A Case of Bilateral Opercular Stroke Presenting as Foix-Chavany-Marie syndrome: a 6-Month Follow-Up, Supplemented with a Physical Examination Video
Donohoe Charles1, Gratton Sean1, Finn Margaret1*, Lodhi Hafsa1 and Siddiqui Waquar1,2
1University of Missouri, USA
2Center for Behavioral Medicine, USA
Submission: May 24, 2017; Published: June 26, 2017
*Corresponding author: Waquar Siddiqui, MD, Center for Behavioral Medicine, 1000 East 24th Street, Kansas City, Missouri 64108, Tel: (816]-512-7000; Email: siddiquiw@umkc.edu
Margaret Finn, BA, University of Missouri-Kansas City, 2411 Holmes Street, Kansas City, MO 64108, Tel: (816)-304-4485;Email: mmf2p4@mail.umkc.edu
How to cite this article: Donohoe C, Gratton S, Finn M, Lodhi H, Siddiqui W. A Case of Bilateral Opercular Stroke Presenting as Foix-Chavany-Marie syndrome: a 6-Month Follow-Up, Supplemented with a Physical Examination Video. Open Access J Neurol Neurosurg. 2017; 4(3): 555638. DOI: 10.19080/OAJNN.2017.04.555638
Abstract
Foix-Chavany-Marie syndrome is a rare disorder due to bilateral damage of the operculum most commonly secondary to stroke. Classically the patient presentation is alert and cognitively intact, but unable to voluntarily speak or swallow and is accompanied by preservation of automatic movements such as yawning or smiling. We report a case of a 38-year-old African American male with history of left middle cerebral artery infarction that presents with sudden inability to open his mouth or perform any oral motion upon command, although can execute automatic movements such as yawning. The patient exhibited FCMS with classic clinical symptoms due to the most common vascular etiology. This is accompanied by confirmatory magnetic resonance evidence revealing an old infarct in the left frontal operculum with multiple new ischemic foci in the right operculum.
Keywords: Bilateral opercular stroke; Foix-chavany-marie syndrome; FCMS; Cortical pseudobulbar paralysis; Bilateral stroke
Abbreviations: FCMS: Foix-Chavany-Marie Syndrome; MCA: Middle Cerebral Artery; DWI: Diffusion-Weighted Imaging; ALS: Amyotrophic Lateral Sclerosis
Introduction
Foix-Chavany-Marie syndrome (FCMS) is a rare disorder due to bilateral damage of the operculum most commonly secondary to stroke, with even rarer cases presenting after a unilateral stroke. Encephalitis, seizures, CNS infections, developmental and degenerative disorders, and head trauma are far less frequently encountered as primary insults [1]. The clinical presentation though stereotyped, if not previously encountered, can pose a diagnostic challenge. Classically the patient presentation is alert and cognitively intact, but unable to voluntarily speak or swallow and is accompanied by preservation of automatic movements such as yawning and smiling [1-3]. We report a case of FCMS with classic clinical symptoms due to the most common vascular etiology with confirmatory magnetic resonance (MR) evidence of acute infarction superimposed upon chronic infarction of both opercular regions.
Case Presentation
A 38-year-old African American diabetic male with a history of left middle cerebral artery (MCA) infarctionsix years ago resulting in residual right-sided weakness, presented to the emergency department with sudden inability to open his mouth, speak or swallow. Neurology was consulted for possible botulism. On examination, the patient was unable to open his mouth, close his eyes, swallow or stick out his tongue upon command, yet automatic movements such as yawning and smiling remained intact. Comprehension was preserved and handwritten or hand signal responses to mental status questioning were unremarkable. The patient denied any oral pharyngeal pain or recent infection and, other than a mild chronic right hemiparesis, the remainder of his neurological examination including ocular motor examination and pupillary reflexes was intact.
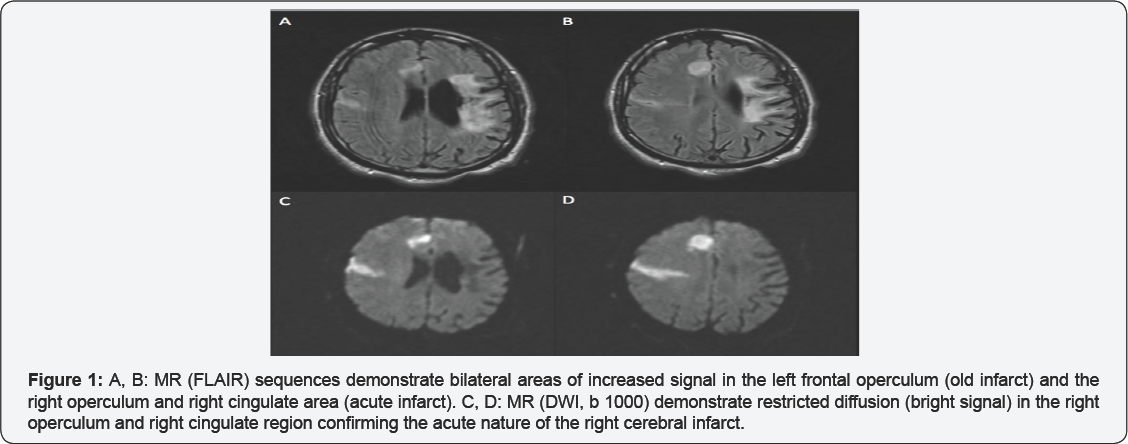
MR of the brain with diffusion-weighted imaging (DWI) was performed sixteen hours after onset of symptoms (Figure 1). This examination clearly demonstrated both the old infarct in the left frontal operculum and multiple new ischemic foci in the right operculum and right cingulate area demonstrated by restricted diffusion characteristic of acute infarction.
The patient received anticoagulant therapy (enoxaparin), antiarrhythmic agents (digoxin, metoprolol), statin (rosuvastatin), angiotensin-converting enzyme inhibitor (perindopril), and insulin. A nasogastric feeding tube was placed due to dysphagia and to prevent aspiration pneumonia. The patient communicated by writing and using hand signals while undergoing speech therapy. Prolonged EKG monitoring revealed no evidence of atrial fibrillation. Underlying multiple stroke risk factors including cigarette smoking, hypertension and hyperlipidemia were addressed. After 3 weeks, he was discharged to a skilled nursing facility, still unable to smile, swallow or speak. The patient was seen in the clinic on regular follow-up visits and despite 6 months of intensive rehabilitation, the patient continued to require percutaneous endoscopic gastrostomyfor nutrition and regained no volitional control of the oral, pharyngeal or facial musculature.
Discussion
FCMS, or bilateral anterior opercular syndrome, is a rare disorder that can escape recognition clinically. Comprehension remains intact without pathologic laughter or crying. Recognition of the dissociation between absent voluntary movements of the bulbar muscles (speech and swallowing) from preserved automatic movements (yawning and smiling) are key to prompt recognition of FCMS [3,4].
FCMS is a rare variant of cortical pseudobulbar paralysis caused by bilateral lesions in the anterior operculum [3]. Initially described by Magnus in 1837, it was ultimately named after the French authors (Foix-Chavany-Marie) who described it more extensively in 1926 [1-3]. Most often the etiology is vascular with a sudden acute presentation due to bilateral sequential rather than simultaneous infarcts of the anterior operculum. Stroke is by far the most common cause of FCMS but it is also less commonly seen in bilateral opercular lesions associated with demyelinating disease like multiple sclerosis, vasculitis, acute disseminated encephalomyelitis, and head trauma.
Differential diagnostic considerations in evaluating bulbar muscle dysfunction include botulism, brain stem infarction (lateral medullary syndrome), myasthenia gravis and motor neuron disease, and amyotrophic lateral sclerosis (ALS). However, the dysarthria and dysphagia associated with ALS do not have a sudden onset, while botulism and myasthenia gravis disrupt the neuromuscular junction and exhibit preferential involvement of the oculomotor nerves with diplopia and, in the case of botulism, pupillary dilatation. Brainstem strokes including lateral medullary syndrome (Wallenberg) due to vertebral or posterior inferior cerebellar artery occlusion exhibit additional symptoms such as ataxia, nystagmus and contralateral loss of pain and temperature sensation.
A core clinical feature that distinguishes cortical pseudobulbar palsy (FCMS) from subcortical pseudobulbar palsy is the dissociation of automatic and voluntary movements of the bulbar movements [1,3]. Voluntary control of the facial, masticatory, pharyngeal and lingual muscles is provided by the primary motor cortex and its projections to the corresponding cranial nerve nuclei. An alternative pathway serving emotional or automatic control of these muscles originates from the amygdala and lateral hypothalamus and is spared in the face of damage to the anterior operculum. Also, FCMS is not associated with the pathologic emotional lability or exaggerated gag reflex seen with subcortical pseudobulbar palsy.
A brain MR is the diagnostic modality of choice but the prognosis of the most common variant of FCMS due to stroke is generally poor [1]. Management often requires a multidisciplinary therapeutic approach and commonly the patient requires PEG tube feeding and neuro-rehabilitation that proceeds without complete recovery of speech and swallowing.
In conclusion, when initially encountering a patient with FCMS, the diagnosis can be puzzling. Identification of the dissociation between voluntary movements of the bulbar muscles (speech and swallowing) which are absent from preserved automatic movements (yawning and smiling) are key to prompt recognition.MR rather than computed tomography (CT) is the modality of choice in identification of the most common etiology, bilateral sequential, rather than simultaneous opercular infarcts. Repeat MR brain imaging 48 hours after the initial presentation can be helpful in difficult cases.
Our patient continued to require PEG tube feeding and even after six months of speech therapy remained anarthric. In general, most patients with FCMS have a poor functional recovery. Rare cases described with unilateral ischemic lesions of the operculum or patients with bilateral lesions due to epileptiform, vasculitic or demyelinating (multiple sclerosis) pathology tend to have a better prognosis [5] (Video).

References
- Milanlioglu A, Aydin MN, Gokgul A, Hamamci M, Erkuzu MA, et al. (2013) Ischemic bilateral opercular syndrome. Case Reports in Medicine 2013: 1-3.
- Kozak HH, Uca AU, Dundar MA (2015) Foix-chavany-marie syndrome after an isolated pontine infarct: A 7-year follow-up. Neurology India 63(6): 983-985.
- Bursaw A, Duginski T (2011) Anterior opercular syndrome caused by acute, simultaneous, isolated bilateral infarcts. Arch Neurol 68(2): 254-255.
- Karaca S, Goksel BK, Tan M, Alkan 0 (2013) Foix-Chavany-Marie syndrome due to cerebral infarctions with relatively good recovery. Neurological Sciences 34(5): 765-767.
- Brandao E, Ferreria A, Leal Loureiro J (2013) Anterior biopercular syndrome caused by unilateral infarction. Acta Med Port 26(2): 177179.






























