital mass. The cytogenic abnormality in GCA is different from the t (17;22) (q22; q13) found in related lesion, such as giant cell fibroblastoma and solitary fibrous tumor, none of which have a specific chromosomal abnormality [10]. Unfortunately, we were not in a position to do the cytogenetic testing in this case.
Conclusion
GCA is a benign mesenchymal tumor of the head and neck region. However, extraorbital cases have been reported in diverse locations. Preoperative diagnosis is rarely made and surgery remains the main treatment. Diagnosis is confirmed only by histopathology and immunohistochemical analysis of the resected tumor to identify multinucleated giant cells and pseudovascular spaces along with positivity of CD34, vimentin and BCL2 as in the case presented.
Acknowledgement
The authors are highly indebted and thankful to Mr. Mohammed Mudassir Anwar Ali for his secretarial assistance in preparation of this article.
References
- Sigel JE, Fisher C, Vogt D, Goldblum R (2000) Giant cell angiofibroma of the inguinal region. Ann of Diagn Pathol 4(4): 240-244.
- Mikami Y, Shimizu M, Hirokawa M, Manabe T (1997) Extraorbital giant cell angiofibromas. Mod Pathol 10(11): 1082-1087.
- Fukunaga M, Ushigome S (1998) Giant cell angiofibroma of the mediastinum. Histopathology 32(2): 187-189.
- Dei Tos AP, Seregard S, Calonje E, Chan JK, Fletcher CD (1995) Giant cell angiofibroma. A distinctive orbital tumor in adults. Am J Surg Pathol 19(11): 1286-1293.
- He Y, Zhang C, Liu G, Tian Z, Wang L, Kalfarentzos E (2014) Giant cell angiofibroma misdiagnosed as a vascular malformation and treated with absolute alcohol for one year: A case report and review of the literature. World J Surg Oncol 12: 117.
- De Andrade CR, Lopes MA, de Almeida OP, León JE, Mistro F, Kignel S (2008) Giant cell angiofibroma of the oral cavity: A case report and review of literature. Med Oral Patol Oral Cir Bucal 13(9): 540-543.
- Thomas R, Banerjee SS, Eyden BP, Shanks JH, Bisset DL, et al. (2001) A study of extraorbital giant cell angiofibroma with documentation of some unusual features. Histopathology 39(4): 390-396.
- Husek K, Veselý K (2002) Extraorbital giant cell angiofibroma. Cesk Patol 38(3): 117-120.
- You-Wen Qiana, Rajit Malliaha, Huey-Jen Leeb, Kasturi Dasa, Neena Mirania (2006) A t(12;17) in an extraorbital giant cell angiofibroma. Cancer Genetics and Cytogenetics 165(2): 157-160.
- Pala EE, Beyhan R, Bayol U, Cumurcu S, Kucuk U (2012) Giant cell angiofibroma in unusual localization: a case report. Case Rep Pathol 10: 1-4.






























