An Unexpected Operative Finding of Intracerebral Pus in a Case of Multifocal Cerebral Metastases from Small Cell Lung Cancer
Ibiwari Pepple* and Debasish Hajra
Department of Neurosurgery, University Hospital Coventry and Warwickshire, United Kingdom
Submission: September 20, 2019; Published: November 01, 2019
*Corresponding author: Ibiwari Pepple, Department of Neurosurgery, University Hospital Coventry and Warwickshire, Coventry, West Midlands, United Kingdom
How to cite this article: Ibiwari Pepple, Debasish Hajra. An Unexpected Operative Finding of Intracerebral Pus in a Case of Multifocal Cerebral Metastases from Small Cell Lung Cancer. Open Access J Neurol Neurosurg. 2019; 11(5): 555825. DOI: 10.19080/OAJNN.2019.11.555825.
Abstract
Background: Small Cell Lung Cancer (SCLC) accounts for 10-20% of all lung cancers and is characterized by early and rapid spread. Ten percent of patients already have cerebral metastases at time of presentation.
Case Description: We report a case of a 37yr old female whose pre-operative CT and MRI brain revealed multicentric left frontal and temporal lesions which mimicked intracerebral abscess intraoperatively and confirmed on gram stain as moderate growth of white cells. The patient was commenced on prolonged antimicrobial therapy postoperatively, however, histology reported SCLC metastases with lung as primary and patient was eventually commenced on chemotherapy.
Conclusion: The prevalence of intraoperative histopathological frozen section to better support diagnosis and good understanding of SCLC cerebral metastases from accumulation of cases together with modern diagnostic tools will hopefully lead to prompt and adequate therapeutic options for patients.
Keywords: Antimicrobial therapy Cerebral abscess Multifocal cerebral metastasis Small cell Lung cancer Non-enhanced Contrast enhanced magnetic Abdomen Multidisciplinary team Weighted imaging Diffusion coefficient
Abbrevations: NECT: Non-Enhanced Computed Tomography; CEMRI: Contrast Enhanced Magnetic Resonance Imaging; CAP: Chest, Abdomen and Pelvis; MDT: Multidisciplinary Team; DWI: Diffusion Weighted Imaging; ADC: Apparent Diffusion Coefficient; SWI: Susceptibility Weighted Imaging
Introduction
Lung cancer is undoubtedly the most common cause of cancer related deaths in the United Kingdom and worldwide for both men and women, accounting for one-fifth of all cancer deaths. Forty percent of patients with lung cancer have brain metastases (highest amongst all malignant tumors), of which 48% have single metastasis and 52% multiple of multifocal.
SCLC account for 10-20% of all lung cancers. Histologically, it is the third most common subtype but has the highest malignant potential. And it has been reported that at time of initial admission, approximately 10% of all SCLC patients have cerebral metastases. Several papers have reported as high as 80-90% of supratentorial metastases from SCLC of which 60-70% have multiple characteristics SCLC spread early via intrathoracic and mediastinal lymph nodes to brain, liver, bone etc. Clinically, patients will complain of headache, vomiting, sensorimotor deficits, seizures, behavioral problems and aphasia. However, these symptoms can be subtle resulting in late hospital presentation.
Case Report
LA 37-year-old female who spoke little or no English presented with 2wks history of headache, blurry vision, slurred speech, dizziness, confusion but no sensorimotor deficits. She had no significant medical history prior to her hospital admission and socially she confirmed that she is a regular smoker. A Non-Enhanced Computed Tomography (NECT) of the head (Figure 1) showed large hypodense mass (5x6cm) in the left frontal lobe with hyperdense margin crossing midline and compressing the frontal horn of left lateral ventricle. Our differential diagnosis centered around glial based tumor with very little possibility of an abscess based on imaging features. She had routine bloods which showed a white cell of 94,300/mm3, Hb of 150g/L, normal BUN and electrolyte level. Patient was also commenced on highdose dexamethasone and levetiracetam for intracerebral edema and seizure prophylaxis

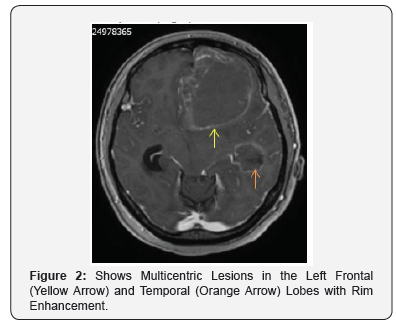
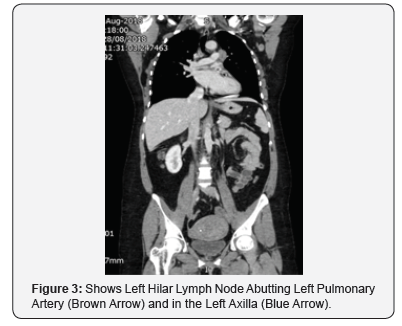
As per our unit protocol, she underwent Contrast Enhanced Magnetic Resonance Imaging (CE-MRI) of brain inclusive of stereotactic planning sequence (Figure 2), CT chest, abdomen and pelvis (Figure 3). MRI was reported as multicentric lesion likely primary glioma and metastatic deposits as possible differentials, but unlikely to be an abscess due to lack of diffusion restriction in the center of the lesions. CT Chest, Abdomen and Pelvis (CAP) found incidental left hilar and axillary adenopathy for which guided biopsy was advised but was not followed up on at this point. The case was discussed in the neuro-oncology Multidisciplinary Team (MDT) meeting and it was recommended that she undergo tumor debulking [1].
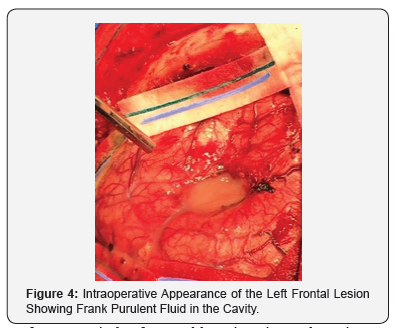
Intraoperatively after stealth registration and craniotomy, cortectomy done directly above the lesion revealed yellowish fluid suggestive of frank pus gushing out of the suspected tumor cavity (Figure 4). Samples were immediately sent to the laboratory for urgent microscopy, culture and sensitivity. A portion of the presumed abscess cavity wall was also sent for histology. It is important to mention that the temporal lobe lesion was not interfered with during surgery. She was commenced on intravenous meropenem intraoperatively as empirical treatment based on intraoperative findings During her recovery, further investigations in the form of echocardiogram, OPG x-ray to look for potential source was carried out. These investigations did not reveal the source of the abscess and though microscopy of the purulent fluid showed moderate growth of white blood cells, no organisms were isolated on culture [2].
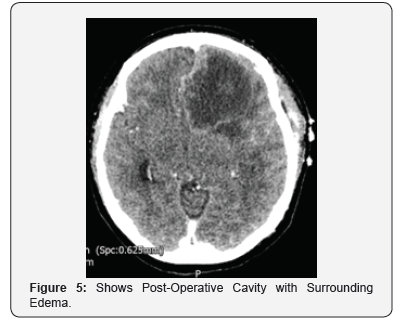
Her post-operative contrast enhanced CT showed reduction in size of the lesion (Figure 5). However, the recovery period was complicated by few episodes of seizures and CT venogram confirmed left transverse sinus thrombosis, both of which were adequately treated. Based on the intraoperative findings, we had somewhat agreed that this is likely an intracerebral cerebral abscess of unknown source for which antibiotics was started following standard guidelines. However, the histology was positive for metastatic small cell carcinoma andImmunohistochemistry favored a primary in the lung. In the view of the histology report, patient was referred to the lung MDT for further discussion and management [3].
Discussion
MRI is the modality of choice for differentiating brain metastases from brain abscess and glioblastoma. On Diffusion Weighted Imaging (DWI) the central area of an abscess is hyperintense due to high viscosity which differentiates it from brain tumors. A recent report by Fink et al. [4]. indicated that brain metastases tend to show high Apparent Diffusion Coefficient (ADC) values while DWI will distinguish between metastases and abscess with high diffusion restriction. This was in contrast to an earlier study by Duygulu et al. [5]. in which reported that increased diffusion restriction for both metastatic SCLC and NSCLC. Even with large studies on lung cancer brain metastases, there are no established trends in MRI manifestations as compared to metastases from other regions (melanoma, kidney and colon) that MRI pathognomonic findings have been reported. In this case and due to the ambiguity as highlighted in the studies above, the intraoperative findings where very much in keeping with intracerebral pus collection (Figure 4) cascading into sample collection for culture and sensitivity, with post-operative antimicrobial therapy.
Retrospectively, maybe the use of additional MR sequences like Susceptibility Weighted Imaging (SWI), proton magneticresonance spectroscopy (1H-MRS), whole body diffusion weighted MRI (DW-MRI) or an additional modality like Positron Emission Tomography (PET) would have changed the approach of giving postoperative antibiotics in this case. Also, the CT CAP which revealed hilar and mediastinal adenopathy could have been biopsied to attain a diagnosis and potentially prevent antibiotic use. However, we need to stress that that the patient was already symptomatic from the mass effect of the lesion which is the main reason operative intervention was pursued as a matter of urgency and one which yielded good post-operative improvement in neurological deficit.
Conclusion
This case report has highlighted an unexpected intraoperative finding of intracerebral pus in multifocal SCLC cerebral metastasis which convinced the surgical team to pursue the use of antimicrobial therapy and to further investigate the source of the abscess only for histopathological examination to confirm the diagnosis as metastatic SCLC. We would like to suggest a robust use of available investigatory armamentarium to clearly differentiate cerebral abscess from metastasis when dealing with ambiguous cases. Secondly, emphasis has to be placed on the importance of frozen section diagnosis which our team believe should be made widely available in other to assist with intraoperative diagnosis and prevent exposing patients to extra investigations and treatment as in this case.
References
- Auchter RM, Lamond JP, Alexander E, Buatti JM, Chappell R, et al. (1996) A multiinstitutional outcome and prognostic factor analysis of radiosurgery for resecta
- Dolgushin, Mikhail, Kornienko, Valery, Pronin (2018) Brain Metastases: Advanced Neuroimaging
- Saito T, Ujiie H, Kadoyama S, Higa T, Shiono S, et al. (2015) Brain metastasis from a lung mucoepidermoid carcinoma mimicking a brain abscess. Surg Neurol Int 6(Suppl 9): S300-303.
- Fink KR, Fink JR (2013) Imaging of brain metastases. Surg Neurol Int 4(Suppl 4): S209‑219
- Duygulu G, Ovali GY, Calli C, Kitis O, Yunten N, et al. (2010) Intracerebral metastasis showing restricted diffusion: Correlation with histopathologic findings. Eur J Radiol 74(1): 117‑120






























